Translate this page into:
Reverse Putti sign in late brachial plexus birth palsy: A case illustration and pathophysiological insights
*Corresponding author: Dr. J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India. terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome JTJ. Reverse Putti sign in late brachial plexus birth palsy: A case illustration and pathophysiological insights. J Musculoskelet Surg Res. 2025;9:266-70. doi: 10.25259/JMSR_341_2024
Abstract
The “Reverse Putti Sign” is a newly identified clinical finding observed in late-stage brachial plexus birth palsy (BPBP), characterized by the superior protrusion of the scapula when the shoulder is adducted and internally rotated. This sign contrasts with the traditional Putti sign, which is associated with glenohumeral abduction contracture and external rotation. The reverse Putti sign suggests a glenohumeral adduction contracture, likely resulting from denervation or weakness of the shoulder adductors, leading to abnormal scapulothoracic motion. This case study highlights the significance of the reverse Putti sign in diagnosing shoulder deformities in BPBP patients, emphasizing the importance of early detection and tailored therapeutic interventions to prevent further complications. Understanding this novel sign broadens the clinical scope for managing BPBP and underscores the complexity of shoulder contractures in these patients.
Keywords
Adduction contracture
Birth palsy
Brachial plexus
Glenohumeral
Putti sign
Reverse
Shoulder
INTRODUCTION
Brachial plexus birth palsy (BPBP) frequently leads to a spectrum of shoulder deformities due to muscle imbalance and denervation.[1,2] These deformities can significantly impact a child’s quality of life, affecting their ability to perform daily activities and potentially leading to long-term functional limitations. While extensive research has focused on the well-known glenohumeral abduction contracture, often associated with the classic “Putti Sign,”[3] glenohumeral adduction contractures remain relatively understudied and poorly understood.[4,5]
Despite their potential impact on shoulder function, glenohumeral adduction contractures have received less attention in the literature, leaving a notable gap in our knowledge of their prevalence, diagnostic criteria, and optimal management strategies.[6,7] This lack of comprehensive understanding highlights the need for new diagnostic tools and a deeper exploration of the underlying mechanisms behind these contractures.
In this context, we introduce the “Reverse Putti Sign,” a newly observed clinical finding characterized by the superior protrusion of the scapula when the shoulder is adducted and internally rotated. This sign, contrasting the traditional Putti sign associated with abduction contractures, may serve as a valuable diagnostic indicator of glenohumeral adduction contracture in late-stage BPBP. Recognizing and understanding this novel sign can pave the way for earlier detection and more targeted interventions, ultimately improving the quality of life for BPBP patients.
CASE REPORT
We present the case of a 5-year-old boy who visited our clinic with a noticeable deformity in his left shoulder. His medical history includes a vacuum-assisted delivery, after which his parents observed weakness in his left upper limb. Clinical photographs at birth demonstrated a classic “policeman tip” posture, characterized by shoulder abduction, internal rotation, forearm pronation, and wrist and finger flexion [Figure 1]. From 3 months of age, the child was managed with an abduction and external rotation brace, and at the time of presentation, he was using an elbow extension splint.

- Sequential images illustrating the patient’s progression from birth to the present condition: (a) Depicts the left shoulder in abduction, with the elbow extended, forearm pronated, and wrist and fingers flexed and ulnar deviated, creating a “policeman’s tip” posture. (b) Shows the application of an abduction and external rotation brace, which was introduced at 3 months of age. (c) Highlights the use of an elbow extension splint, implemented to improve the patient’s left shoulder and upper limb function.
Clinical examination revealed a positive reverse Putti sign, evidenced by superior migration of the scapula during shoulder adduction and internal rotation, which indicates a glenohumeral adduction contracture [Figures 2 and 3]. The child exhibited weak shoulder abduction with a Medical Research Council (MRC) grade of 3/5 and poor triceps function (MRC grade 0). The patient’s modified Mallet score was recorded as follows: Grade II for shoulder abduction, Grade V for external rotation, Grade II for the hand behind the head, Grade II for the hand to the back, and Grade V for the hand to the mouth. Notably, shoulder abduction improved when the elbow was supported in extension [Video]. The forearm, wrist, and hand functions remained intact despite these findings. Ultrasound examination [Figure 4] of the shoulder revealed normal shoulder anatomy with no signs of subluxation, suggesting that the observed contracture might have been a consequence of prolonged use of the abduction and external rotation splint.

