Translate this page into:
Study of outcome of 300 cases of arthroscopic anterior cruciate ligament reconstruction with quadrupled hamstrings tendon graft using anterior cruciate ligament tightrope for femoral fixation
Corresponding Author:
Sanjay K Rai
Department of Orthopaedics, Naval Hospital, RC Church, Colaba, Mumbai - 400 005, Maharashtra
India
skrai47@yahoo.com
| How to cite this article: Rai SK, Varma R, Wani SS. Study of outcome of 300 cases of arthroscopic anterior cruciate ligament reconstruction with quadrupled hamstrings tendon graft using anterior cruciate ligament tightrope for femoral fixation. J Musculoskelet Surg Res 2018;2:26-30 |
Abstract
Objective: The aim of treatment of tear of the anterior cruciate ligament (ACL) in any military soldiers is to restore normal/near normal stability and function of the knee, preventing further damage to other knee structures and quick return to duty. We studied the functional outcome of arthroscopic-guided ACL reconstruction using quadrupled hamstring tendon graft (QHTG) and femoral side graft fixation using ACL TightRope and also to evaluate its complications. Methods: In this prospective study, evaluation parameters Lachman test, pivot test, and hamstring strength were assessed pre- and post-operatively at 3, 6, 12, 18, and 36 months. Lysholm test was assessed postoperatively. Results: A total of 300 male soldiers with a mean age of 26.5 years were evaluated. Injury due to military training, sports, fall, and road traffic accident was a common cause. Preoperatively, all patients had a positive pivot and anterior drawer tests, 4+ score of Lachman test, and 4/5 muscle strength with restriction of movement to <10°. Mean ± standard deviation Lysholm score at 3, 6, and 12 months were 81.19 ± 10.21, 83.86 ± 12.44, and 89.17 ± 8.32, respectively. At the 3rd month, negative Lachman test was seen in 83.6% (251/300) of patients, 13.6% (41/300) had 1+ laxity, and 2.6% (8/300) patients had 2+ laxity. None had positive pivot shift test. At 3 and 12 months, 91.3% (274/300) and 100% (300/300) had a grade of 5/5 power in hamstring muscles. Fifteen cases developed postoperative complications such as infection and graft failure. Conclusion: Autologous ipsilateral QHTG is a near anatomical and good choice for ACL reconstruction and is associated with fewer complications.Introduction
Anterior cruciate ligament (ACL) tears are very commonly seen in military soldiers of any country because of the heavy involvement either in active combat, military training, or in sports. Anterior knee instability associated with rupture of ACL is a disabling clinical condition, especially for young soldiers. Surgical reconstruction of ACL injuries is required to reduce pain, maintain stability, limit further loss in the joint structure, and function and early return to duty. Untreated torn ACL will result in progressive symptomatic instability leading to recurrent injury, damage to the menisci, articular cartilage, and early osteoarthritis.[1],[2]
The treatment option for ACL tear is solely surgical, and reconstruction of the ACL is very crucial in maintaining the structural and functional stability of the joint movement and maintains the static and dynamic equilibrium of knee joint.
Hamstring or patellar tendon autografts are preferred as the chances of rejection are minimal. Problems with extensor mechanism of the knee, loss of motion, patellar fracture, and development of chronic anterior knee pain with the bone-patellar-tendon-bone autograft, prompted surgeons to seek other graft materials for use in ACL reconstruction. Semitendinosus and gracilis (Hamstring) tendon represent an alternative autograft donor material that is used for ACL reconstruction to overcome the postoperative issues associated with a patellar tendon graft.[3]
The main aim for early ACL reconstruction is to restore normal or near normal stability in the knee, restore the level of function, limit the loss of joint function, prevent further injury or more damage to other knee structures, and early return to work.
The aim of this study is assessing the functional outcome of arthroscopic-guided ACL reconstruction using quadrupled hamstring tendon graft (QHTG) and femoral side graft fixation using ACL TightRope and evaluate its complications.
Materials and Methods
This prospective study was conducted by the Department of Orthopedics, Jalandher hospital, Punjab, India, and Naval Hospital, Colaba, Mumbai, 400005, India, from September 2010 to December 2015 after obtaining Institutional Ethics Committee's approval.
