Subvastus approach improves intraoperative patellofemoral tracking in total knee arthroplasty for varus deformities – An in vivo study
*Corresponding author: Mohamed Elkabbani, Department of Orthopedic Surgery, Mansoura University, Mansoura, Egypt. mohamedalkappany@mans.edu.eg
-
Received: ,
Accepted: ,
How to cite this article: Elkabbani M, Adi M, Osman A, Khater A, Tarabichi S, Zaghloul A. Subvastus approach improves intraoperative patellofemoral tracking in total knee arthroplasty for varus deformities – An in vivo study. J Musculoskelet Surg Res. 2024;8:368-74. doi: 10.25259/JMSR_170_2024
Abstract
Objectives:
The subvastus approach has the theoretical advantages of protecting the extensor mechanism while securing the patellar blood supply, enhanced patellofemoral tracking, faster recovery, decreased post-operative pain, and shortened length of hospital stay at the expense of longer operative and tourniquet times. This study aimed to evaluate the effect of the subvastus approach on patellofemoral tracking. We hypothesize that being a more anatomical approach, the subvastus approach may improve patellofemoral tracking intraoperatively and decrease the necessity to release the lateral retinaculum during total knee replacement (TKR).
Methods:
In 54 consecutive cases presented with advanced varus osteoarthritis knee in a high-volume arthroplasty hospital from January 2022 to April 2022 and scheduled for cemented posterior stabilized TKR, patellofemoral tracking and the tightness of lateral retinaculum were evaluated intra-operatively all through the whole range of motion (ROM) of the knee by “No thumb test” and “Vertical patella test” subsequent doing the whole tibial and femoral bony cuts, proper sizing, completing soft-tissue release and gap balancing, and reaching the full ROM.
Results:
The “No thumb test” and “Vertical patella test” were negative in all the patients, and there was no intra-operative dislocation or subluxation. In addition, there was no need to release the lateral retinaculum in any of them.
Conclusion:
Implementing the subvastus approach during TKR surgeries, with subsequent preservation of the patellar attachment of the vastus medialis oblique muscle, allows for better tracking of the patella over the femur during surgery, resulting in a reduction in the necessity of performing lateral retinaculum release intraoperatively.
Keywords
Patellofemoral tracking
Subvastus approach
Total knee arthroplasty
Total knee replacement
Varus osteoarthritis
INTRODUCTION
Total knee replacement (TKR) is considered a standard solution with good long-term outcomes for managing end-stage knee osteoarthritis (OA).[1] However, one in five patients is still dissatisfied with their outcomes following TKR.[2-5] Patellar complications account for 10% of these poor results.[6] Post-operative knee pain, especially anterior knee pain (AKP), remains the commonest trigger of patient disappointment following TKR.
AKP is reported in cases with and without patellar replacement.[7-10] Hence, whether or not to resurface the patella remains controversial in TKR.[11-13] The exact cause of AKP is still not well known, as neither patella denervation nor patellar replacement can eliminate AKP.[14-16] Patellofemoral maltracking is another key player. Patellar tracking can be affected by many factors, such as the morphology and alignment of the native patella, surgical technique, implant design, rotational alignment of tibial and femoral implants, component positioning, and pre-existing patellar tracking.[17-21]
Therefore, appropriate patellar alignment and tracking are of ultimate significance in improving the results and patient-reported outcome measures after TKR.[22-26] After all, attaining adequate patellar tracking is crucial while performing TKR. Any intra-operative patellar-tracking problem noted acts as a red flag and must prompt the surgeons to re-evaluate each component’s position and soft-tissue balance.[27-30] In literature, multiple intraoperative methods have been described to evaluate patellofemoral tracking and lateral retinaculum tightness while performing TKR such as: “No thumb test,” “Towel clip test” and “Vertical patella test.”[31,32]
Another critical point in this issue is the approach used in TKR. Various surgical approaches have been described since the advent of the conventional medial parapatellar approach in 1874.[33] The subvastus approach - detailed by Erkes in 1929 and popularized by Hofmann et al. in 1991[34,35] – has the advantages of conserving the quadriceps mechanism and improving patellar tracking.[36-39]
The purpose of the current work was to evaluate the effects of using the subvastus approach on patellofemoral tracking. We hypothesize that, as a more anatomical approach, the subvastus approach may improve intraoperative patellofemoral tracking and decrease the need for releasing lateral retinaculum during TKR.