- Clinical image showing the absence of the Putti sign during shoulder adduction and internal rotation.

- The reverse putti sign is demonstrated by the superior migration of the scapula during shoulder adduction and internal rotation, indicating a glenohumeral adduction contracture.
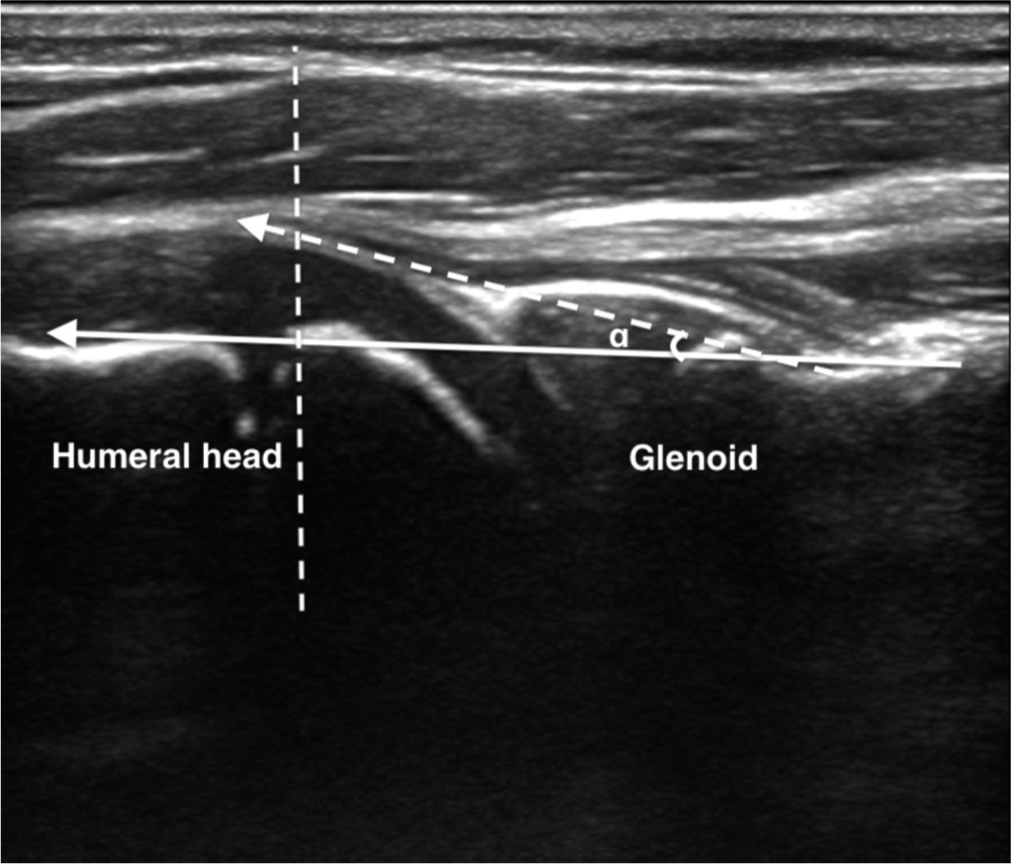
- Ultrasound image of the shoulder demonstrating normal anatomical structures, with no signs of subluxation or other abnormalities. The α angle is formed between the posterior margin of the scapula (solid line arrow) and a line tangential to the posterior humeral head (dotted line).
Pathophysiology of reverse putti sign
One hypothesis is that the supraspinatus and infraspinatus muscles could be structurally affected in a manner similar to the internal rotators, such as the subscapularis. Another possibility is the amyotrophy of all the shoulder’s internal rotator muscles, including the latissimus dorsi, subscapularis, and teres major. In addition, there may be a mild anterior subluxation of the shoulder. These changes might be attributed to secondary abnormal forces around the shoulder joint. As the external rotation of the shoulder becomes more pronounced, the internal rotators lengthen, while the external rotators, such as the rotator cuff muscles and teres minor, shorten. This alteration in muscle length can cause the humeral head to externally rotate and shift anteriorly within the glenoid fossa, changing the line of muscle pull or action line. Such biomechanical alterations could reduce the contraction strength of the internal rotators, even if they are re-innervated.
