Translate this page into:
Reuse of orthopedic implants in a peri-implant fracture of both forearm bones in an adolescent: A case report
*Corresponding author: Felipe Aguilar-Chavez, MD Department of Orthopedics, Star Medica, Chihuahua, Mexico. felipemj23@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aguilar-Chavez F, Jorba-Elguero P, Cruz-Cortés M, Gonzalez-Gonzalez F. Reuse of orthopedic implants in a peri-implant fracture of both forearm bones in an adolescent: A case report. J Musculoskelet Surg Res. 2024;8:66-70. doi: 10.25259/JMSR_182_2023
Abstract
Fractures of both forearm bones in adolescents are common. Many of these fractures are surgically fixed with internal fixation. However, among the complications that can occur are peri-implant fractures, which are somewhat infrequent. They are due mainly to high-energy injuries. Therefore, not much information about them is found in the literature. Reusing implants is not a frequent or well-documented practice, and it is carried out only when the necessary resources are unavailable, particularly in developing countries. We are reporting a 16-year-old male patient who suffered a peri-implant fracture distal to plates that were placed 3 years earlier in both left forearm bones. The material was removed successfully and reused, achieving an adequate reduction and fixation with one dynamic compression plate (DCP) plate for the radius and one reconstruction plate for the ulna. The patient recovered successfully. This case report aimed to understand the lack of resources in a developing country and a possible solution for this problem in this type of scenario.
Keywords
Adolescent
Case report
Forearm fracture
Implant reuse
Peri-implant fracture
INTRODUCTION
Fractures of the radial and ulnar diaphysis, commonly known as fractures of both forearm bones, are the third-most common fractures in pediatric patients. Closed reduction followed by immobilization usually results in appropriate healing. These fractures in adolescents (10–16-years-old) can be more challenging to treat due to the lower remodeling potential of these patients.[1] The most typical mechanism of injury is indirect trauma to the forearm, which is responsible for fractures of both bones, generally following a fall on an outstretched hand.[2]
A bone fracture with an existing non-prosthetic implant, such as a plate, nail, or screw, is known as a non-prosthetic peri-implant fracture.[3] Peri-implant fractures can occur after any osteosynthesis. However, there is little information in the literature about peri-implant fractures of both forearm bones in adolescent patients.
We present the case of a 16-year-old patient with a peri-implant fracture of both forearm bones distal to a previous osteosynthesis, which consisted of a radial DCP plate and an ulnar reconstruction plate, which was satisfactorily treated by removal of the material, open reduction, and fixation utilizing the removed plates.
This case report aimed to understand the lack of resources in developing countries and a possible solution for this problem in this type of scenario.
CASE REPORT
A 16-year-old male patient was admitted to the emergency room. He had suffered a fall from a moving motorcycle 10 days before his admission, with direct trauma to the left upper limb causing pain and functional limitation.
The patient was reported to have suffered another motorcycle accident 3 years before. He suffered a moderate brain injury associated with an orbital floor fracture, which was treated conservatively. He had a fracture of the diaphysis of both bones of the left forearm, which required surgical management, with open reduction and internal fixation utilizing a 3.5 mm DCP plate for the radius and a 3.5 mm reconstruction plate for the ulna, which had a satisfactory result, with no complications.
At the time of his arrival at the emergency room, the physical examination revealed a deformity in the middle third of the left forearm. His active and passive hand movements could not be assessed due to pain. There was no distal neurovascular deficit.