All patients who were young soldiers, aged 19–40 years, with a history of repeated and episodic knee instability, without evidence of clinical or radiological degenerative changes in the knee joint, and underwent arthroscopic-guided ACL reconstruction using QHTG (Semitendinosus and Gracilis) were included in the study. The diagnosis was confirmed radiologically, which included an X-ray and magnetic resonance imaging (MRI) scan.
Inclusion criteria
ACL tear with or without meniscus tear within 9-month postinjury.
Exclusion criteria
- Patients with ACL tear in the age groups <19 and above 40 years
- Partial tear of ACL
- ACL tear older than 9 months
- Posterior cruciate ligament tear
- Bilateral ACL ruptures
- ACL tears with associated injuries of tibial or femoral condyles
- ACL tear with tricompartmental osteoarthritis of knee joint
- Revision ACL reconstructions were excluded from the study.
Preoperatively, all patients underwent preanesthesia checkup and were accepted as American Society of Anesthesiologists Grade 1.
Ligament laxity was assessed using Lachman's test (0–4+ grades),[4] anterior drawer's test,[5] and pivot shift test.[6] The range of motion of the operated knee was noted and compared with the contralateral knee. Knee flexion strength (hamstring power) was assessed using Medical Research Council (MRC) grading muscle power after harvesting the semitendinosus and gracilis tendon graft.[7]
Majority of the patients (206) were operated by a single surgeon, and remaining patients (94) were operated along with another surgeon (co-author). All patients were operated in supine position under spinal anesthesia. First, semitendinosus and gracilis hamstring tendon was harvested, and quadrupled graft was prepared and kept under tension. ACL tear was confirmed by arthroscopic evaluation; partial meniscectomy was done if a large tear was found, we did not repair any meniscus in our study as all tears were in mid-substance and in the avascular area. If any associated chondral lesion, osteoarthritic changes were seen or chondromalacia patella was detected during arthroscopic evaluation; such patients were excluded from the study. Femoral and tibial tunnels were made using the standard technique.
We tried to keep tibial tunnel exit position in the posteromedial portion of the ACL footprint also to keep the tibial tunnel inclined posteriorly toward the Blumensaat's line on a full extension to prevent graft-notch impingement. After deciding these points, the ACL tibial guide was set to an angle of 55° and placed medial to the center of the remaining tibial stump of the native ACL through an anteromedial portal just medial to the patellar tendon. The guide wire was then passed, and the tibial tunnel was created with a cannulated drill.
The femoral tunnel was positioned with the 7- or 8-mm “over the top” femoral guide and a guide wire with eyelet was passed through an anteromedial portal. The knee was then hyperflexed at up to 120°–130° before drilling the lateral femoral condyle. The center of the tunnel was marked depending on the graft size (normally 8–9 mm diameter and 25-mm depth), and a remaining posterior wall of 2–3 mm was recommended. This femoral insertion site represents an anatomical position between the anatomical anteromedial and posterolateral tunnel positions at the 2 o'clock position on a left knee and the 10 o'clock position on a right knee. After passing the graft in both tibial and femoral tunnels, the femoral end was fixed by flipping the ACL TightRope endobutton. After securing femoral end graft end was held, and about 25–30 cycles of knee movement were done (flexion/extension) then tibial end was secured with a bioabsorbable screw by keeping knee flexed at 30°. Finally, isometry, graft tension, and graft impingement were tested.
Postoperatively, intravenous Teicoplanin 400 mg once daily for 2 days was given, and the suture was removed on 14 days. Postoperative ACL rehabilitation protocol was followed for all patients.
All patients were evaluated at an interval of 3, 6, 12, 18, and 36 months to assess their progress. The standard protocol of Lysholm knee scoring system was used for the evaluation of the results of surgery during follow-up. Subjective and objective evaluations were performed; latter included ligament laxity (assessed using Lachman's test, anterior drawer's test, and pivot shift test), comparison of a range of motion of the operated knee with the contralateral knee, and knee flexion strength (hamstring power, assessed using MRC grading).