MATERIALS AND METHODS
In 54 consecutive cases presented with advanced varus OA knee in a high-volume arthroplasty hospital from January 2022 to April 2022 and scheduled for cemented posterior stabilized TKR, patellofemoral tracking and the tightness of lateral retinaculum were evaluated intraoperatively all through the whole range of motion (ROM) of the knee by “No thumb test” and “Vertical patella test” subsequent doing the whole tibial and femoral bony cuts, proper sizing, completing soft-tissue release and gap balancing, and reaching the full ROM. The assessment was done twice: the first while utilizing trial components and the second after the cementation of final implants. The patellae were not resurfaced in any of these cases.
All patients with varus deformities of more than 15°, flexion deformities of more than 10°, and previous knee surgeries were excluded. Demographic data regarding age, sex, and body mass index (BMI) were documented. In addition, data concerning present history and medical co-morbidities utilizing the American Society of Anesthesiologists (ASA) physical status were documented. Clinical evaluation was done for all patients preoperatively. Radiographic evaluation was done through standing anteroposterior and lateral radiographs utilizing Thienpont and Parvizi Classification[40] and Insall–Salvati ratio.[41] Informed consent was attained from all potential candidates before surgery.
The surgery was performed in accordance with the protocol for cemented posterior stabilized TKR in our institution. The entire procedures were performed by one high-volume TKR surgeon through the same subvastus approach [Figures 1 and 2] and using cemented posterior stabilized TKR “Zimmer Persona System.”
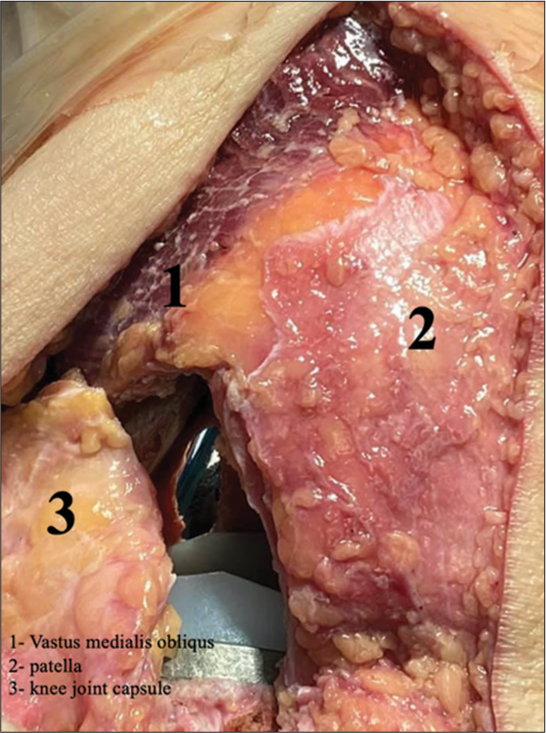
- Exposure and arthrotomy.
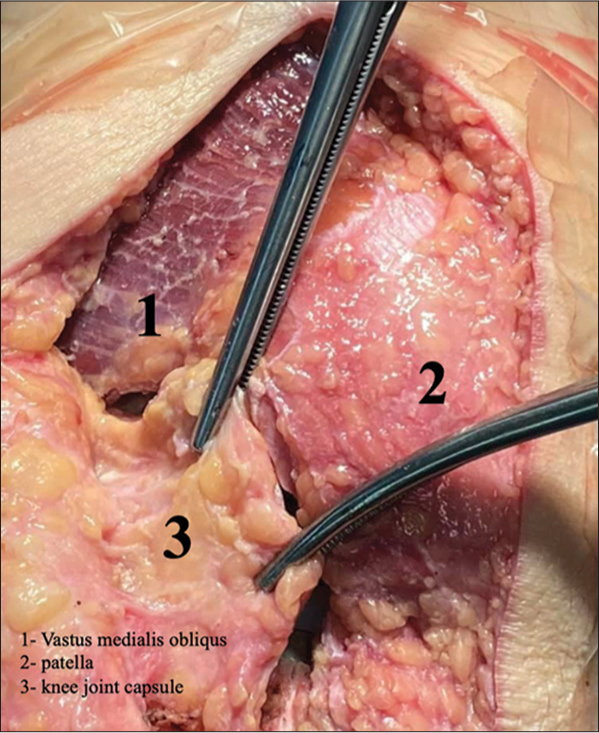
- Closure with intact vastus medialis oblique muscle.