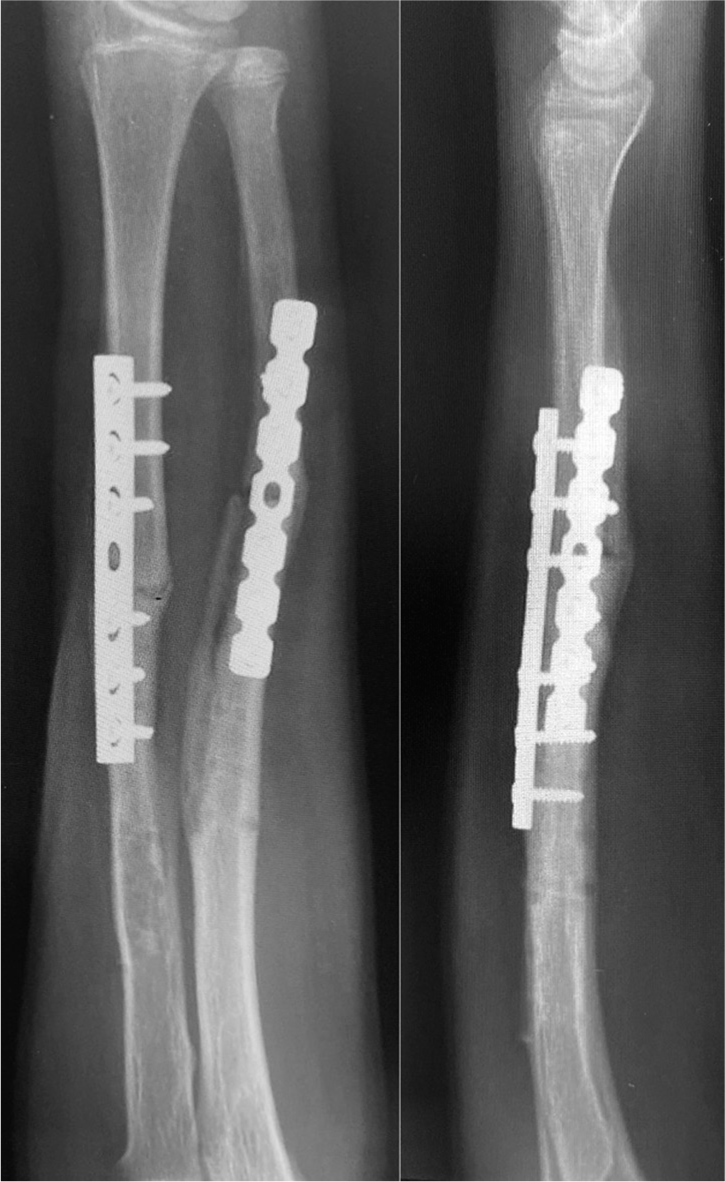
AP and lateral radiographs of the left forearm [Figure 1] showed a simple transverse fracture line in the middle third of the radius and ulna, immediately distal to the previously placed implants in both forearm bones. The plates were intact, without evidence of loosening, and with adequate consolidation of the previous fractures.

- Preoperative AP and lateral views, showing periimplant fracture of both forearm bones.
Due to the lack of implants, surgery was delayed for several days, and the patient was eventually referred to our hospital. Given the risk of malunion, if the surgery was delayed any further, the decision was made to remove and subsequently reuse the previously implanted plates and screws as part of the definitive treatment. Before this, all the requisite hospital safety surgery protocols were meticulously followed, and all necessary documentation and consent forms were duly completed. The patient and his family were informed about the relative risk of further delay of surgery and the high risk of malunion versus the risk inherent to reusing orthopedic implants.
The next day after being admitted to our hospital, the patient was taken to the operating room, where both plates and all screws were removed. After the removal of the implants, the area where the implants were previously placed was examined, with no macroscopic evidence of instability or fracture observed. This was further confirmed through fluoroscopy. Both fractures were exposed, reduced, and fixed in the usual manner, using the same implants that had just been removed, with adequate radiographic and clinical results [Figure 2].

- Immediate postoperative AP and lateral views.
The patient was discharged the day after surgery with a full-arm back slab, without complications, and with only mild pain. He was seen in the outpatient clinic 2 weeks later, where uneventful wound healing was seen, and a full-arm back slab and stitches were removed to initiate active and passive movements without support and weight. He reported no pain then, with mild limitation to full elbow extension with 20° lag and 20° of active pronation [Figure 3].
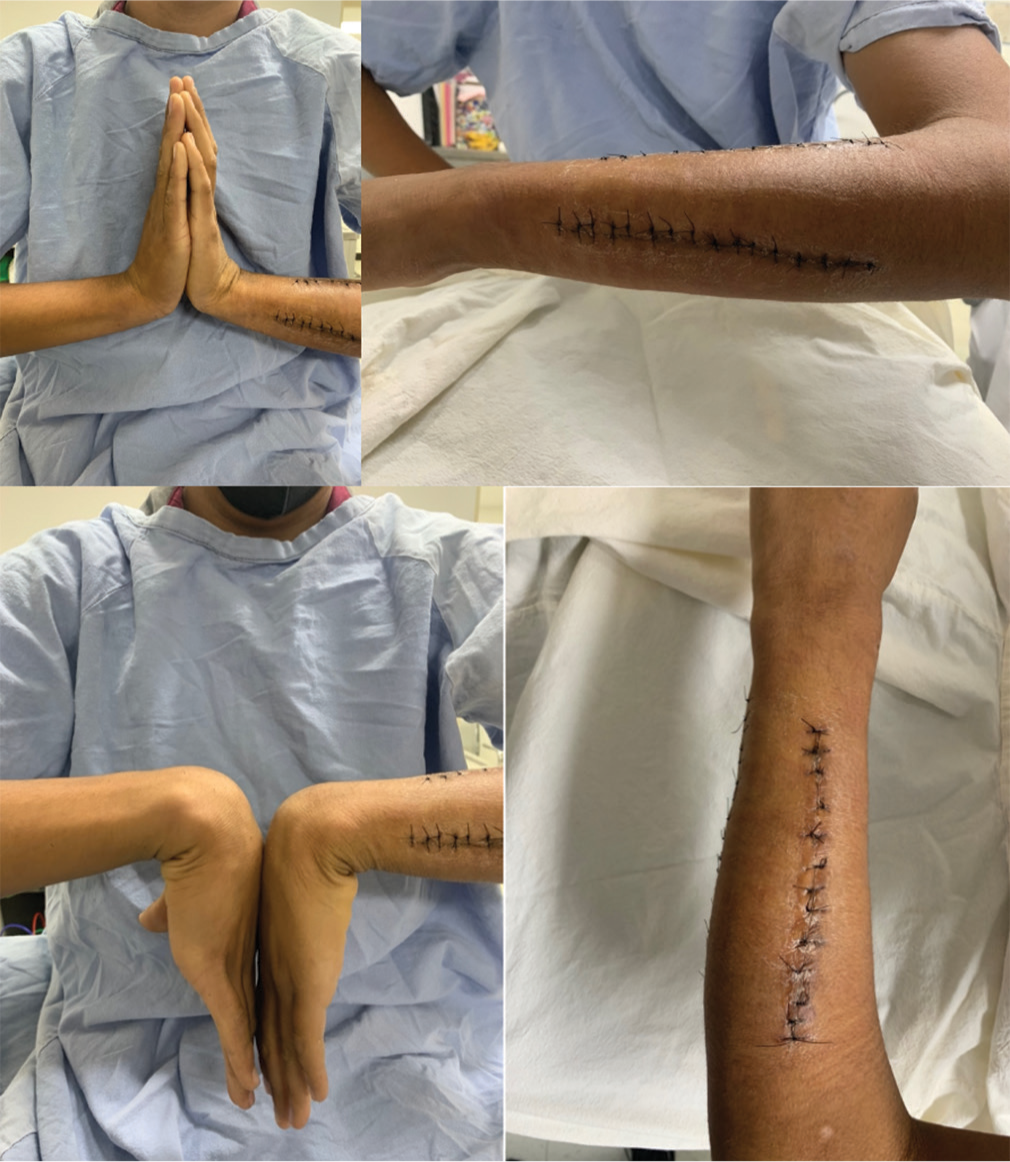
- Active range of movement at 2 weeks after surgery.
The patient was seen 1 month after the procedure, showing marked improvement, with complete motion arc and full strength for all muscle groups. Radiographs were taken, which showed adequate fixation and incipient bony healing. The patient had a complete function 2 months postoperatively, with radiographic evidence of good healing using the RUST score [Figure 4].[4]
- AP and lateral views 2 months after surgery.
DISCUSSION
The treatment of forearm fractures in adults is usually done with open reduction and internal fixation with different types of plates, particularly those that allow interfragmentary compression, due to the propensity to defective consolidation of the radius and ulna and the resulting loss of pronation.[5]
