Translate this page into:
Short-oblique lumbar spine fracture in ankylosing spondylitis patient
Corresponding Author:
Sami I AlEissa
Department of Surgery, King Abdul.Aziz Medical City, Riyadh
Saudi Arabia
saleissa@yahoo.com
| How to cite this article: AlEissa SI, Konbaz FS, AlHelal FH, Abalkhail MS, AlMugren TS. Short-oblique lumbar spine fracture in ankylosing spondylitis patient. J Musculoskelet Surg Res 2019;3:367-369 |
Abstract
Ankylosing spondylitis (AS) is a chronic inflammatory joint disease that mainly causes fusion of the intervertebral discs and facet joints by involving the axial skeleton that typically leads to kyphotic bamboo spine. Demineralization of vertebral bodies in AS raises the risk of spinal fracture even after a simple trauma. During the progression of the disease, the spine becomes more prone to injury, even after minor trauma. Patients with AS have a higher fracture risk during their lifetime by four times compared to the normal population. A 61-year-old male, a known case of AS, came to the emergency room complaining of back pain. His neurological examination was normal, and the images showed transverse/oblique fracture involving L2 vertebral body associated with small retropulsed fragments and bone debris. Posterior spinal fixation and fusion with a bone graft from T10 to S1 was decided to stabilize the fracture. On the 2nd postoperative day, the radiograph showed good alignment and fixation. One-year follow up showed a normal neurological exam with a stable and fused spine. In this case, we present a rare lumbar spine fracture orientation in a patient with AS, with a good outcome with 1-year follow-up. Up to our knowledge, this is the first report to presenting a short-oblique fracture in a patient with AS disease.
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory joint disease that mainly causes fusion of the intervertebral disc and facet joints by involving the axial skeleton that typically leads to kyphotic bamboo spine.[1] AS has a prevalence of 0.1%–1.4% and typically affects male patients between 20 and 30 years of age.[2] The chronic inflammation in AS leads to spontaneous fusion of the bilateral sacroiliac joints and spine leading initially to back pain followed by generalized stiffness of the spine. Demineralization of vertebral bodies in AS raises the spinal fracture risk even after a trivial trauma.[3] During the progression of the disease, the spine becomes more prone to injury, even after minor trauma.[4],[5],[6] Patients with AS have a higher fracture risk during their lifetime by four times compared to the normal population.[7],[8] Fractures in patients with AS can be classified into three types: shearing injury, wedge compression, or pseudarthrosis from chronic nonunion. Shearing injuries are seen in acute trauma and compression fractures with chronic injuries, whereas pseudarthrosis is seen in missed fractures.[9] Extension–distraction fracture pattern is the most common in the thoracolumbar spine of a patient with AS.[10]
Case Report
A 61-year-old male, a known case of AS and hypertension, was admitted to the emergency room in October 2016 for low back pain that started 1 month before and progressed during the last week before presentation. The patient mentioned that he felt a click when moving on the airplane seat a month before. The patient denied any weakness, bowel, or urine obstruction. The pain was relieved by pain killers and rest. On physical examination, the patient had a thoracic kyphosis and tenderness with palpation of the lumbar spine at the level of L2. Sensory and motor neurological examinations were normal. Anteroposterior and lateral radiographs of the lumbar spine showed a bamboo spine (a radiological sign that is typical for AS), with evidence of an oblique fracture involving the body of L2 vertebra [Figure - 1]a and [Figure - 1]b. Computed tomography scan showed transverse/oblique fracture involving L2 vertebral body associated with small retropulsed fragments and bone debris in the surrounding thickened soft tissue, mainly in the right paraspinal lesion [Figure - 2]a and [Figure - 2]b. The patient could not go for magnetic resonance imaging, as he could not stay steady during the examination.
