Translate this page into:
Spontaneous union of neglected proximal pole scaphoid fracture: A case report
*Corresponding author: Sherif M. Elnikety, Department of Surgery, College of Medicine and Health Sciences, United Arab Emirates University, Abu Dhabi, United Arab Emirates. elnikety@uaeu.ac.ae
-
Received: ,
Accepted: ,
How to cite this article: Basal HM, Elnikety SM. Spontaneous union of neglected proximal pole scaphoid fracture: A case report. J Musculoskelet Surg Res. doi: 10.25259/JMSR_43_2024
Abstract
Scaphoid fractures are the most common carpal bone fractures and usually occur due to trauma, typically a fall on an outstretched hand. The scaphoid bone is integral to wrist biomechanics, linking the proximal carpal row to the distal row. Neglected scaphoid fractures can lead to significant long-term complications, with degenerative changes likely to occur. The most common consequence of a neglected scaphoid fracture is known as scaphoid non-union advanced collapse, which typically begins within five years following the injury. It is widely accepted that scaphoid fractures, in general, should be treated to avoid long-term complications. Many surgeons aggressively treat proximal pole fractures with surgical fixation due to the high risk of avascular necrosis. Although some surgeons may consider a period of immobilization, none would argue against the need for treatment of proximal pole fractures, either through immobilization or surgical fixation. In this case, we present an instance of spontaneous union of a neglected proximal pole fracture non-union in a mature adult. This report aims to provide awareness of the possible spontaneous union of neglected proximal pole scaphoid fracture. It also challenges the call for acute aggressive surgical intervention in such fractures. Radiographs and magnetic resonance imaging scan images before and after union are presented, along with a review of the available literature.
Keywords
Carpal bone fracture
Neglected fracture
Non-union
Proximal pole
Scaphoid fracture
INTRODUCTION
Scaphoid fractures are common in young patients; they usually happen following a fall on an outstretched hand. They represent up to 7% of all fractures and around 70% of carpal bone fractures.[1,2] These injuries can be easily misdiagnosed initially due to the lack of radiological evidence of a fracture. This misdiagnosis can result in a non-union with a risk as high as 50% if displaced. Scaphoid non-union may lead to progressive wrist arthritis, resulting in a scaphoid non-union advanced collapse if left untreated. The biomechanics of how proximal pole fractures occur are not clear. However, it is thought that the position of the wrist (supination, mid-range, and pronation) may play a role in determining which part of the scaphoid bone is broken.
The majority of injuries are low-energy injuries and tend to occur in young adult men between 15 and 40 years of age. About 10% of these develop non-union. The anatomic location of scaphoid fractures is distributed as 65% waist fractures, 10% distal third, and 25% proximal pole.
Due to the vascularity interruption at anatomic sides, proximal pole fractures have an exceptionally higher rate of non-union and avascular necrosis (AVN). The higher incidence of non-union is due to its unique blood supply pattern. Most of the scaphoid surface is hyaline cartilage. The scaphoid is supplied by the radial artery through dorsal scaphoid branches; these branches penetrate the dorsal scaphoid ridge at the waist and supply 80% of the bone. The volar branches supply the distal 20% at the tubercle. Therefore, the vascular supply is mainly intraosseous blood flow in a retrograde fashion. This unique vascular supply to the proximal pole of the scaphoid explains the higher risk of non-union and AVN. The AVN risk can be as high as 50%. It is exceptionally high in proximal pole fractures.[3] Other risk factors, such as smoking, may add up to a 20% increase in non-union risk.[4]
Non-operative treatment of scaphoid fracture involves immobilization, usually in plaster cast, for a minimum of six weeks and could take up to 24 weeks to achieve union. It is widely accepted that surgical fixation yields better outcomes for displaced fractures to minimize non-union incidence and avoid malunion, which may lead to humpback deformity with limitation of wrist biomechanics. Spontaneous union of scaphoid fracture is extremely rare. However, it has been reported to occur in children in a few studies. This report provides awareness of such cases. However, it is rare, and the treating surgeon needs to have this awareness and arrange adequate investigations as part of the treatment plan to avoid over-treatment of such cases.
CASE REPORT
A 19-year-old man presented to the orthopedic clinic with a history of nine months of left wrist pain. He plays football regularly and has had multiple falls during his games. The last injury was four months before his clinic visit. The patient was fit and well. He is a moderate smoker. During the patient’s evaluation, he was found to have tenderness in the anatomic snuffbox, the scapholunate instability provocative testing such as Watson’s shift test and scapholunate ballottement test were negative, and the wrist joint range of motion was almost the same as the contralateral side. Radiographs were taken, which showed a proximal pole scaphoid fracture non-union and confirmed non-union cyst formation [Figure 1].

- (a) AP and (b) lateral radiographs of the left wrist taken at the first patient encounter confirming evidence of displaced scaphoid fracture.
The wrist was not immobilized, and he had a magnetic resonance imaging (MRI) scan to plan surgical intervention. The MRI was reviewed and confirmed non-union of the proximal pole and non-union with cyst formation at the fracture gap. There was no evidence of AVN of the proximal pole [Figure 2].