Although there are established surgical indications for conditions like pediatric forearm fractures, which take into account factors like the patient’s age, the extent of angulation, rotation, and the number of remaining growth years, it’s important to note that there is no universally agreed-upon approach to managing and treating fractures. In cases involving children aged 13 or older, where bayonet apposition, angulation exceeding 10°, and a 30° rotation are present, surgical intervention is considered the standard of care.[6] Between 1985 and 1995, the prevalence of invasive surgery as an alternative to closed reduction and cast immobilization grew from 1.8% to 22%.[7]
In contrast to the extensive publications dealing with primary care of forearm fractures in the growing skeleton, neither the incidence nor the proposed management of peri-implant fractures of the middle third of both forearm bones has been addressed in the literature because it is a rare complication that has not been previously reported. The high effectiveness rate and low incidence of complications for this treatment can explain this lack of literature.[8]
Anantavorasakul et al. demonstrated, using a retrospective study of 925 forearm bone fractures in the adult population, that there is a high refracture rate within the first 3 months after removing the osteosynthesis material.[9] Similarly, in the pediatric population, it is estimated that there is a 10.4% incidence of refracture when removing forearm plates.[10]
It is recommended that after the removal of an implant, an orthopedic brace is used, and activity restriction is maintained for 6 weeks in the adult population.[5] However, it has been studied that bone resistance after the removal of a plate in a forearm bone recovers within 3–6 months, being complete in 6 months, emphasizing the degree of recovery of bone atrophy since this varies from one site to another and patients should be careful with refracture after removal.[11] On the other hand, in pediatric patients, Makki et al. recommend not removing the forearm plates before a year after they were placed, and if they plan to remove them within those 12 months, verify the adequate consolidation of the fracture with computed tomography and also place a subsequent immobilization.[10]
Another problem is the delay in surgical procedures, which can be a source of distress to the patient and a reason for poor outcomes. This also is associated with an increased risk of complications.[12]
There is a lack of studies dealing with the reuse of orthopedic implants, which is a problem unique to developing countries, where patients sometimes cannot afford an implant to treat a fracture, and there is often a lack of government-funded health insurance protection.[13] Due to the lack of support in certain circumstances, patients are unable to take advantage of advances related to biomaterials when they are not available and the devastating prospect of a patient needing a new implant and not being able to pay for it leads to reuse of implants as in the case presented above.
