Translate this page into:
Surgical versus nonsurgical treatment of distal femur physeal fractures: A systematic review and meta-analysis
2 Department of Surgery, Division of Orthopaedic Surgery, Sidra Medical and Research Center, Doha, Qatar
Corresponding Author:
Talal Ibrahim
Department of Surgery, Division of Orthopaedic Surgery, Sidra Medical and Research Center, P.O. Box 26999, Doha
Qatar
tibrahim@sidra.org
| How to cite this article: Alhammoud A, Younis MH, Ahmed AF, Ibrahim T. Surgical versus nonsurgical treatment of distal femur physeal fractures: A systematic review and meta-analysis. J Musculoskelet Surg Res 2019;3:179-183 |
Abstract
Distal femur physeal fractures can lead to growth disturbance such as premature physeal closure (PPC), leg length discrepancy (LLD), and angular deformity (AD). This study aims to systematically review the literature to assess whether surgical management is associated with a different rate of growth disturbances compared to nonsurgical treatment. We searched several databases from 1966 to 2018 for studies that evaluated surgical versus nonsurgical treatment of distal femur physeal fractures. Descriptive and quantitative data were extracted, and a meta-analysis was performed using a random-effects model to pool odds ratio (OR) for the comparison of PPC, LLD, and AD rate between children undergoing surgical versus nonsurgical treatment. Of the 470 articles identified, 11 case series were eligible, with a total of 527 distal femur physeal fractures. The pooled OR of PPC between surgical and nonsurgical treatments showed no statistically significant difference (OR = 0.30, 95% confidence interval [CI]: 0.30–3.03; I2 = 73.4%, P = 0.01). No significant difference in the rates of LLD (OR = 1.03, 95% CI: 0.36–2.94; I2 = 0%, P= 0.87) and AD (OR = 0.40, 95% CI: 0.10–1.57; I2 = 0%, P = 0.79) was detected between surgical and nonsurgical treatments. Despite the current evidence to date does not support an association between the method of treatment of distal femur physeal fractures and the risks of PPC, LLD, and AD, a significant clinical relevance cannot be carried out. Surgeons can use both treatment methods as dictated case by case.Introduction
Among all growth plates in humans, the distal femur physis is considered the fastest in growth rate. The distal femur physis contributes up to 40% and 70% of the total linear growth of the body and femur, respectively.[1],[2] In the pediatric age group, distal femur physeal fractures are considered uncommon and account for 7% of lower limb physeal fractures.[3] Distal femur physeal fractures usually occur following a hyperextension injury of the knee[4] and can result in significant growth disturbances approaching 90% that are manifested as a premature physeal closure (PPC), leg length discrepancy (LLD), angular deformity (AD),[1],[4],[5],[6] and physeal bridge formation. Physeal bridge formation in the distal femur is common after injury due to the large surface area with marked undulation of the physis.[7] Salter-Harris (S-H) Type II injuries comprise the majority of distal femur physeal fractures and tend to occur frequently in older children.[4],[8],[9] S-H Type I fractures of the distal femur are the least associated with growth disturbances, whereas S-H Type IV fractures lead to the highest incidence of growth complications.[4] Conversely, other studies report a higher incidence of complications with Type II fractures compared to Type IV.[10] In the literature, controversy exists in terms of the use of the S-H classification to predict the occurrence of growth disturbances following distal femur physeal fractures.[3],[4],[8],[10],[11],[12],[13] Several factors have been found to be related to poor prognosis following these fractures such as injury at a young age,[3] fractures due to significant trauma,[3],[13] fracture pattern,[4],[6],[8] initial displacement and the quality of fracture reduction.
The treatment of distal femur physeal fractures can be performed using both surgical and nonsurgical techniques. Surgical treatment of distal femur physeal fractures with open reduction and internal fixation has been recommended to minimize potential growth disturbances,[6],[10],[14] whereas nonsurgical treatment with closed reduction and cast immobilization has resulted in growth disturbances due to subsequent displacement.[6]
In this study, we aim to systematically review the literature regarding growth disturbances occurring in surgical versus nonsurgical treatment of distal femur physeal fractures.
Materials and Methods
This meta-analysis was conducted in adherence to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[15]
Search strategy
The databases that were searched included MEDLINE, Cochrane Registry of Clinical Trials, and EMBASE (January 1966–August 2018). The primary terms for the search were “distal femur and fracture or injury and pediatric or paediatric or children.” Two independent authors assessed the eligibility of identified studies. Studies eligible for full review included articles published in English and those with accessible full text. Unpublished worked was not included in our review.
