Translate this page into:
Surgical technique for collateral ligament avulsion fractures of the proximal interphalangeal joint with a rotated bony fragment
*Corresponding author: Dr. J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India. terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome T. Surgical technique for collateral ligament avulsion fractures of the proximal interphalangeal joint with a rotated bony fragment. J Musculoskelet Surg Res. doi: 10.25259/JMSR_533_2024
Abstract
Collateral ligament avulsion fractures of the proximal interphalangeal (PIP) joint, particularly those with a rotated bony fragment, can lead to chronic instability and functional impairment. While many avulsion fractures can be managed conservatively, a subset with significant displacement and fragment rotation requires surgical intervention. This technical note describes a surgical technique using Kirschner wire fixation for managing displaced collateral ligament avulsion fractures with a rotated bony fragment involving the volar plate of the PIP joint. The technique is illustrated through a detailed case presentation and further supported by a brief discussion of four additional cases with similar injury patterns and successful outcomes.
Keywords
Avulsion fracture
Collateral ligament
Instability
Proximal interphalangeal joint
Surgical technique
Volar plate
INTRODUCTION
Displaced collateral ligament (CL) avulsion fractures of the proximal interphalangeal (PIP) joint, particularly those with a rotated bony fragment, present a unique challenge in hand surgery. These injuries, often caused by a combination of hyperextension and rotatory forces, can result in joint incongruity, joint instability, and long-term functional limitations if not appropriately addressed.[1,2] While many small and minimally displaced CL avulsion fractures can be treated conservatively with splinting or buddy taping, fractures with significant displacement, particularly those with a bony fragment rotated 90° such that its articular surface faces the fracture site at the base of the middle phalanx, often require surgical intervention to restore joint stability and congruity.[1]
While traditional methods like screw fixation may be suitable for larger avulsion fragments, managing small, rotated bony fragments associated with CL injuries requires careful consideration.[1] Attempting screw fixation in these small fragments can lead to complications such as fragment comminution or further instability, potentially necessitating more complex reconstruction procedures.[1,2]
This technical note describes a surgical technique utilizing Kirschner wire (K-wire) fixation for managing this specific subset of challenging injuries. The technique aims to achieve stable anatomical reduction of the rotated bony fragment, indirectly reducing and stabilizing the associated volar plate and CL, and facilitating early mobilization. Our technique addresses the limitations of traditional methods by providing a simple, minimally invasive, and effective solution for these complex PIP joint injuries. A detailed case presentation illustrates the technical nuances of the procedure, followed by a brief overview of four additional cases demonstrating the effectiveness of this approach.
INDICATIONS
Displaced CL avulsion fractures of the PIP joint with a bony fragment rotated 90°, such that its articular surface faces the fracture site at the base of the middle phalanx, resulting in joint incongruity.
Volar plate avulsion fractures associated with the above CL injury, where the fragment is small and not amenable to screw fixation.
CONTRAINDICATIONS
Non-displaced or minimally displaced and non-rotated CL avulsion fractures, even with associated volar plate injuries. These injuries are often managed successfully with conservative treatment (splinting and buddy taping).
Isolated volar plate avulsion fractures without a concomitant displaced and rotated CL avulsion fracture. These may be amenable to conservative treatment, fragment excision, or screw fixation if the fragment is large enough.
Significant articular comminution or bone loss precluding stable K-wire fixation of the avulsed fragment.
Open fractures or significant soft tissue injury requiring staged management or more complex soft tissue reconstruction.
SURGICAL ANATOMY
The PIP joint is a complex structure stabilized by CLs and a volar plate, functioning as a box-like unit to resist displacement.[3] The injury occurs through a two-plane disruption, typically hyperextension and rotation, causing the CL and volar plate avulsion from the middle phalanx base. The intact accessory CL prevents complete dislocation. Both CLs may be injured in severe cases, leading to volar PIP joint dislocation and potential central slip injury.[3]
TECHNICAL ASPECTS
Patient position and anesthesia
The patient is positioned supine with the affected hand on a hand table. Regional anesthesia (e.g., supraclavicular block) or local anesthesia with a digital block is administered. A pneumatic tourniquet is applied to the upper arm.