Through a midline skin incision, full-thickness medial and lateral flaps are created sharply with careful hemostasis till exposure of vastus medialis oblique (VMO) muscle insertion. Using blunt dissection, a finger is placed under the inferior border of the VMO muscle which is then retracted proximally and laterally while maintaining its attachment to the patella. A capsular incision is then made just distal to the VMO muscle, taking care to leave a cuff of tissue attached to the patella for closure and not to injure the medial collateral ligament. Synovial attachments to the undersurface of the quadriceps tendon in the suprapatellar pouch are released completely from medial to lateral to allow mobilization of the extensor mechanism. The release of soft-tissue proximal to the patellar tendon all the way to the lateral edge of the tibial plateau is performed, including retropatellar pad fat, intermeniscal ligament, and anterior horn of the lateral meniscus. The patella can now be subluxed into the lateral gutter using a 90°-bent Hohman retractor while flexing the knee with subsequent exposure of the entire joint.
A measured resection technique was applied with a 9-mm distal femoral cut, and a 5° valgus angle was performed using the intramedullary femoral guide. An anterior reference sizing guide was used to determine the anteroposterior size of the femoral implant and adjust the external rotation of femoral components based on the mean rotation of the trans epicondylar axis and the axis at a right angle to the Whiteside’s line.
The tibial cuts were performed utilizing the extramedullary guide with 3° of a posterior tibial slope followed by tibial component sizing using tibial symmetrical trials. After performing femoral notch cuts, soft-tissue balancing, including sequential medial releases, was performed and then the properly sized trial components were used. In all patients, the curve-on-curve technique was utilized to adjust the rotation of the tibial components.
The “No thumb test” was performed by flexing the knee without applying force by the operator’s thumb to block lateral patellar subluxation. In cases with proper patellar tracking, the patella maintains contact with the medial femoral condyle all through the ROM; any elevation of the medial edge, subluxation, or dislocation of the patella represents a positive test.
The “Vertical patella test” was performed using a towel clip to evert the patella to 90° respecting the femoral component while the knee is extended and then trying to translate it medially so that its lateral border passes beyond the middle of the intercondylar groove of the femoral component while the patella is in an everted position. A positive test means the inability to do this.
Data was analyzed using the Statistical Package for the Social Sciences (SPSS) software, version 25 (SPSS Inc., PASW Statistics for Windows version 25. Chicago: SPSS Inc.,). The description of qualitative data was in numbers and percentages and that of quantitative data was in median (minimum and maximum) for non-normally distributed data and mean ± Standard deviation for normally distributed data following the evaluation of normality utilizing the Kolmogorov–Smirnov test. The judgment of the significance of the results obtained was calculated at the (0.05) level.
RESULTS
The current study included 40 females (74%) and 14 males (26%). Their mean age was 54.85 ± 3.88 years, and their mean BMI was 30.1 ± 3.9 kg/m2. Details of demographic data and ASA score are listed in Table 1. The mean varus deformity of the included cases was 7.9° ± 3.5 and the mean flexion deformity was 4.9° ± 3. Details of clinical evaluation are documented in Table 2. The mean Insall–Salvati ratio of the included cases was 1.17 ± 0.15 and data regarding radiographic evaluation are summarized in Table 3.
| Demographic data and ASA score | |
|---|---|
| Age (years) mean±SD | 54.85±3.88 |
| Sex number (%) | |
| Male | 14 (25.9) |
| Female | 40 (74.1) |
| BMI (kg/m2) mean±SD | 30.12±3.92 |
| ASA score number (%) | |
| 1 | 27 (50) |
| 2 | 21 (38.9) |
| 3 | 6 (11.1) |
BMI: Body mass index, ASA: American Society of Anesthesiologists, SD: Standard deviation
| Clinical evaluation | Number | Percentage |
|---|---|---|
| Varus deformity (degrees) | ||
| 5 | 29 | 53.7 |
| 10 | 19 | 35.2 |
| 15 | 6 | 11.1 |
| Flexion deformity (degrees) | ||
| 0 | 10 | 18.5 |
| 5 | 35 | 64.8 |
| 10 | 9 | 16.7 |
| Radiographic evaluation | |
|---|---|
| Thienpont and Parvizi classification: n(%) | |
| IA -AMOA IA -PMOA IA -Fixed varus without lateral laxity IA -Fixed varus with lateral laxity |
15 (27.8) 29 (53.7) 6 (11.1) 4 (7.4) |
| Insall–Salvati ratio (Mean±SD) | 1.17±0.15 |
IA: Intra-articular, AMOA: Anteromedial osteoarthritis, PMOA: Posteromedial osteoarthritis, SD: Standard deviation
The “No thumb test” and “Vertical patella test” were negative in all the patients with no intraoperative dislocation or subluxation. In addition, the release of lateral retinaculum was not needed in any of them. The mean operative time was 102.8 ± 13.1 min. The details of the implant sizes are summarized in Table 4.