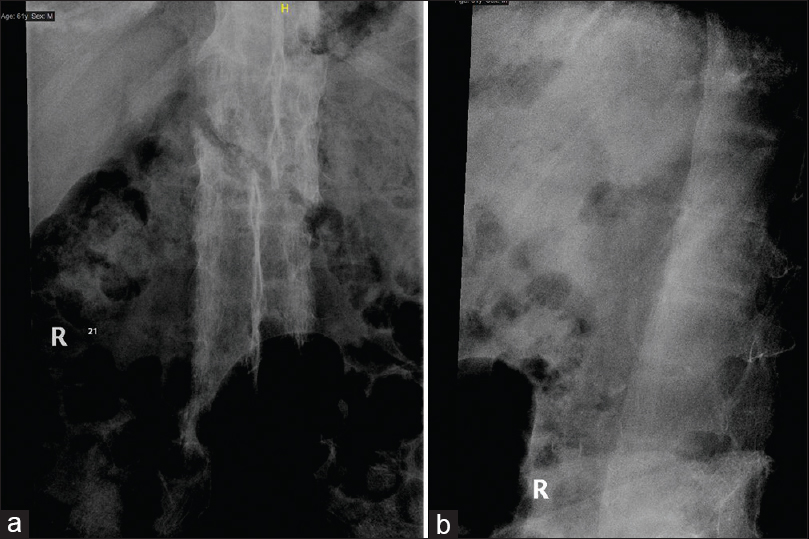 |
| Figure 1: (a and b) Anteroposterior and lateral radiographs of the lumbar spine showing oblique fracture of L2 vertebra |
 |
| Figure 2: (a and b) Computed tomography sagittal and coronal images showing oblique fracture of L2 vertebra |
Since almost any spine fracture in AS patients considered as an unstable fracture (traversing through the three spinal columns), posterior instrumentation from T10 to S1 performed to stabilize the fracture using posterior fixation and fusion with bone graft. The patient was positioned over a Wilson's frame to maintain the kyphosis, and care was taken during positioning to prevent distraction at the fracture site, injury to anterior vascular structures, and anterior gapping. Under both fluoroscopy and navigation guidance, bilateral pedicle screws with appropriate size and length were inserted four levels above up to T10 vertebra and four levels below down to S1 with one left pedicle screw at the fractured vertebra (L2). By utilizing a transpedicular approach on the right side of L2 vertebra to get access to the body, we identified the fracture site. Fracture's edges were refreshed using the curettes and shavers, and then a mesh cage filled with a bone graft was inserted under fluoroscopic guidance. Two rods were inserted, and they were secured to the threaded screws and set screws.
Physiotherapy was started on the 1st postoperative day, and the patient started mobilizing on the same day with a walker frame. Postoperative radiographs were taken on the 2nd day, which showed good alignment and fixation [Figure - 3]a and [Figure - 3]b. The wound was checked on the 3rd day, and the patient was discharged home in a stable condition.
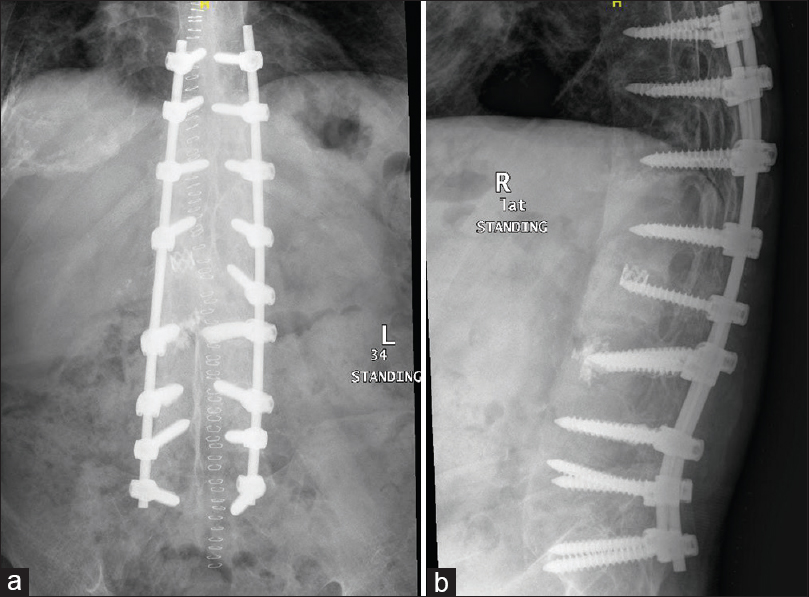 |
| Figure 3: (a and b) Anteroposterior and lateral radiographs of the thoracolumbar spine postoperatively |
The patient was followed up postoperatively in 2 weeks to inspect the wound, which showed good signs of healing. The patient was seen in our clinic 6, 12 weeks postoperatively, when his neurological examination and radiographs were good. One-year postoperatively, the patient came for follow-up, when he was doing fine with no complaints. Physical examination showed intact neurological function, and imaging showed stable and fused fracture with no signs of loosening [Figure - 4]a and [Figure - 4]b.