Surgical approach
A meticulous skin incision is marked, typically a Bruner-type or mid-lateral incision centered over the affected PIP joint [Video 1]. The incision should provide adequate exposure to both the volar plate and the injured CL. The skin and subcutaneous tissues are carefully dissected and elevated, protecting the neurovascular structures. The dissection proceeds down to the avulsed volar plate and the involved CL (radial or ulnar). The small bone fragment attached to the volar plate and CL is often found rotated, with its articular surface facing the fracture site at the base of the middle phalanx. Carefully dissect the fragment to ensure it is free from any adhesions, paying attention to the flexor tendon sheath.
Video 1:
Video 1:Intraoperative video demonstrating the step-by-step approach to open reduction and K-wire fixation of the volar plate and radial collateral ligament injury with bone avulsion.K-wire fixation
Prepare the avulsed fragment and the corresponding fracture site on the middle phalanx base by removing any interposed soft tissue. Gently reduce the fragment, ensuring proper anatomical alignment. The size of the K-wire used for fixation will depend on the size of the avulsed fragment. In most cases, a 1.0 mm or 1.2 mm K-wire provides sufficient stability. A K-wire (typically 1.2 mm in our experience) is inserted into the volar aspect of the fragment, close to its articular margin. It is advanced across the fracture site and into the dorsal aspect of the middle phalanx under fluoroscopic guidance. Once accurate placement is confirmed, the volar portion of the K-wire is cut short and buried beneath the bone. The dorsal end is left longer for easier removal in the outpatient setting. This fixation primarily aims to achieve bony union at the CL avulsion site. While the volar plate avulsion is indirectly reduced, when the fragment is very small, as is often the case, it is typically left alone to heal by a fibrous union, which is usually sufficient for restoring volar plate function in this context.
Confirming reduction and stability
The PIP joint is taken through a range of motion to assess the fixation stability. Fluoroscopy is used to confirm that the volar plate and CL are adequately reduced and that the joint is stable throughout the range of motion.
Reinforcing the repair
The remnants of the CL are sutured to the intact accessory CL using non-absorbable sutures. These sutures can be passed through the volar plate to augment fixation and provide additional stability.
Wound closure and immobilization