| Implant size | Number | Percentage |
|---|---|---|
| Femoral component | ||
| D | 17 | 31.5 |
| E | 20 | 37 |
| F | 9 | 16.7 |
| G | 8 | 14.8 |
| Articular surface | ||
| 10 | 28 | 51.8 |
| 12 | 23 | 42.6 |
| 14 | 3 | 5.6 |
| Tibial component | ||
| 2 | 4 | 7.4 |
| 3 | 15 | 27.8 |
| 4 | 18 | 33.3 |
| 5 | 14 | 25.9 |
| Stem extension | 9 | 16.7 |
DISCUSSION
Adequate patellofemoral tracking and precise component alignment are the core points of TKR to achieve a well-functioning knee with high patient satisfaction.[42] Patellar maltracking causes multiple complications ranging from AKP, restricted ROM, and instability up to frank dislocation.[43]
In literature, multiple intraoperative methods have been described to evaluate patellar tracking as well as lateral retinaculum tightness while performing TKR, such as the “No thumb test” and “Towel clip test”.
Lately, Goyal et al. proposed another test, the “Vertical patella test.” A reliable and simple method was to evaluate lateral retinaculum tightness and assess patellar tracking. They found a high correlation between the “Vertical patella test” and the “Towel clip test” where the “Vertical patella test” was positive in 86% of cases with positive “Towel clip test.” In addition, they concluded that the “Vertical patella test” may be more specific and should be used in addition to the currently used “No thumb” and “Towel clip” tests.[32]
In a study by Verma and Lalchandani on 100 consecutive primary TKAs utilizing posterior stabilized implants, the “Towel clip test” and “Vertical patella test” were positive in 8 and 10 cases, respectively. They documented a good correlation between the results of both tests and recommended their use intraoperatively, as the “Vertical patella test” validates the results of the “Towel clip test” and gives more confidence to surgeons about patellar tracking and the need for lateral retinacular release.[31]
As regard the approach, the subvastus approach has the benefits of preserving the quadriceps mechanism with conservation of the blood supply of the patella, better patellofemoral tracking, faster recovery, reduced postoperative pain, and shorter hospital stays with early mobilization at the expense of longer operative and tourniquet times and bounded exposure when utilized for complex cases.[36-39]
Lateral retinacular release represents one of many well-described options for dealing with patellofemoral maltracking during surgery. The literature has documented it as being utilized in 3.8–45% of cases undergoing TKR.[31] However, this release could precipitate a wide range of complications, including attenuation of patellar blood supply,[44,45] wound healing problems,[28] and symptomatic subluxation of the soft-tissue defect over the femoral component.[46] In addition, it may be associated with increased blood loss and wound healing complications.[28] Accordingly, with these possible problems, decreasing the need and knowing the appropriate indications for such release are critical. In the current study, lateral retinaculum release was not needed in any case with proper intraoperative patellar tracking in all patients.
In 200 consecutive primary TKRs, Archibek et al. reported a positive “No thumb test” and a positive “Towel clip test” in 39% and 6.5% of cases, respectively. They concluded that the “No thumb test” had a high rate of false positives that overpredict the need for retinacular release. They recommended using the “Towel clip test” to determine the necessity for the lateral retinaculum release.[47] In another study by Laskin, utilizing the “Towel clip test,” the lateral retinaculum release rate was 6% in 178 cases.[48] In addition, Fetto et al. reported a reduction in the lateral retinaculum release rate after using an electronic pressure sensing instrument for soft-tissue balancing in 99 TKRs, compared with 100 cases before its use.[49]
On the contrary, the current study showed a negative “No thumb test” in addition to the “Vertical patella test” in all patients with no need for the use of the “Towel clip test.” This work had more than a few limitations. Aside from the small sample size, valgus knees were not included, as the soft-tissue procedures and cases with severe varus or flexion deformities were completely different. We believe that balancing these cases will affect our evaluation of the efficacy of maintaining the VMO muscle attachment to the patella in normalizing patellar tracking. Another limitation is the absence of clinical correlation, as this was an intra-operative study without post-operative follow-up, and other studies should cover this point.