Imaging studies may reveal abnormal muscle development due to disrupted neural input during the neonatal period. Muscle biopsy studies of the rotator cuff in patients with BPBP may show that the supraspinatus and infraspinatus muscles exhibit shorter slack sarcomere length and increased stiffness compared to healthy muscle. Impaired muscle growth could contribute to the development of muscle contracture and a consequent limitation in shoulder internal rotation.
These changes may be observed in cases involving C6, C7, and C8 brachial plexus injuries, as noted in our case. Such injuries often disrupt neural input to specific muscle groups, leading to abnormal muscle development and biomechanical alterations. In this context, the external rotators may shorten while the internal rotators lengthen, leading to weakened internal rotation and possible anterior subluxation of the shoulder. This muscle imbalance and subsequent contracture contribute to the limitation of shoulder function commonly seen in patients with this type of brachial plexus injury.
Glenohumeral adduction contracture
In the study by Alabau-Rodriguez et al.[7] on glenohumeral adduction contractures in patients with residual neonatal brachial plexus injury, the authors reviewed charts to assess demographic information and the level of palsy using the modified Mallet scale. This approach included only patients older than 4 years to measure both active and passive glenohumeral abduction. The study focused on defining the extent of glenohumeral adduction contracture, with different thresholds (10°, 20°, or 30°) used to compare the affected and unaffected shoulders. A significant finding was that 85% of patients exhibited a contracture >10°, especially among those with C5-C7 or total brachial plexus injuries.
The study provides crucial insights into the prevalence of contractures in this patient population but also highlights a gap in understanding the underlying mechanisms of these contractures, particularly the role of muscle imbalance and denervation. While previous studies have largely focused on glenohumeral abduction contractures (e.g., Gharbaoui et al.),[2] this study sheds light on the less commonly recognized issue of glenohumeral adduction contractures. In addition, the study confirms that shoulder imbalance plays a critical role in developing these contractures, which may not be resolved through isolated glenohumeral releases. This supports the notion that tendon transfers may be essential for improving shoulder function in such cases.
The findings address a significant knowledge gap by demonstrating that glenohumeral adduction contractures are prevalent even in the absence of severe abductor atrophy, a concept not fully explored in prior research. This study emphasizes the need for further investigation into early interventions that balance shoulder musculature to prevent the progression of these contractures, thereby contributing to the broader understanding of shoulder deformities in BPBP patients.
DISCUSSION
Glenohumeral abduction contractures in BPBP are believed to arise from the denervation of the shoulder abductors, commonly seen in C5, 6 injuries. Abduction contractures are frequently observed in patients with residual shoulder dysfunction from neonatal brachial plexus palsy. Interestingly, the abduction contracture does not seem to result from the over-pull of abductors against weak adductors. Instead, the contracture occurs even in the presence of abductor atrophy, independent of adductor atrophy. This finding suggests that denervated muscle shortening contributes to contracture development. Abnormal scapulothoracic movements are a compensatory development to the contractures.
Similarly, we propose that glenohumeral adduction contractures, as evidenced by the reverse Putti sign, may not result from the over-pull of adductors against weak abductors. Instead, they may stem from denervation or weakness of the shoulder adductors, leading to abnormal scapulothoracic motion and a greater contribution of scapular rotation to global shoulder motion. This condition could explain why scapular protrusion is observed during adduction and internal rotation in BPBP patients with adduction contractures.
We did not observe a direct correlation between adduction and external rotation contractures, suggesting that these deformities may result from different combinations of factors, such as muscle imbalance and impaired growth. While other studies have noted a relationship between external rotation contracture severity and glenohumeral dysplasia, our findings do not support a similar correlation with adduction contracture severity.
Surgical interventions aimed at rebalancing the shoulder in BPBP patients, particularly those with shoulder internal rotation contractures, can improve shoulder abduction. However, such procedures do not seem to exacerbate abduction contractures, except in cases with glenoid retroversion. Occasionally, overcorrection during surgery may contribute to developing shoulder adduction contracture and the reverse Putti sign, warranting careful evaluation and management.
