Replantation of a severed arm in a 5-year-old - Surgical challenges and solutions in pediatric microsurgery: A case report
*Corresponding author: Thi Cao, Department of Orthopedics and Traumatology, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam. caothibacsi@ump.edu.vn
-
Received: ,
Accepted: ,
How to cite this article: Nguyen TN, Nguyen HM, Nguyen PD, Cao T. Replantation of a severed arm in a 5-year-old - Surgical challenges and solutions in pediatric microsurgery: A case report. J Musculoskelet Surg Res. doi: 10.25259/JMSR_119_2025
Abstract
Replantation of a completely severed arm in a child is a highly complex procedure that presents significant technical and physiological challenges. Unlike in adults, pediatric microsurgery involves dealing with smaller anatomical structures, increased vulnerability to ischemic damage, and the need for long-term functional rehabilitation. The success of such a procedure depends on multiple factors, including time from injury to surgery, microsurgical precision, interdisciplinary coordination, and intensive post-operative care. This report details the replantation of a 5-year-old girl’s arm following a traumatic amputation, highlighting the critical surgical challenges and solutions encountered.
Keywords
Children
Growth plate preservation
Limb replantation
Nerve regeneration
Vascular anastomosis
INTRODUCTION
The successful replantation of severed limbs was documented in 1962.[1] Severed arm injuries are relatively rare, particularly in children, and thus, knowledge and expertise are often shared through clinical case studies.[2-4] Similar cases of avulsion-type arm amputations have been reported, such as a 5-year-old boy who underwent successful replantation within 6 h of injury after an amputation caused by a fodder-cutting machine.[2] However, these reported cases have yet to fully demonstrate the entire process from emergency admission to the initial signs of recovery, particularly in instances of avulsion-type arm amputation. What is new in this report is the focus on the unique challenges of managing an avulsion-type arm amputation in a 5-year-old child. Unlike other studies that predominantly focus on more conventional amputation cases, this report emphasizes the specific surgical and post-operative considerations for this type of injury in young children. Notably, while pediatric patients generally exhibit superior neural plasticity and regenerative capacity, achieving optimal recovery remains difficult due to factors such as nerve regeneration speed, post-operative compliance, and the need for specialized rehabilitation.[5,6] In our case, the surgical team employed a refined approach to nerve repair, paying particular attention to preserving neural structures during the replantation procedure.
The child’s enhanced regenerative capacity, along with early intervention and a comprehensive post-operative care plan, contributed to a promising recovery trajectory. However, this case differs from others in that it outlines not only the surgical steps but also the management of post-operative care and functional support, which significantly impacted recovery outcomes. This detailed account provides new insights for junior surgeons, emphasizing the critical role of early referral to a specialized team, timely intervention, and a tailored post-operative care protocol that optimizes functional recovery, particularly in cases of severe avulsion-type amputation.
CASE REPORT
A 5-year-old girl presented to the emergency department 5.5 h after a traumatic amputation of her right arm following a motorbike accident. The child was wearing a one-armed shirt, with the other sleeve not occupied by her arm, which became entangled in the motorbike’s wheel, causing her to be thrown to the ground and resulting in the complete amputation of her right arm. She suffered a complete transection of major neurovascular structures, fractures of the humerus and both forearm bones, along with extensive soft-tissue loss. Specifically, a transverse fracture occurred in the upper third of both forearm bones, while a spiral oblique fracture occurred in the lower third of the right humerus. The triceps brachii, biceps brachii, and brachialis muscles were torn and avulsed in an irregular manner. The radial, ulnar, and median nerves were completely contused, and the brachial artery, along with the major venous structures of the arm, was completely severed. Significant amounts of dirt and sand were embedded within the wound. The case required meticulous planning to optimize replantation success within the limited ischemic time frame.
To maximize efficiency, three surgical teams operated concurrently in two separate rooms. One team performed debridement and fracture fixation using intramedullary K-wires 1.8 mm, another team prepared vascular grafts, and the third focused on revascularization and nerve repair. We conducted a soft-tissue evaluation and observed that after debridement, the muscles retained a pink color and responded to muscle contraction with thermal stimulation. There were no signs of complete tissue damage, and after flushing the vascular lumen post-debridement, the endothelium appeared smooth and pink. Therefore, we decided to proceed with vascular revascularization with shortening and complete grafting. The nerves were severed and crushed, requiring debridement of the radial, ulnar, and median nerve stumps, followed by microsurgical repair using epineural and fascicular techniques with 8.0 nylon sutures. We sutured the muscle with Vicryl 1.0 sutures and the tendon core with nylon 3.0 sutures. Despite successful arterial and venous anastomoses, the 1st post-operative day presented a major challenge: Significant bleeding at the intramedullary nail entry point, necessitating urgent re-exploration. Careful hemostasis was achieved without compromising revascularization, demonstrating the delicate balance required in pediatric microsurgical procedures.