The Food and Drug Administration has only issued guidance on reprocessing medical devices in health care but only considers those manufactured for reuse, which leaves out any implant for osteosynthesis.[14] The reuse of orthopedic implants is an understudied and underreported area in the literature. As in many other aspects of medicine in precarious situations, it is advisable to follow lines of research to identify safe and effective management alternatives in these cases.
The absence of follow-up due to patient improvement, as he has not shown up for another visit, is a limitation of this publication.
CONCLUSION
We presented a case of a high-energy peri-implant fracture of both forearm bones in a patient with a plate osteosynthesis history. Both fractures were treated satisfactorily using the previously implanted plates and screws, with good functional results.
In situations of economic disadvantage, where resources for standard surgical treatment are unavailable, the reuse of orthopedic implants can be a reasonable alternative to perform primary osteosynthesis, avoid the complications associated with late surgery, and allow an early return to activities.
AUTHORS’ CONTRIBUTIONS
FA and PJ conceived of the presented idea. FA collected the data and wrote the manuscript with support from PJ, MC and FG reviewed the paper and made corrections with support from FA and PJ All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This publication was approved by the Legaria Children’s Hospital Bioethics Committee ethics board dated August 01, 2023.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s parent has given consent for the publication of the patient’s images and other clinical information in the journal. The parent understands that the patient’s name and initials will not be disclosed, and every effort will be made to conceal their identity. However, complete anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Forearm diaphyseal fractures in the adolescent population: Treatment and management. Eur J Orthop Surg Traumatol. 2015;25:201-9.
- [CrossRef] [PubMed] [Google Scholar]
- The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg. 2013;23:289-96.
- [CrossRef] [PubMed] [Google Scholar]
- Non-prosthetic peri-implant fractures: Classification, management and outcomes. Arch Orthop Trauma Surg. 2018;138:791-802.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of radiographic union scale in tibial fractures and modified radiographic union scale in tibial fractures scores in the evaluation of pediatric forearm fracture union. Jt Dis Relat Surg. 2021;32:185-91.
- [CrossRef] [PubMed] [Google Scholar]
- Management of adult diaphyseal both-bone forearm fractures. J Am Acad Orthop Surg. 2014;22:437-46.
- [CrossRef] [PubMed] [Google Scholar]
- Management of pediatric forearm fractures: What is the best therapeutic choice? A narrative review of the literature. Musculoskelet Surg. 2021;105:225-34.
- [CrossRef] [PubMed] [Google Scholar]
- The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury. 2012;43:362-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-and postoperative complications of adult forearm fractures treated with plate fixation. Orthop Traumatol Surg Res. 2016;102:781-4.
- [CrossRef] [PubMed] [Google Scholar]
- Forearm plate fixation: Should plates be removed? Arch Bone Jt Surg. 2022;10:153-9.
- [Google Scholar]
- Refractures following removal of plates and elastic nails from paediatric forearms. J Pediatr Orthop B. 2014;23:221-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric fractures following implant removal: A systematic review. J Child Orthop. 2022;16:488-97.
- [CrossRef] [PubMed] [Google Scholar]
- Delays in orthopaedic trauma treatment: Setting standards for the time interval between admission and operation. Ann R Coll Surg Engl. 2000;82:322-6.
- [Google Scholar]
- Recovery of forearm bone strength after plate removal: A finite element analysis study. J Hand Surg Am. 2022;16:S0363-5023(22)00460-9.
- [CrossRef] [Google Scholar]
- “Labeling reusable medical devices for reprocessing in health care facilities: FDA reviewer guidance” issued preface public comment. 1996. Available from: https://www.fda.gov/biologicsbloodvaccines/guidancecomplianceregulatoryinformation/guida [Last accessed on 2023 Oct 30]
- [Google Scholar]