All patients were subjected to four phases (I–IV) of intense rehabilitation,[8] starting from 3rd postoperative day till 4–8 months, to restore the function and stability of the joint, gait, pain reduction, and restore and enhance the strength and endurance through active physiotherapy.
This was a time-bound clinical study. Data were captured on Microsoft Excel worksheet and analyzed. Descriptive statistics, frequency tables, mean, standard deviation (SD), and percentage were used to portray the results.
Results
Three hundred patients were included in the study; all underwent unilateral arthroscopic ACL reconstruction using hamstring autograft. All patients completed their follow-up visit at 3, 6, 12, 18, and 36 months.
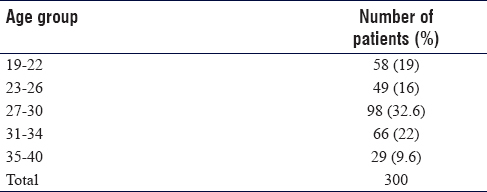
All patients were young male in the study, with an average age of 26.5 (19-40) years [Table - 1].
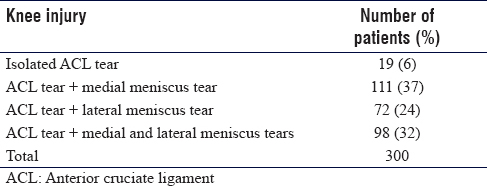
The right knee was affected in 234/300 (78%) patients, and the left knee was affected in 66/300 (22%) patients. Only 19/300 (6%) patients in our study had isolated ACL tears, and the rest had associated meniscal injuries [Table - 2].
Preoperatively, all participants had a positive anterior drawer and pivot test, 4+ score of Lachman test. All patients had 4/5 muscle strength, and the limitation of the range of motion in all patients was <10°.
The mean ± SD Lysholm score at 3, 6, 12, 18, and 36 months was 86.11 ± 9.21, 87.86 ± 12.40, 91.67 ± 7.32, 98.19 ± 3.53, and 98.25 ± 2.17, respectively.
At 3-month follow-up, all 300 (100%) patients had negative anterior drawer test and had negative Lachman test. At 6 months, three (1%) patients had 1+ laxity, and only two patients had 2 + laxity. At the 12th month, Lachman test was negative in 295 (98%) patients [Table - 3].
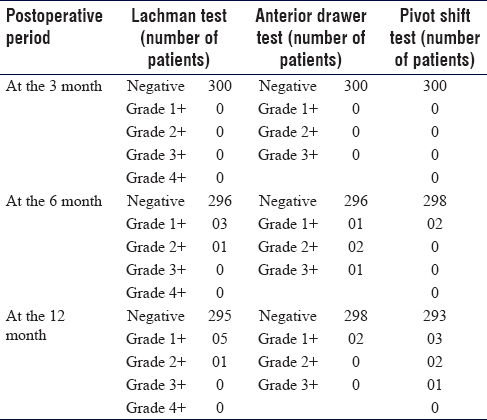
Lachman test, anterior drawer, and pivot shift test postoperatively at the 18th month was the same as the 12th month.
289 patients regained full range of movement at the end of the 18th month. However, among 300 patients, only 289 patients were available for followed-up until 3 years, the other eleven patients lost follow-up because of change of their posting place. Among the 289 patients, all had negative Lachman, and none had positive pivot shift test.
At the 1st year, ten patients had Grade 1 laxity. Five patients had grade 1 Lachman, two patients had Grade 1 anterior drawer, and three patients had positive pivot shift.
These patients at 1-year follow-up had no instability while walking or during activities such as running or climbing up and down stairs.
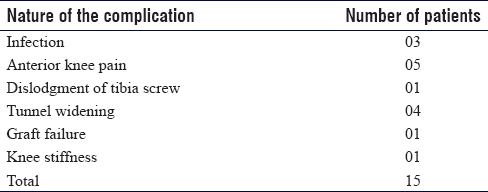
At 3-month follow-up, 129 patients (43%) had a 5/5 grade (MRC) power in hamstring muscles, and in 171 patients (54%) had a 4/5 grade power. Postoperative complications were seen in 15 patients; anterior knee pain (5/300), tunnel widening (4/300), and infection (3/300 were the frequent complications, which were managed accordingly [Table - 4].