The skin is closed with non-absorbable sutures. A dorsal blocking splint is applied to the finger, maintaining the PIP joint in slight flexion to protect the repair.
Postoperative rehabilitation
Early active mobilization of the PIP joint is initiated on postoperative day 2, encouraging flexion while initially limiting full extension. Radiographs are obtained at 3 weeks to assess fracture healing.
K-wire removal and continued rehabilitation
The K-wire is typically removed at 4 weeks postoperatively. A progressive rehabilitation program is then initiated, focusing on restoring full PIP joint motion and function. A nighttime extension splint may be used for a short period to protect the healing ligaments. Patients can gradually return to daily activities and progressively increase their activity levels as tolerated.
ILLUSTRATIVE CASE
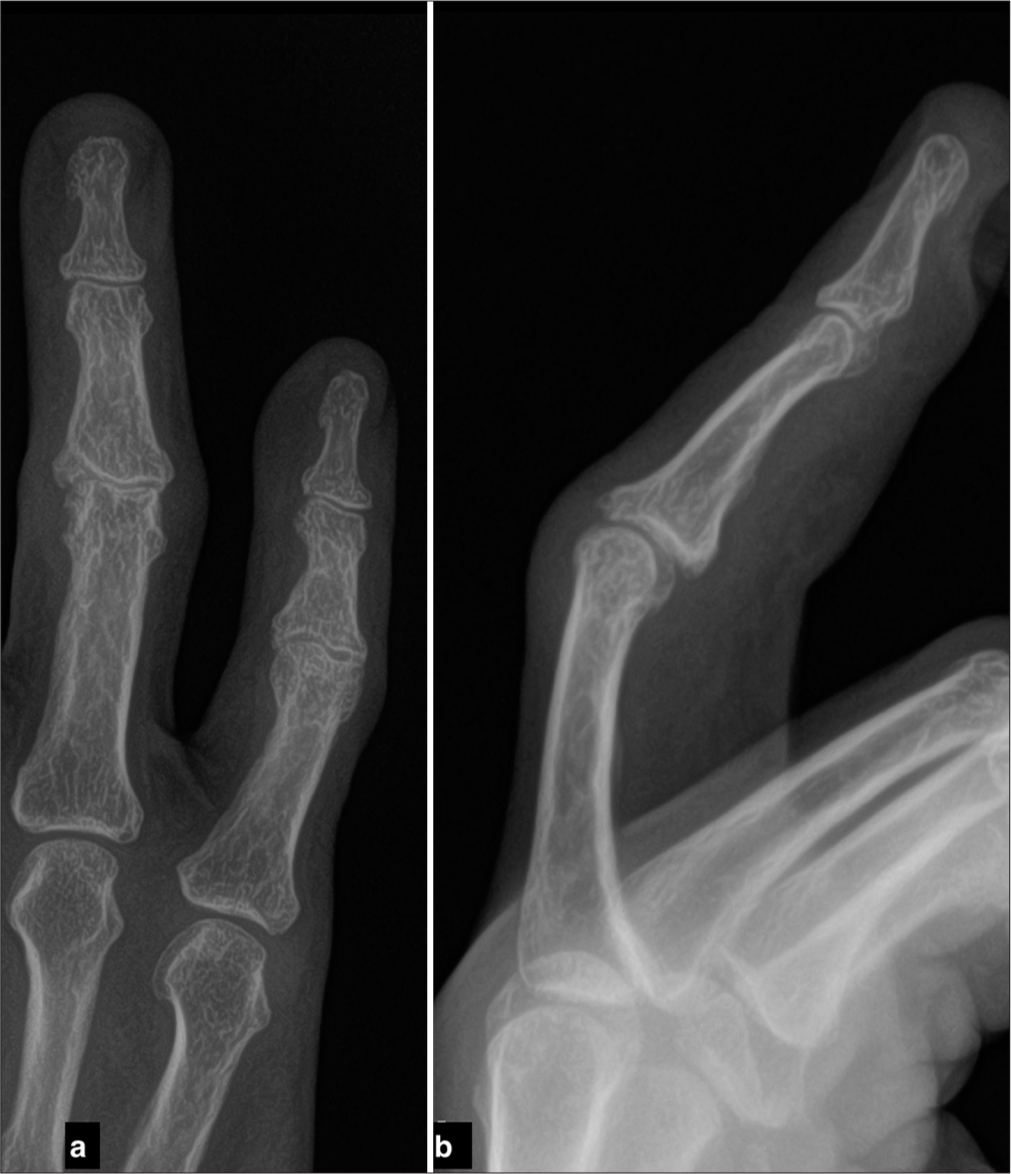
A 62-year-old right-hand dominant woman presented to our clinic with right ring finger pain, swelling, and restricted motion following a chain-snatching incident 1 week prior. During the incident, she sustained a severe injury to her finger while resisting the assailant. She had not received any prior treatment. The right ring finger PIP joint was tender to palpation with an apparent volar prominence on examination. There was a limited range of motion with pain in both active and passive movement. Radiographs demonstrated a volar plate avulsion fracture with an associated radial CL avulsion [Figure 1]. A computed tomography (CT) scan confirmed that the bony fragment was rotated 90° and separated from the middle phalanx base [Figures 2, 3]. While magnetic resonance imaging (MRI) is not always necessary in these cases, as the bony injury and displacement are typically well-appreciated on CT, it was obtained in this instance to evaluate further the extent of soft tissue injury, particularly the volar plate and CL complex. The MRI confirmed the volar plate avulsion and radial CL injury with the associated bone fragment [Figure 4]. Given the displacement and instability, we proceeded with open reduction and internal fixation. A Bruner-type incision was made over the radial aspect of the PIP joint. Careful dissection exposed the avulsed volar plate and radial CL [Figure 5]. The small bone fragment was identified and reduced anatomically to the base of the middle phalanx. A 1.2 mm K-wire was used to secure the fragment, advancing it from volar to dorsal across the fracture site [Video 1]. The radial CL was then repaired using non-absorbable sutures passed through the volar plate for augmentation.