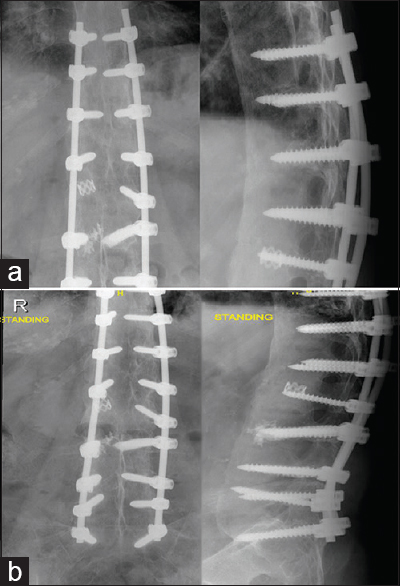 |
| Figure 4: (a and b) Anteroposterior and lateral radiographs of the thoracolumbar spine 1year postoperatively |
Discussion
In patients with AS, the decreased bone mineral density and altered biomechanics of the spine, especially the fusion of functional spine units, increases the incidence of spine fractures.[11] The fused vertebrae from the development of the disease result in a change of the spine's behavior and reaction to any acting forces. Unusually a long-fused spine in AS patient act as a long bone in this situation (one segment), therefore we think that bending with superimposed axial compression forces caused this fracture.
The standard of fixation in AS patients is to go for longer posterior constructs to stabilize spinal fractures, including at least three vertebral levels above and below the fractured vertebra to achieve a good bony apposition that aid in fracture healing, without attempting to reduce the pre-existing deformity.[12],[13],[14]
In our case, the fracture was fixed with four levels above and four levels below to reduce the stress at each level and decrease the pull-out risk. A mesh cage was used with a bone graft after refreshing the fracture edges due to the chronicity of the fracture with the poor bone quality of the patient, and to add stability to anterior column of the spine. Restoration of the anterior column was done through posterior approach without laminectomy, and to achieve a good fixation, a left transpedicular screw to the fractured vertebra was inserted.
In this case, we present a rare lumbar spine fracture orientation in a patient with AS, with a good outcome with 1-year follow-up. Up to our knowledge, this is the first report to presenting a short-oblique fracture in a patient with AS disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
SIA was the primary surgeon, had the first idea to report the case and gave logistic support. FMSQ provided logistic support. FMH did the literature review. MSA wrote the initial draft. TSSM collected the data and helped writing the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Kubiak EN, Moskovich R, Errico TJ, Di Cesare PE. Orthopaedic management of ankylosing spondylitis. J Am Acad Orthop Surg 2005;13:267-78. [Google Scholar] |
| 2. | Braun J, Sieper J. Ankylosing spondylitis. Lancet 2007;369:1379-90. [Google Scholar] |
| 3. | Donnelly S, Doyle DV, Denton A, Rolfe I, McCloskey EV, Spector TD. Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis 1994;53:117-21. [Google Scholar] |
| 4. | Broom MJ, Raycroft JF. Complications of fractures of the cervical spine in ankylosing spondylitis. Spine (Phila Pa 1976) 1988;13:763-6. [Google Scholar] |
| 5. | Hunter T, Dubo HI. Spinal fractures complicating ankylosing spondylitis. A long-term followup study. Arthritis Rheum 1983;26:751-9. [Google Scholar] |
| 6. | Taggard DA, Traynelis VC. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine (Phila Pa 1976) 2000;25:2035-9. [Google Scholar] |
| 7. | Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord 1999;37:444-7. [Google Scholar] |
| 8. | Young JS, Cheshire JE, Pierce JA, Vivian JM. Cervical ankylosis with acute spinal cord injury. Paraplegia 1977;15:133-46. [Google Scholar] |
| 9. | Trent G, Armstrong GW, O'Neil J. Thoracolumbar fractures in ankylosing spondylitis. High-risk injuries. Clin Orthop Relat Res 1988;227:61-6. [Google Scholar] |
| 10. | Chaudhary SB, Hullinger H, Vives MJ. Management of acute spinal fractures in ankylosing spondylitis. ISRN Rheumatol 2011;2011:150484. [Google Scholar] |
| 11. | Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56. [Google Scholar] |
| 12. | Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: A systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976) 2004;29:803-14. [Google Scholar] |
| 13. | Sapkas G, Kateros K, Papadakis SA, Galanakos S, Brilakis E, Machairas G, et al. Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord 2009;10:96. [Google Scholar] |
| 14. | Reinhold M, Knop C, Kneitz C, Disch A. Spine fractures in ankylosing diseases: Recommendations of the spine section of the German society for orthopaedics and trauma (DGOU). Global Spine J 2018;8:56S-68S. [Google Scholar] |
Fulltext Views
1,785
PDF downloads
1,117