CONCLUSION
As the latest literature has not added any notable change to modify current clinical practice in improving patellofemoral tracking after TKR, we believe that conserving the VMO muscle attachment to the patella by utilizing the subvastus approach betters the intraoperative – and consequently the post-operative – patellofemoral tracking and diminishes the necessity to release the lateral patellar retinaculum in TKR surgeries.
RECOMMENDATIONS
Considering the study’s findings, the subvastus approach may improve patellofemoral tracking and patient satisfaction while avoiding the hazards of performing lateral retinacular release. Further research is encouraged to investigate the patellofemoral kinematics with different knee prosthesis designs for refining approaches and follow-up of clinical outcomes.
ACKNOWLEDGMENT
This research abstract was presented as a free paper at the 43rd SICOT Orthopedic World Congress, which was held from November 21 to 23, 2023, in Cairo, Egypt.
AUTHORS’ CONTRIBUTIONS
ME and ST generated the concept, performed the literature search, prepared the manuscript, and reviewed it. MA and AO contributed by defining the intellectual content, searching for literature, and preparing and editing manuscripts. AZ, AK, and ME contributed by editing and reviewing manuscripts. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study was approved by the Institutional Review Board at Burjeel Hospital for Advanced Surgery, Dubai, UAE. number E10028, dated May 15, 2020.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients consented to their images and other clinical information reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that no artificial intelligence (AI)- assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- What factors drive inpatient satisfaction after knee arthroplasty? J Arthroplasty. 2017;32:1769-72.
- [CrossRef] [PubMed] [Google Scholar]
- What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty. 1996;11:831-40.
- [CrossRef] [PubMed] [Google Scholar]
- Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262-7.
- [CrossRef] [PubMed] [Google Scholar]
- Patient-based outcome analysis is important to determine the success of total knee arthroplasty: Result of a focus group discussion. Med Devices (Auckl). 2016;9:125-30.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019;105:S43-51.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of femoral implant design modification on anterior knee pain and patellar crepitus in patients who underwent total knee arthroplasty without patella resurfacing. BMC Musculoskelet Disord. 2020;21:364.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar denervation does not reduce post-operative anterior knee pain after primary total knee arthroplasty with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc. 2021;29:3346-51.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar denervation reduces postoperative anterior knee pain after patellar resurfacing total knee arthroplasty: A randomized controlled trial. J Arthroplasty. 2021;36:1295-301.
- [CrossRef] [Google Scholar]
- Different factors conduct anterior knee pain following primary total knee arthroplasty: A systematic review and meta-analysis. J Arthroplasty. 2018;33:1962-71.e3.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar resurfacing does not improve clinical outcome in patients with symptomatic tricompartmental knee osteoarthritis. An RCT study of 40 patients receiving primary cruciate retaining total knee arthroplasty. J Knee Surg. 2021;34:1503-9.
- [CrossRef] [PubMed] [Google Scholar]
- Total knee replacement without patellar resurfacing: About 60 cases. Pan Afr Med J. 2020;36:132.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of patellar resurfacing versus preservation in high flexion total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:1782-90.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar denervation with electrocautery reduces anterior knee pain within 1 year after total knee arthroplasty: A meta-analysis of randomized controlled trials. Orthop Surg. 2021;13:14-27.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar resurfacing as a second stage procedure for persistent anterior knee pain after primary total knee arthroplasty. Int Orthop. 2012;36:1181-3.
- [CrossRef] [PubMed] [Google Scholar]
- To resurface or not to resurface the patella in total knee arthroplasty. Clin Orthop Relat Res. 2008;466:2775-83.
- [CrossRef] [PubMed] [Google Scholar]
- The painful knee after total knee arthroplasty: Evaluation and management. Acta Biomed. 2017;88:60-7.
- [Google Scholar]
- Anterior knee pain after total knee arthroplasty: A narrative review. Int Orthop. 2014;38:319-28.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc. 2014;22:2599-607.
- [CrossRef] [PubMed] [Google Scholar]
- Stress distribution of the patellofemoral joint in the anatomic V-shape and curved dome-shape femoral component: A comparison of resurfaced and unresurfaced patellae. Knee Surg Sports Traumatol Arthrosc. 2017;25:263-71.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of patellar morphology classified by Wiberg classification on knee joint function and patellofemoral tracking after total knee arthroplasty without patellar resurfacing. J Arthroplasty. 2021;36:3148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Patellar tilt and subluxation in total knee arthroplasty. Relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;286:103-9.
- [CrossRef] [Google Scholar]
- Patella position is not a determinant for anterior knee pain 10 years after balanced gap total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:2656-62.