Discussion
Reconstruction of ACL tear has been performed with various structures, of which hamstrings offers advantages because of anatomical position and strong structure, faster recovery, less pain with joint movements, and cosmetically, it is more acceptable to the patient. The studies have recommended this procedure,[9] it is the most adopted technique, and the application of this procedure is increasing.
All patients were men in most of the studies [10] have documented male preponderance though females are at a higher risk.[11] In our study, the mean age was 26.5 years. It could be attributed to the active involvement of this age group in sports activities; it may also be attributed to the riding of two wheelers for commuting in the study region.
Sports and trauma are the well-established and documented causes of ACL tears. Military training and sports accounted for 76% patients in our study. All soldiers had unilateral ACL, and the incidence of associated medial meniscal tears was more than the lateral meniscus tears the current study. Associated meniscal injuries were seen in the other studies as well,[12] but unlike our patients, the lateral meniscal injuries (46.88%) were more frequent in them.[13]
In our study, all soldiers had a positive pivot and anterior drawer test, and Lachman score of 4+ indicating complete ACL tear clinically, further confirmed by MRI. All patients had decreased muscle strength (4/5) and range of movement (<10°) before surgery, which improved subsequently postsurgery.
We have used Lysholm test for subjective evaluation of ACL reconstruction. Our study has documented a gradual increase in the score from 88.17 to 98.58, indicating improvement. The previous studies also documented similar observations of improvement in Lysholm score postoperatively.[14]
Lachman test is the most sensitive maneuver for eliciting the ACL tear in an acute setting, when the knee is swollen and painful, in which considerable knee motion is painful to be tolerated. We have operated on acute ACL tears after 10–14 days of injury once the acute phase has subsided. All patients had 4+ score before surgery and negative in 98.3% of patients at 1-year follow-up.
All our patients had decreased, or restricted range of movement preoperatively, and a full range of motion was attained in all patients after 3 months of surgery because of supervised physiotherapy. Postoperatively, six patients in our study had positive pivot shift.
There was a significant improvement in hamstring muscle strength at long-term follow-up with good rehabilitation program even after both the tendons were used for the graft.
We did not observe a significant difference in the Lachman score, hamstring test, and range of motion after 12 months of follow-up.
The usual complications of ACL reconstruction are DVT, infection, bleeding, injury to nerves and/or vessels, graft failure, swelling, pain, instability, knee stiffness, hamstring-related issues, and foreign body reactions secondary to screws and buttons. Superficial infection was the most common postoperative complication seen in various studies. Studies have noted less anterior knee pain with the use of hamstrings graft compared to bone patella tendon graft.[15]
Harvesting of hamstring (semitendinosus and gracilis) tendon weakened the ACL agonists, which resulted in initial less hamstring power and also mild laxity patterns in the initial 6 months of the postoperative period. Regaining hamstring power negated the mild laxity pattern in the postoperative follow-up period. Knee stability was restored postoperatively in our soldiers, and they all resumed their military duty.
Anterior knee pain (1%) and tunnel widening (1%) were more frequently reported complications in our patients. In five patients, pain over the anterior part of the leg persisted up to 8 months postoperatively; the reason could not be found out in our patients. We managed this pain with nonsteroidal anti-inflammatory drugs and physiotherapy. Heijne et al. have concluded that mild anterior knee pain is associated with good clinical outcome.[16]
In the study by Nag and Gupta, it was shown that ACL fixation with ACL TightRope has a good result with minor complications.[17] Wise et al.[18] showed that variable loop button is better than fixed loop button, which also supports our outcome of surgery.
Graft failure was noted in only one patient; however, we have managed him with relook arthroscopy and regrafted him after 3 months, and this soldier has shown improvement over 1 year.
In our study, we observed that the proximal femoral ACL TightRope (Arthrex, USA) and distal bioabsorbable interference screw provided good primary ACL graft fixation, which enabled immediate negation of anterior drawer and pivot shift tests and hence is one of the good choices for ACL graft fixation.