The introduction of the Reverse Putti sign, a clinical manifestation of glenohumeral adduction contracture in BPBP, offers valuable insights into the complexity of shoulder deformities in this patient population. Our case report underscores the importance of recognizing atypical presentations and considering a wider spectrum of potential contractures beyond the commonly encountered abduction contracture.
However, it is essential to acknowledge the potential challenges in differentiating the Reverse Putti sign from other clinical signs associated with shoulder dysfunction in BPBP. For instance, the Sprengel deformity, characterized by an elevated scapula, may present with similar visual cues during shoulder adduction. Careful clinical examination, including assessing the range of motion in different planes and evaluating muscle strength, is crucial for accurate diagnosis. In addition, imaging modalities such as radiographs and MRI can help differentiate between bony abnormalities and soft-tissue contractures, aiding in identifying the underlying cause of scapular protrusion.
Our findings resonate with the research by Alabau-Rodriguez et al.,[7] which underscored the prevalence of glenohumeral adduction contractures and their association with shoulder imbalance. Both studies suggest that these contractures are primarily driven by muscle imbalance and denervation rather than the over-pull of specific muscle groups. This understanding challenges the traditional paradigm and necessitates a shift in treatment approaches.
The discovery of the reverse Putti Sign and its link to glenohumeral adduction contractures has the potential to spur the development of novel treatment strategies. Early identification of these contractures through this clinical sign could facilitate timely intervention with targeted physical therapy and rehabilitation programs aimed at restoring muscle balance and preventing further complications. Furthermore, as suggested by Alabau-Rodriguez et al.,[7] surgical interventions like tendon transfers might be considered in cases where conservative management fails to achieve satisfactory outcomes.
CONCLUSION
The reverse Putti sign emerges as a valuable clinical indicator of glenohumeral adduction contracture in BPBP, emphasizing the need for meticulous assessment and personalized treatment plans. Understanding the intricate mechanisms underlying shoulder deformities in BPBP, particularly the roles of muscle denervation and imbalance, is paramount to enhancing patient outcomes.
The recognition and early detection of the reverse Putti sign can potentially revolutionize the management of BPBP. By enabling timely intervention and targeted therapeutic strategies, it has the potential to significantly improve the quality of life for these patients. Enhanced shoulder function and reduced complications can empower individuals with BPBP to engage more fully in daily activities, fostering greater independence and overall well-being.
While further research and clinical observation are necessary to validate these findings and refine treatment approaches, identifying the reverse Putti sign represents a significant step forward in our understanding and management of BPBP-related shoulder deformities. Continued exploration of this novel sign and its implications promises to pave the way for improved care and a brighter future for individuals affected by BPBP.
Ethical approval
Ethical approval was obtained from the OHRC Ethical Committee Board, reference number 30/2024, dated August 2nd, 2024.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient’s parents have given their consent for the patient’s images and other clinical information to be reported in the journal. The parents understand that the patient’s name and initials will not be published, and due efforts will be made to conceal the patient’s identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Glenohumeral abduction contractures after residual neonatal brachial plexus injury. J Hand Surg Eur Vol. 2022;47:243-7.
- [CrossRef] [PubMed] [Google Scholar]
- Perspectives on glenohumeral joint contractures and shoulder dysfunction in children with perinatal brachial plexus palsy. J Hand Ther. 2015;28:176-83. quiz 184
- [CrossRef] [PubMed] [Google Scholar]
- Glenohumeral abduction contracture in children with unresolved neonatal brachial plexus palsy. J Bone Joint Surg Am. 2015;97:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- An obstetric brachial plexus data sheet. J Hand Microsurg. 2009;1:32-8.
- [CrossRef] [PubMed] [Google Scholar]
- Biceps Rerouting after forearm osteotomy: An effective treatment strategy for severe supination deformity in obstetric plexus palsy. J Hand Microsurg. 2017;9:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Complex forearm deformities in brachial plexus birth palsy: Radial head dislocation, forearm bones crossing, and distal ulna volar dislocation. J Musculoskelet Surg Res. 2024;8:403-5.
- [CrossRef] [Google Scholar]
- Glenohumeral adduction contractures with residual neonatal brachial plexus injury. J Hand Surg Eur Vol. 2021;46:432-4.
- [CrossRef] [PubMed] [Google Scholar]