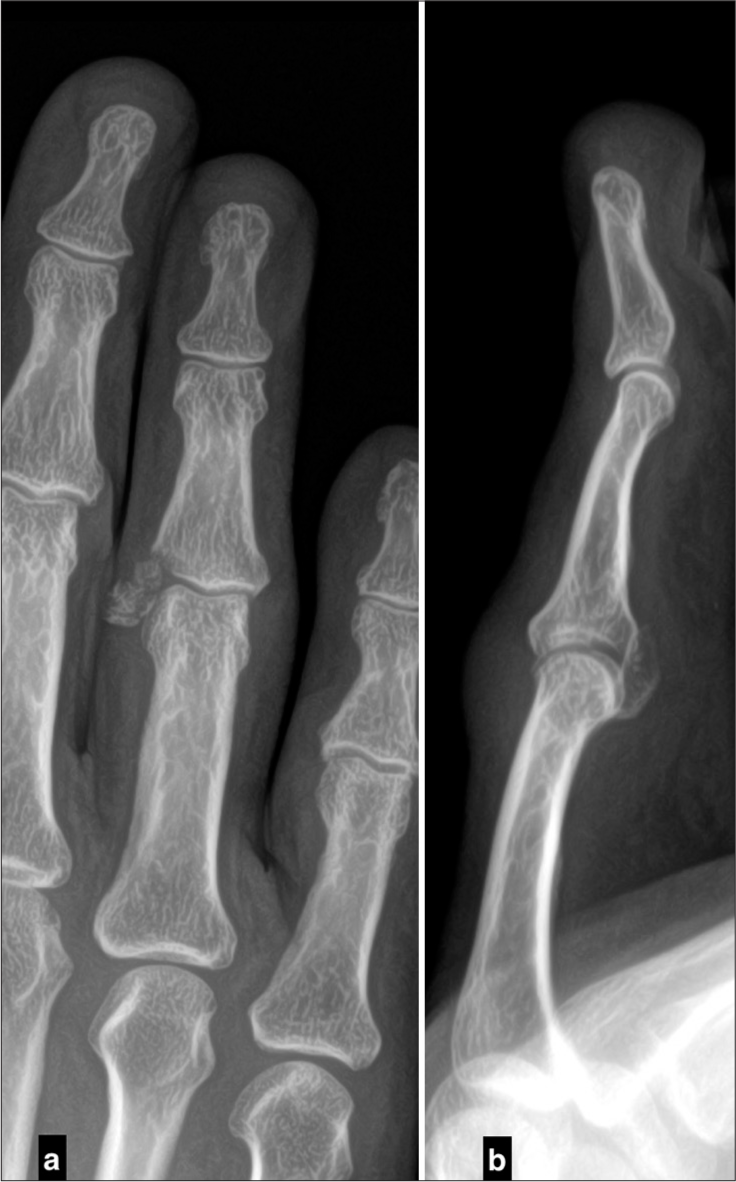
- (a) Anteroposterior and (b) lateral radiographs of the right ring finger demonstrating a volar plate avulsion fracture with an associated radial collateral ligament avulsion.
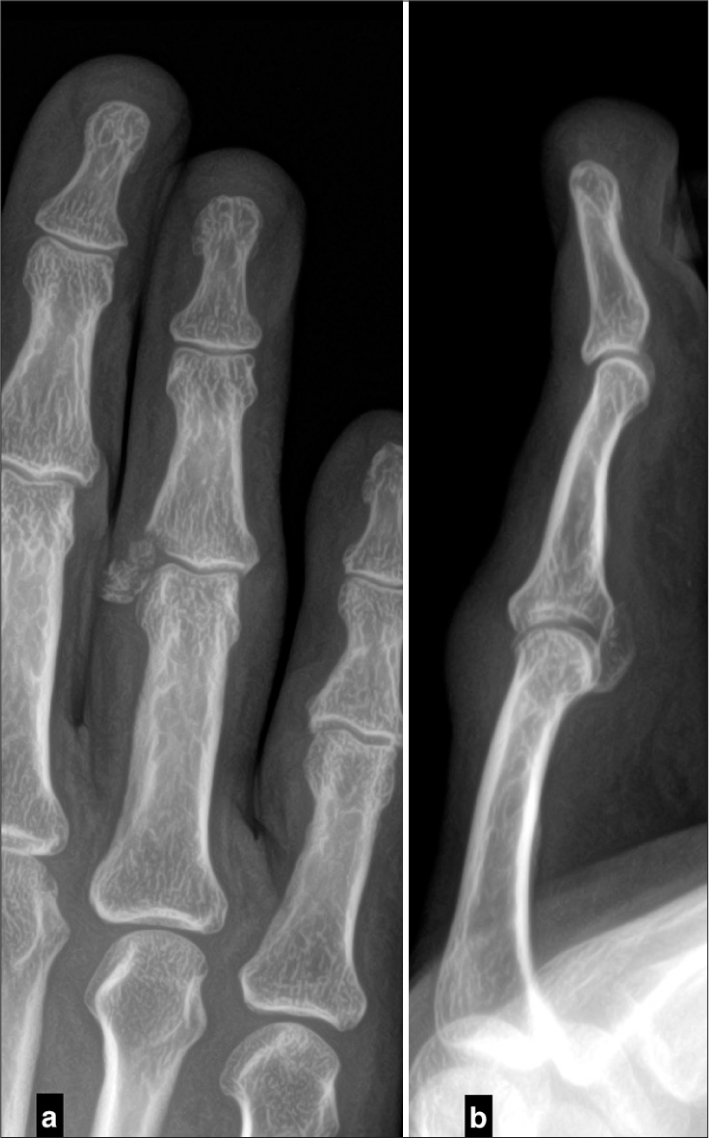
- (a) Coronal and (b) sagittal computed tomography scan images confirming the avulsion fracture and demonstrating the displacement of the fragment.