We administered Unasyn 1.5 g intravenously at a dose of 200 mg/kg body weight/day, with intravenous injections every 6 h, in combination with gentamicin 0.08 g at a dose of 1.2 mg/kg/day, intramuscularly every 8 h. The wound condition was monitored daily, along with vital signs. A complete blood count was performed, which showed no signs of post-operative infection. Wound culture and sensitivity testing revealed continued susceptibility to Unasyn and gentamicin, so we decided to continue their use without switching to another antibiotic.
Post-operative follow-up
The patient was supported by the family in daily muscle strengthening exercises. We instructed the family to perform passive range-of-motion exercises for the baby’s shoulder, elbow, and hand, including simple exercises to assist with shoulder abduction and adduction, elbow flexion and extension, wrist flexion and extension, and finger movement. These exercises were to be repeated multiple times a day, with no limitation on the number of repetitions, with monthly radiographs to monitor bone healing during the first 3 months. Bone healing was confirmed to be complete, and all fixation devices were removed in the 8th month. Starting from the 3rd month post-surgery, the patient could flex and extend the elbow, and electromyography (EMG) showed recovery of the radial nerve. By the 4th month, wrist extension was possible. At the 12th month, the patient was able to flex the fingers, but thumb opposition had not yet been achieved [Video 1]. EMG at the 10th month indicated recovery of the median and ulnar nerves.
Video 1:
Video 1:The illustration clip of neurological recovery in the right hand following replantation of the severed arm.The outcome of the patient
At the 12-month follow-up, the patient exhibited significant motor recovery, including wrist and finger extension [Table 1]. However, sensory restoration remained incomplete. This underscores the need for long-term follow-up and rehabilitation, which remains a challenge in pediatric microsurgery due to the geographical and economic barriers many families face.
| Evaluation content | Third Month | Fifth Month | Eighth Month | Tenth Month |
|---|---|---|---|---|
| Clinical Mobility | Able to lift the arm, extend the elbow, and move the wrist | Able to extend the wrist and finger | Able to extend the wrist and fingers | Able to extend the wrist and fingers and gently flex the thumb and index finger. |
| ECG–Radial Nerve | Muscle clumping observed at the brachioradialis muscle at a level of ++ | Severe and incomplete injury, localized at the elbow, at the level where the radial nerve branches to the extensor carpi radialis muscle | Currently, reinnervation is observed for the short abductor of the thumb and the short abductor of the fifth digit, with minimal muscle clumping | Currently, reinnervation is observed for the short abductor of the thumb |
| ECG–Ulnar Nerve | Muscle clumping observed in the ulnar flexor carpi at a level of ++ | Complete injury, localized at the elbow, at the level where the ulnar nerve branches to the flexor carpi ulnaris muscle | Severe but incomplete injury, localized at the elbow, at the level where the ulnar nerve branches to the flexor carpi ulnaris muscle | Severe and incomplete injury, localized at the elbow, at the level where the ulnar nerve branches to the flexor carpi ulnaris muscle and the first dorsal interosseous muscle, with good muscle clumping |
| ECG–Median Nerve | Muscle clumping observed in the pronator teres muscle at a level of ++ | Complete injury, localized at the elbow, at the level where the median nerve branches to the pronator teres muscle | Severe but incomplete injury, localized at the elbow, at the level where the median nerve branches to the pronator teres muscle | Severe but incomplete injury, localized at the elbow, at the level where the median nerve branches to the pronator teres muscle |
ECG: Electrocardiogram
DISCUSSION
Although a report has documented a large number of pediatric cases undergoing replantation and revascularization of the upper extremities,[7] significant challenges in pediatric microsurgery remain. This case involved microsurgical vascular anastomosis for a complex, twisting-type complete traumatic vascular injury, necessitating the primary repair of bones, nerves, and musculotendinous structures. A well-planned surgical strategy was employed to enhance treatment success.
The vascular diameter in a 5-year-old child ranges from approximately 1–2 mm, making the vessels fragile and prone to rupture.[8] In this case, the injury involved a complete avulsion of the upper limb due to traction, leading to significant soft-tissue twisting and extensive damage. The affected blood vessels exhibited intimal disruption due to excessive stretching, necessitating the excision of the damaged segment. End-to-end anastomosis was not a viable option in this scenario.