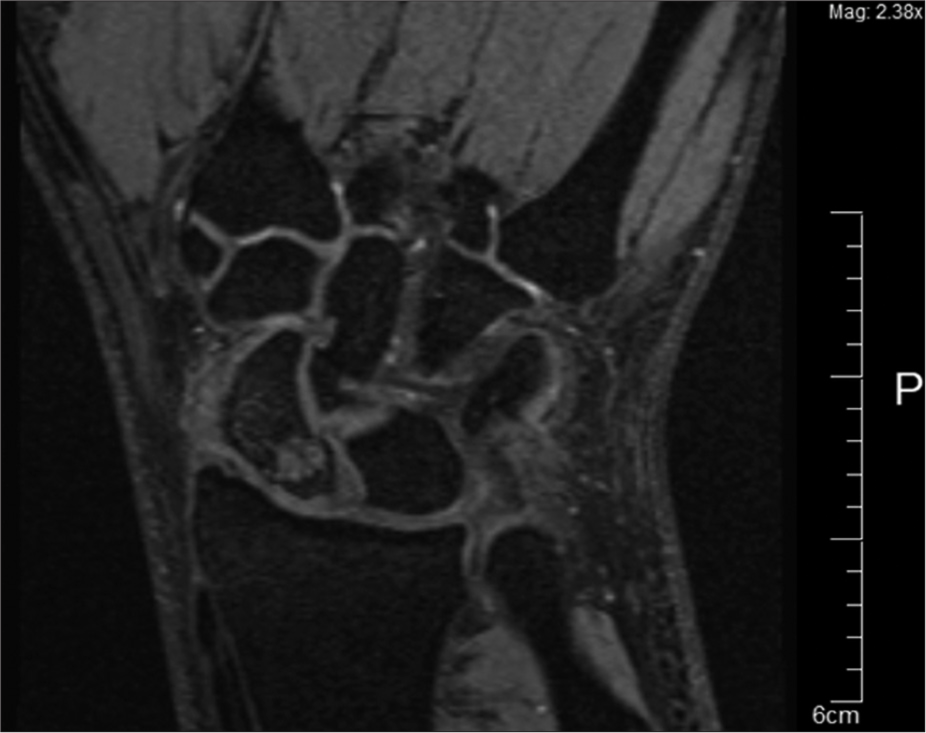
- Magnetic resonance imaging of the left wrist confirming the fracture with cystic changes.
Unfortunately, the patient was lost to follow up for 16 months; during this period, the patient was not seen by any other health-care provider regarding his wrist condition and received no treatment. The fracture was neglected for this period. He returned 16 months later due to persistent pain and limitations. A new radiograph was obtained, which surprisingly showed a significant healing of the fracture [Figure 3]. A full below-the-elbow cast was applied for one month to treat his persistent pain. Further, radiographs were obtained, revealing the fracture’s complete healing. Clinically, the patient was satisfied with the outcome. He returned to his physical exercises, including push-ups, and joined military services without pain or wrist disability. At 12 months follow-up after removing the cast (long gap due to patient non-compliance), an MRI was obtained and revealed complete fracture healing as shown in Figures 4a and b.
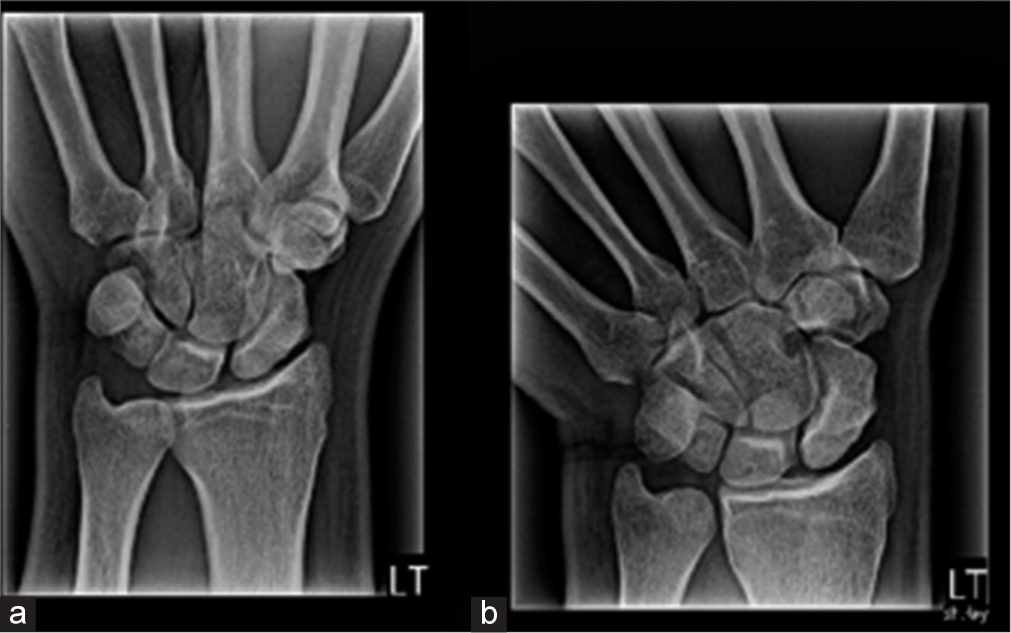
- (a) Oblique and (b) AP radiographs of the left wrist taken 16 months after the first encounter.