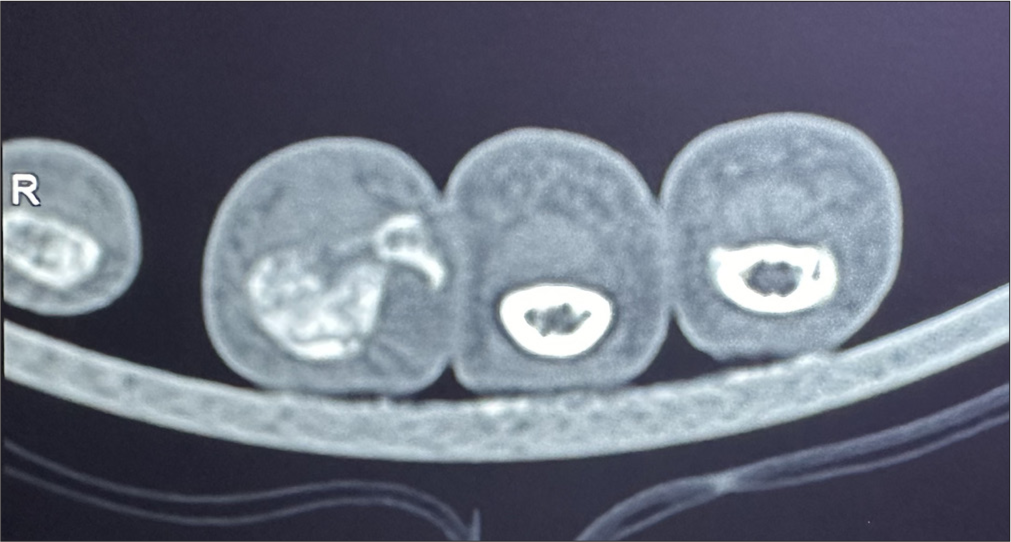
- Axial computed tomography scan image showing the bone fragment rotated and displaced from the base of the middle phalanx.

- Magnetic resonance imaging confirming the volar plate and radial collateral ligament injury with the associated bone avulsion.
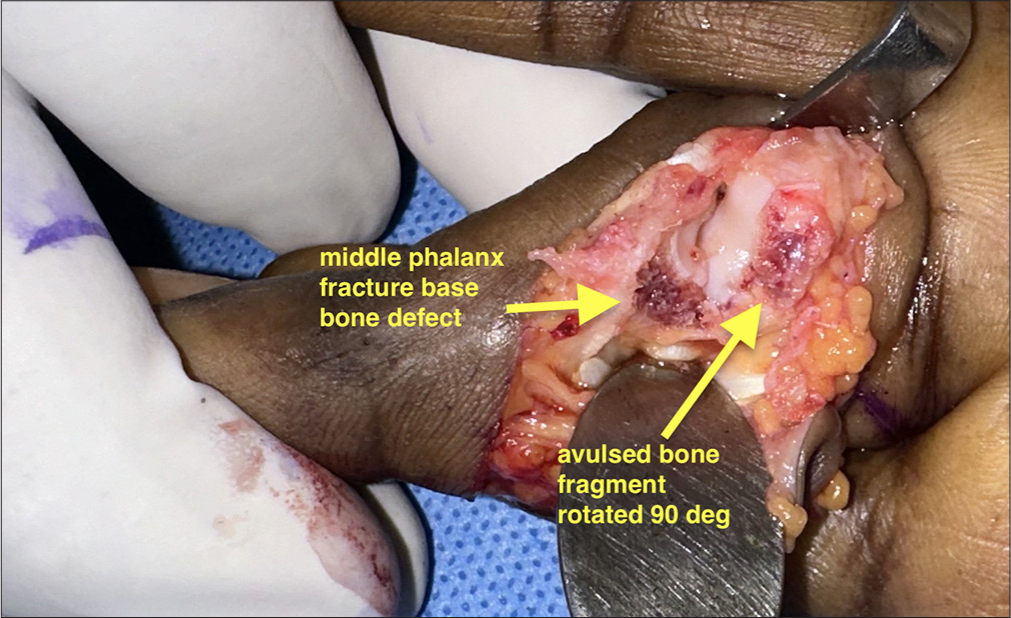
- The intraoperative image reveals a 90-degree rotated avulsed middle phalanx bone fragment, with visible bone defects at the base of the middle phalanx.