To resolve this problem, a vascular graft must be prepared in advance to facilitate arterial and venous anastomosis. This preparation should be performed in advance to optimize surgical efficiency and minimize operative time. In this case, while another surgical team performed bone fixation for the forearm, we simultaneously harvested the great saphenous vein from the child’s leg, ensuring it was ready for vascular anastomosis as soon as the bone fixation team completed their procedure [Figure 1].
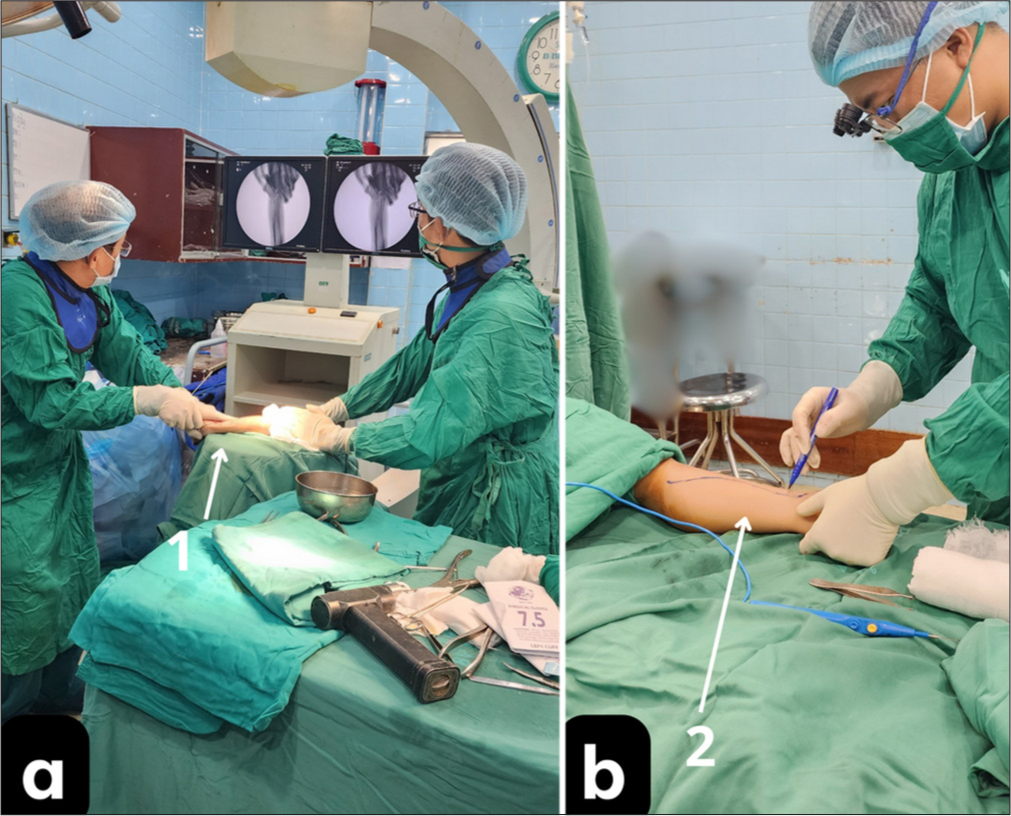
- Two parallel surgical teams in separate operating rooms; (a) forearm bone fixation with intramedullary nailing, 1: forearm positioned on the C-arm machine for manipulation; and (b) harvesting the great saphenous vein for graft preparation, 2: Patient’s lower leg.
Although the ischemic tolerance in children is still unknown, muscle tissue is highly vulnerable to ischemic injury and can suffer irreversible damage. The team prioritized venous anastomosis first to minimize blood loss, rapidly restored arterial circulation, and employed intraoperative monitoring to assess perfusion adequacy. We meticulously irrigated the vessel lumen in this case before performing venous anastomosis. Initially, only one vein was anastomosed, followed by the brachial artery. Blood flow was immediately restored to the most distal part of the hand. The blood overflow from the veins was quickly controlled, allowing us to proceed with the subsequent venous anastomoses [Figure 2].

- Vascular anastomosis for blood reperfusion; (a) Completion of one vein and one artery anastomosis, 1: patent artery, 2: patent vein; and (b) proceeding with the next vein anastomosis, 3: pre-marked location of the vein.
Reperfusion of an ischemic limb can release toxic metabolites into the bloodstream, potentially leading to systemic complications.[9,10] To mitigate this risk, a stepwise revascularization approach was adopted, with close intraoperative monitoring of metabolic markers guiding interventions. In this patient, vital signs remained stable once blood flow was restored. The anesthesia and critical care team closely monitored all parameters and reported no abnormalities. As a result, the outcome was favorable [Figure 3].