Conclusion
ACL TightRope is an excellent femoral side graft fixation device, which provides an option for further tightening the graft even after the tibial end fixation is done if the surgeon feels it is needed. We can now conclude that autologous ipsilateral quadrupled hamstring tendon graft is a good graft choice in arthroscopic ACL reconstruction and graft fixation using ACL TightRope for the femoral end fixation and bioabsorbable interference screw fixation at the tibial end give an excellent result with minor complications. This implant has adjustable length loops that can be tightened intraoperatively. This property of ACL TightRope makes it a better and a robust fixation device. ACL rehabilitation protocol concentrating on regaining hamstring power is essential to the success of ACL reconstruction surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author contributions
SKR-Senior surgeon, concept and design of work, the acquisition and interpretative of data. RV-Surgeon and analysis of data. SSW-Surgeon and statistical analysis. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | McGinty JB. Arthroscopic surgery in sports injuries. Orthop Clin North Am 1980;11:787-99. [Google Scholar] |
| 2. | Arnold JA, Coker TP, Heaton LM, Park JP, Harris WD. Natural history of anterior cruciate tears. Am J Sports Med 1979;7:305-13. [Google Scholar] |
| 3. | Rowden NJ, Sher D, Rogers GJ, Schindhelm K. Anterior cruciate ligament graft fixation. Initial comparison of patellar tendon and semitendinosus autografts in young fresh cadavers. Am J Sports Med 1997;25:472-8. [Google Scholar] |
| 4. | Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 1976;4:84-93. [Google Scholar] |
| 5. | Slocum DB, James SL, Larson RL, Singer KM. Clinical test for anterolateral rotary instability of the knee. Clin Orthop Relat Res 1976;118:63-9. [Google Scholar] |
| 6. | Galway HR, MacIntosh DL. The lateral pivot shift: A symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 1980;147:45-50. [Google Scholar] |
| 7. | Magee DJ, editor. Principles and concepts. In: Orthopaedic Physical Assessment. 2nd ed. Philadelphia: W. B. Saunders Co.; 1992. p. 1-33. [Google Scholar] |
| 8. | Williams JS Jr., Bach BR Jr. Operative and nonoperative rehabilitation of the ACL injured knee. Sports Med Arthrosc Rev 1996;4:69-147. [Google Scholar] |
| 9. | Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: A comprehensive review of current literature and systematic review of clinical results. Arthroscopy 2015;31:541-54. [Google Scholar] |
| 10. | Kubiak G, Fabiś J. Evaluation of treatment strategy of acute knee infection after ACL reconstruction with hamstring. Pol Orthop Traumatol 2013;78:235-8. [Google Scholar] |
| 11. | Torn W. ACL. Emedicine Health. Available from: http://www. Emedicinehealth.com/torn_acl/page4_em.htm. [Last updated on 2015 Jul 30; Last accessed on 2016 Jan 25]. [Google Scholar] |
| 12. | Ali MS, Kumar A, Adnaan Ali S, Hislop T. Anterior cruciate ligament reconstruction using hamstring tendon graft without detachment of the tibial insertion. Arch Orthop Trauma Surg 2006;126:644-8. [Google Scholar] |
| 13. | Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M, et al. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: Differences and similarities. Am J Sports Med 2005;33:1337-45. [Google Scholar] |
| 14. | Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med 1999;27:444-54. [Google Scholar] |
| 15. | Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH, et al. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: A prospective comparative study with 9-year follow-up. Arthroscopy 2011;27:653-65. [Google Scholar] |
| 16. | Heijne A, Ang BO, Werner S. Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scand J Med Sci Sports 2009;19:842-9. [Google Scholar] |
| 17. | Nag HL, Gupta H. Seating of tightRope RT button under direct arthroscopic visualization in anterior cruciate ligament reconstruction to prevent potential complications. Arthrosc Tech 2012;1:e83-5. [Google Scholar] |
| 18. | Wise BT, Patel NN, Wier G, Labib SA. Outcomes of ACL reconstruction with fixed versus variable loop button fixation. Orthopedics 2017;40:e275-e280. [Google Scholar] |
Fulltext Views
3,885
PDF downloads
449