Postoperative radiographs showed a well-reduced and congruent PIP joint with the K-wire stabilizing the avulsed bone fragment [Figure 6]. The finger was immobilized in a dorsal blocking splint, allowing immediate active flexion exercises.

- Immediate postoperative radiographs in the (a) anteroposterior and (b) lateral projections showing a well-reduced bone fragment restoring proximal interphalangeal joint congruity using a K-wire (white line).
At 4 weeks postoperatively, radiographs confirmed the union of the avulsed bone fragment, and the K-wire was removed. The patient began active finger extension exercises and continued with a customized hand therapy program.
At 1-year follow-up, the patient had regained excellent range of motion of the PIP joint (5–110°). Final radiographs showed a congruent and stable PIP joint with complete healing of the middle phalanx base fracture [Figure 7]. At the 1-year follow-up, grip and pinch strength were measured as 25.4 kg and 4.9 kg, respectively. These values represented 90% of the patient’s contralateral, uninjured hand, indicating a good functional recovery. Her Quick disabilities of the arm, shoulder, and hand (QuickDASH) score was 2.4, and her Visual Analog Scale (VAS) pain score was 0, indicating minimal disability and no pain. She was able to perform all her daily activities without difficulty [Figure 8].
- Follow-up radiographs at one year in the (a) anteroposterior and (b) lateral projections demonstrating good union of the bone fragment with a congruent proximal interphalangeal joint.

- Clinical photographs of the right ring finger at one-year follow-up, demonstrating a good range of motion of the proximal interphalangeal joint.
BRIEF OVERVIEW OF FOUR ADDITIONAL CASES
We have successfully utilized this technique in four additional patients (three males, one female; age range 45–71 years) with similarly displaced and rotated radial CL avulsion fractures of the PIP joint. All patients presented with pain, swelling, and instability of the affected PIP joint. The bony fragment was rotated 90° in all cases, with the articular surface facing the fracture bed. The surgical technique described above was employed, achieving stable fixation and anatomical reduction in all cases. At a minimum follow-up of 6 months, all patients demonstrated radiological union, a stable and congruent PIP joint, and a functional range of motion (average flexion 95°, extension lag <10°). The average grip strength was 28.5 kg, the average pinch strength was 4.2 kg, the average DASH score was 4.5, and the average VAS score for pain was 0.4. Importantly, all patients in this small series returned to their previous work duties.
PEARLS
Successful surgical management of volar plate avulsion fractures with CL injuries requires careful attention to several key factors. Accurate preoperative assessment with good quality radiographs and, if necessary, a CT scan is crucial to characterize the injury and fully identify small bone fragments. A meticulous surgical approach is essential to avoid further injury to the soft tissues and neurovascular structures. Proper fragment preparation ensures adequate removal of any interposed soft tissue, allowing for proper reduction and healing. Stable fixation with appropriately sized K-wires is necessary to secure the fragment to the middle phalanx base.
Avoid using screws, as drilling and screw insertion may fracture the small bone fragment, making fixation challenging. K-wires offer a simpler approach, often requiring only a single attempt to achieve a good fragment reduction, indirectly facilitating ligament healing. Fluoroscopic confirmation helps confirm accurate reduction and stable fixation throughout the range of motion. Consider reinforcing the repair with sutures to augment the CL and enhance stability. Early active PIP joint mobilization is crucial to prevent stiffness and promote healing.