- Severed upper arm and microsurgical revascularization. (a) Pre-anastomosis and (b) hand pinking immediately after arterial reperfusion.
In cases of limb detachment, the bones must be stably immobilized. However, growth plate preservation in children is crucial to preventing long-term deformities. Traditional plating methods risk interfering with bone growth.[11] Intramedullary K-wires were selected for their minimal invasiveness and reduced risk of growth disturbance. We used intramedullary K-wires 1.8 mm for both the radius and ulna, as well as two intramedullary K-wires 1.8 mm for humeral fixation [Figure 4].

- X-ray images before and after surgery. (a) Severed upper arm, fractures of both forearm bones; (b) intramedullary nailing of the radius, ulna, and humerus; (c) consolidation of bones showing healing; and (d) bone fixation hardware removed in its entirety.
In children, nerve regeneration occurs at an unpredictable rate, often requiring prolonged therapy.[12] This delay hinders nerve recovery and functional rehabilitation. Epineural and fascicular nerve repair techniques were used to optimize neural regeneration to resolve this problem. In this case, the nerve injury was due to avulsion, making precise alignment during nerve repair more challenging compared to clean-cut nerve transections. We relied on the size of the fascicles and the vascular structures within the nerve trunk to guide the suturing process. Limited access to post-operative rehabilitation services presented a significant challenge. During follow-up, the child lived far from the medical facility and did not undergo physical therapy but continued daily activities as usual. Monthly follow-ups were conducted, and the patient was prescribed 500 mg of calcium, 500 mcg of methylcobalamin, and one tablet daily of cytidine monophosphate disodium 5 mg + uridine monophosphate disodium 3 mg, with the goal of promoting peripheral nerve recovery after neurorrhaphy and alleviating neuropathic pain throughout the recovery period [Figure 5].

- Preparation for microsurgical nerve anastomosis in the arm and post-operative recovery images. (a) Nerve anastomosis preparation after completing vascular anastomosis; (b) right wrist in neutral position; and (c) full extension of the right wrist showing signs of radial nerve recovery.
CONCLUSION
Pediatric limb replantation presents multiple challenges, including anatomical constraints, ischemic vulnerability, and the need for long-term functional rehabilitation. This case highlights the importance of meticulous surgical planning, interdisciplinary collaboration, and post-operative care to optimize outcomes. However, ongoing research into optimizing nerve regeneration and improving access to specialized rehabilitation remains crucial for maximizing long-term success.
Authors’ contributions:
TNN and TC: Concepts, design, definition of intellectual content, literature search, clinical studies, manuscript preparation, and editing. HMTN: Clinical studies, data acquisition; PDN: manuscript preparation and editing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient’s consent:
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for the patient’s images and other clinical information to be reported in the journal. The parents understand that the patient’s name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Conflicts of interest:
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Toka machine injury: Replantation left arm in a 5 year old. Apollo Medicine. 2015;12:50-3.
- [CrossRef] [Google Scholar]
- Pediatric upper extremity replantation. Clin Plast Surg. 2005;32:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric upper extremity replantation: Courage in the face of a life-altering injury. Plastic Reconstr Surg Glob Open. 2018;6:e1766.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term outcomes of arm replantation. Ann Plast Surg. 2020;84:S151-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric replantation after traumatic amputation at the distal forearm: Rehabilitation protocol and outcomes. J Hand Microsurg. 2021;13:169-72.
- [CrossRef] [PubMed] [Google Scholar]
- Results after replantation and revascularization in the upper extremity in children. J Bone Joint Surg Am. 1994;76:1766-76.
- [CrossRef] [PubMed] [Google Scholar]
- Can children be considered for transradial interventions?: Prospective study of sonographic radial artery diameters. Circ Cardiovasc Interv. 2020;13:e009251.
- [CrossRef] [PubMed] [Google Scholar]
- The pathophysiology of skeletal muscle ischemia and the reperfusion syndrome: A review. Cardiovasc Surg. 2002;10:620-30.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms and interventions on acute lower limb ischemia/reperfusion injury: A review and insights from cell to clinical investigations. Ann Vasc Surg. 2022;86:452-81.
- [CrossRef] [PubMed] [Google Scholar]
- Physiology and pathophysiology of the growth plate. Birth Defects Res C Embryo Today. 2003;69:123-43.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical innovations to restore function in pediatric peripheral nerve conditions. Pediatrics. 2021;148:e2021052556.
- [CrossRef] [PubMed] [Google Scholar]