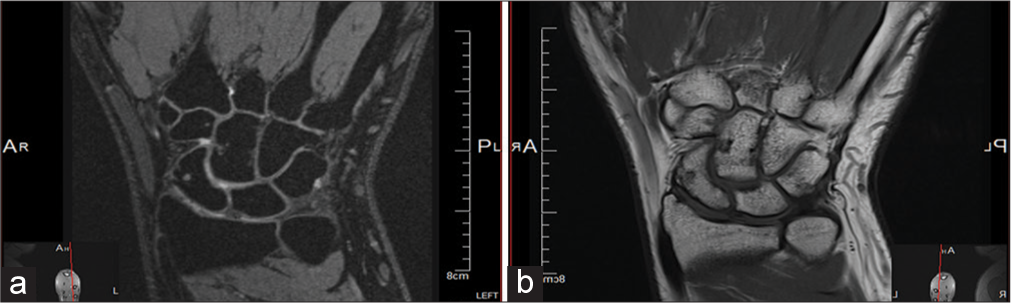
- (a and b) Magnetic resonance imaging taken more than 26 months post initial encounter confirming the complete union of the neglected proximal pole left scaphoid fracture.
DISCUSSION
This case presents a very rare and unexpected outcome where the proximal pole neglected fracture with cystic changes went on to full spontaneous union. It is not clear how this happened. The patient is a young, active smoker, and sustained multiple falls during the time span between the initial injury and fracture union. Union was achieved despite all these factors that are known to delay and prevent bone fracture healing. To the best of our knowledge, only one published report confirms the spontaneous union of a proximal pole fracture in an adult patient. There is a lack of awareness that neglected non-united fractures can achieve spontaneous union without active treatment. This may result in over-treating these fractures. It is widely accepted that treatment immobilization is the non-operative treatment of choice for most scaphoid fractures. Multiple authors advocate operative treatment for proximal pole scaphoid fractures as the first line of treatment to avoid the risk of non-union and AVN complications. In a recently published meta-analysis, authors reported up to 18% of the non-union rate in non-operative treatment of proximal pole fractures (including proximal 1/3rd) against 6% of non-union following operative treatment.[5] Other published studies reported the non-union rate of proximal pole fractures to be as high as 34%.[6] Less aggressive surgeons recommend a trial of immobilization for 6–12 weeks at least before considering surgical fixation. By reviewing a vast body of literature, we found only one case report of the spontaneous union of proximal pole scaphoid fracture non-union without any modality of treatment in an adult patient[7] and another similar case report for a distal pole neglected fracture non-union with spontaneous healing without treatment.[8]
It is widely accepted that proximal pole scaphoid fractures must be treated with strict immobilization or surgical fixation to minimize the higher risk of significant complications.[9,10]
We do not advocate neglecting such fractures. This practice is not recommended due to the clearly higher risk of serious complications. However, our report may strengthen the argument for conservative treatment of such fractures.
CONCLUSION
The majority of proximal pole fracture scaphoid and non-union were recommended early surgical treatment. In very rare situations, spontaneous healing was reported. Nevertheless, this was an exception; we recommend active treatment for proximal pole fracture. The debate remains on whether to consider a period of immobilization or to proceed with surgical fixation as a primary intervention.
AUTHORS’ CONTRIBUTIONS
HHB: Main treating Surgeon, conceived the idea of the report, provided report materials, collected and organized data, and wrote the initial draft. SME: Analyzed and interpreted data, wrote the article’s final draft, and provided logistic support. Both authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Acute scaphoid fractures: Guidelines for diagnosis and treatment. EFORT Open Rev. 2020;5:96-103.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33:423-6.
- [CrossRef] [PubMed] [Google Scholar]
- Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87:2160-8.
- [CrossRef] [PubMed] [Google Scholar]
- Smoking increases failure rate of operation for established non-union of the scaphoid bone. Int Orthop. 2007;31:503-5.
- [CrossRef] [PubMed] [Google Scholar]
- A meta-analysis of union rate after proximal scaphoid fractures: Terminology matters. J Plast Surg Hand Surg. 2022;56:298-309.
- [CrossRef] [PubMed] [Google Scholar]
- Union rates after proximal scaphoid fractures; meta-analyses and review of available evidence. J Hand Surg Eur. 2013;38:888-97.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual case of spontaneous healing of a proximal pole scaphoid non-union. Hand (N Y). 2011;6:313-6.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous healing of a non-union of the scaphoid. J Hand Surg Br. 1998;23:86-7.
- [CrossRef] [PubMed] [Google Scholar]
- Scaphoid fractures and nonunions: Diagnosis and treatment. J Orthop Sci. 2006;11:424-31.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66:114-23.
- [CrossRef] [PubMed] [Google Scholar]