- [CrossRef] [PubMed] [Google Scholar]
- Suboptimal patellofemoral alignment is associated with poor clinical outcome scores after primary total knee arthroplasty. Arch Orthop Trauma Surg. 2019;139:249-54.
- [CrossRef] [PubMed] [Google Scholar]
- Kinematic aligned femoral rotation leads to greater patella tilt but similar clinical outcomes when compared to traditional femoral component rotation in total knee arthroplasty. A propensity score matched study. Knee Surg Sports Traumatol Arthrosc. 2021;29:1059-66.
- [CrossRef] [PubMed] [Google Scholar]
- Tibial tubercle-trochlear groove distance influences patellar tilt after total knee arthroplasty. J Arthroplasty. 2019;34:3080-7.
- [CrossRef] [PubMed] [Google Scholar]
- The intraoperative assessment of patellar tracking In: Scuderi GR, Tria AJ, eds. Surgical techniques in total knee arthroplasty. New York: Springer; 2002. p. :317-25.
- [CrossRef] [Google Scholar]
- Lateral patellar release in knee arthroplasty. Effect on wound healing. J Arthroplasty. 1992;7:427-31.
- [CrossRef] [PubMed] [Google Scholar]
- The total condylar knee prosthesis: The first 5 years. Clin Orthop Relat Res. 1979;145:68-77.
- [CrossRef] [Google Scholar]
- Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg. 2009;17:766-74.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective comparative study of intraoperative “Towel clip test” and “Vertical patella test” assessing lateral retinaculum tightness in patients undergoing TKR. J Clin Orthop Trauma. 2019;10:995-8.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing patellar tracking during total knee arthroplasty: A technical note. Am J Orthop (Belle Mead NJ). 2012;41:450-1.
- [Google Scholar]
- Further experiences with physiological incision to open the knee joint. Bruns Beitr Klin Chir. 1929;147:221-32.
- [Google Scholar]
- Subvastus (Southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res. 1991;269:70-7.
- [CrossRef] [Google Scholar]
- Minimally invasive knee arthroplasty with the subvastus approach allows rapid rehabilitation: A prospective, biomechanical and observational study. J Phys Ther Sci. 2013;25:557-62.
- [CrossRef] [PubMed] [Google Scholar]
- Faster quadriceps recovery with the far medial subvastus approach in minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21:2370-4.
- [CrossRef] [PubMed] [Google Scholar]
- Subvastus versus medial parapatellar approach in total knee arthroplasty: Meta-analysis. Orthopedics. 2012;35:e1722-31.
- [CrossRef] [PubMed] [Google Scholar]
- Early patient outcomes after primary total knee arthroplasty with Quadriceps-Sparing subvastus and medial parapatellar techniques: A randomized, double-blind clinical trial. J Bone Joint Surg Am. 2014;96:907-15.
- [CrossRef] [PubMed] [Google Scholar]
- A new classification for the varus knee. J Arthroplasty. 2016;31:2156-60.
- [CrossRef] [PubMed] [Google Scholar]
- Patella position in the normal knee joint. Radiology. 1971;101:101-4.
- [CrossRef] [PubMed] [Google Scholar]
- A technique of staged lateral release to correct patellar tracking in total knee arthroplasty. J Arthroplasty. 2009;24:735-42.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical technique: Lateral retinaculum release in knee arthroplasty using a stepwise, outside-in technique. Clin Orthop Relat Res. 2012;470:2854-63.
- [CrossRef] [PubMed] [Google Scholar]
- Scintigraphic determination of patellar viability after excision of infrapatellar fat pad and/or lateral retinacular release in total knee arthroplasty. Clin Orthop Relat Res. 1990;260:10-6.
- [CrossRef] [Google Scholar]
- Clinical, roentgenographic, and scintigraphic results after interruption of the superior lateral genicular artery during total knee arthroplasty. Clin Orthop Relat Res. 1989;248:145-51.
- [CrossRef] [Google Scholar]
- A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12:322-31.
- [CrossRef] [PubMed] [Google Scholar]
- Indications for lateral retinacular release in total knee replacement. Clin Orthop Relat Res. 2003;414:157-61.
- [CrossRef] [PubMed] [Google Scholar]
- Lateral release rates after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:88-93.
- [CrossRef] [PubMed] [Google Scholar]
- Electronic measurement of soft-tissue balancing reduces lateral releases in total knee arthroplasty. Bull NYU Hosp Jt Dis. 2011;69:285-8.
- [Google Scholar]