PITFALLS
While the described technique offers several advantages, surgeons should consider potential pitfalls. Inadequate fragment reduction can lead to persistent joint incongruity and instability, compromising long-term outcomes. K-wire fixation, while commonly used, is associated with potential complications such as pin breakage, migration, and pin-track infection. Prolonged immobilization should be avoided to minimize the risk of joint stiffness, and early mobilization is crucial to promote healing and restore function. Finally, it is essential to carefully assess for any associated injuries, such as central slip or extensor tendon injuries, which may require additional treatment to optimize outcomes.
DISCUSSION
Managing displaced CL avulsion fractures with rotated bony fragments of the PIP joint presents a distinct challenge, particularly when associated with volar plate injuries. While literature exists on managing avulsion fractures at the metacarpophalangeal joint, suggesting conservative treatment for many cases,[1,2,4,5] there is a paucity of research specifically addressing this unique injury pattern at the PIP joint. Furthermore, the principles guiding the treatment of PIP pilon fractures and dorsal fracture-dislocations, which often involve closed reduction, external fixation, or various open reduction techniques, including hook plates, screws, or cerclage wires, do not directly translate to this specific injury.[3-5] In select cases of pilon fractures and dorsal fracture-dislocations, hemi-hamate, or hemi-capitate arthroplasty may be considered, however, this does not apply to the injury pattern addressed in our study.[6]
This technical note contributes to the limited literature by presenting a simple and effective surgical technique for managing displaced and rotated CL avulsion fractures with associated volar plate injuries. Our K-wire fixation approach focuses on achieving a stable anatomical reduction of the rotated fragment, indirectly addressing the volar plate and CL. Another strategy for managing these small, rotated fragments is the use of suture anchors, which can provide stable fixation and allow for early mobilization. The successful outcome in our illustrative case, along with the favorable results in our small case series (average grip strength 28.5 kg, pinch strength 4.2 kg, DASH score 4.5, VAS score 0.4, and all patients returning to work), demonstrates the efficacy of this technique.
The decision to proceed with open reduction and K-wire fixation was based on several factors, including the significant displacement and 90° rotation of the radial collateral ligament avulsion fragment, the resulting joint instability, and the limitations of screw fixation for such small fragments. Our technique offers several advantages in this context. It is minimally invasive, allows for precise fragment reduction under direct visualization, and provides sufficient stability to allow for early mobilization. This is crucial for minimizing stiffness, a common complication following PIP joint injuries.
While our results are encouraging, we acknowledge the limitations of a small case series. Further research, including larger prospective studies, is needed to validate these findings and to further refine treatment algorithms for this specific injury pattern. Future studies could also investigate the long-term outcomes of this technique, including the incidence of post-traumatic arthritis and the need for any secondary procedures.
CONCLUSION
Our described surgical technique focuses on achieving stable fixation and restoring joint congruity using a simple and straightforward K-wire fixation method. This approach has yielded good radiological and functional outcomes in our case series, including the illustrative case presented. By addressing the avulsed fragment and indirectly reducing the volar plate and CL, we aim to promote healing in an anatomical position, facilitating early mobilization and restoring PIP joint function. The technique is particularly useful for cases with significantly displaced and rotated (90°) bony fragments, where conservative management is likely to fail and screw fixation is not feasible.
Ethical approval
Ethical approval for this study was obtained from the OHRC Institutional Review Board (IRB)/Ethics Committee, reference number 35/2024, dated 1 December 2024.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published, and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Volar plate avulsion fracture alone or concomitant with collateral ligament rupture of the proximal interphalangeal joint: A comparison of surgical outcomes. Arch Plast Surg. 2018;45:458-65.
- [CrossRef] [PubMed] [Google Scholar]
- Operative treatment for volar plate avulsion fractures of the fingers. Arch Orthop Trauma Surg. 2013;133:1463-7.
- [CrossRef] [PubMed] [Google Scholar]
- Volar dislocation of the proximal interphalangeal joint. Orthop Surg. 2021;5:6-8.
- [CrossRef] [Google Scholar]
- Treatment for acute proximal interphalangeal joint fractures and fracture-dislocations: A systematic review of the literature. J Hand Microsurg. 2020;12:S9-15.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative dorsal proximal interphalangeal joint subluxation in volar base middle phalanx fractures. J Hand Microsurg. 2020;12:32-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hemi-capitate arthroplasty for dorsal fracture-dislocations of the proximal interphalangeal joint: Surgical technique and illustrative case. Indian J Orthop. 2023;57:527-32.
- [CrossRef] [PubMed] [Google Scholar]