Selection of studies
We considered any clinical study that directly compared surgical to nonsurgical treatment of distal femur physeal fractures in children (below 18 years) and reported the three complication rates of PPC, LLD, and AD. Surgical treatment was defined as open reduction and internal fixation, whereas nonsurgical treatment was defined as either casting alone, traction, or closed reduction and casting. We defined PPC as the radiographic appearance of a bony bar in the distal femur physis in the injured limb. LLD was defined as a difference of 15 mm between the affected and nonaffected lower limbs. AD was defined as angulation of the fracture site by 10° or more in the coronal and/or sagittal planes.
Data collection
Two independent authors extracted the following data of interest: the first author's name, study year and country, study design, number of patients, patient's mean age and gender, number of surgically and nonsurgically treated patients, and the number of growth disturbance events.
Quantitative synthesis
We performed the meta-analytic comparisons using the open meta-analyst tool.[16]
Given that our outcome of interest was the occurrence of growth disturbance, which is dichotomous, we summarized the outcomes with odds ratio (OR) to achieve the comparisons.
The comparisons were conducted with a binary random effects model using the DerSimonian–Laird method.[17] The meta-analysis had a confidence interval (CI) level of 95% and a correction factor of 0.5, and the heterogeneity across studies was determined through reporting the I2 statistic. Our primary comparison was the PPC between surgical and nonsurgical treatments for distal femur physeal fractures. In addition, our secondary comparisons were LLD and AD between both treatments.
Results
Search strategy
The search strategy resulted in 470 publications, with 11 articles matching our inclusion criteria which were included in our analysis. These 11 studies were case series and evaluated the rate of PPC, LLD, and/or AD in children who had surgical and nonsurgical treatments for distal femur physeal fractures. [Figure - 1] summarizes the PRISMA flowchart of our search strategy. The level of evidence of this study was Level IV as determined by the lowest included evidence. The interobserver agreement on study eligibility was perfect (kappa statistic = 100%).
 |
| Figure 1: Flow diagram of search strategy and the yield of eligible studies |
Characteristics of the included studies
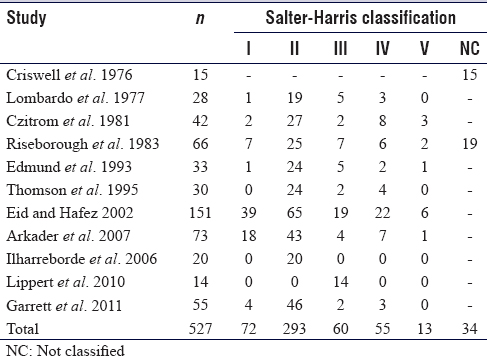
[Table - 1] displays the characteristics of the included studies. We identified a total of 527 pediatric distal femur physeal fractures and a total of 79 cases with complications, 39 cases with PPC, 23 cases with LLD, and 17 cases with AD. The S-H classification[11] was used to describe a fracture pattern in all included studies. Most of the included fractures (55.5%) were classified as S-H Type II. [Table - 2] displays the different S-H-type distal femur physeal fractures. Surgical treatment was undertaken in 202 fractures in the form of open reduction with percutaneous pinning or screw fixation, whereas nonsurgical treatment was undertaken in the form of either casting alone, traction, or closed reduction and casting in 306 fractures. The treatment of 19 distal femur physeal fractures was not reported in the study by Riseborough et al.[3] The mean follow-up period was 9 years (range: 0.2–20 years) across all studies.

Quantitative synthesis
Across all studies, nonsurgical treatment was associated with a 2.5-fold greater rate of PPC (53.8%) when compared to surgical treatment (22.2%). The forest plot of the comparison between surgical and nonsurgical treatments for physeal growth disturbance is shown in [Figure - 2]. In 4 of the 11 retrospective case series[6],[12],[13],[18] that reported PPC, the pooled OR was 0.30 (95% CI: 0.03–3.03; I2 = 73.4%, P = 0.010) for PPC (surgical vs. nonsurgical treatment). Therefore, there was no significant difference between surgical and nonsurgical treatments with regard to PPC development. Secondary analysis for the comparison of LLD rate of surgical versus nonsurgical treatment in distal femur physeal fractures included 5 of the 11 studies.[4],[6],[12],[14],[18] This showed an overall pooled OR of 1.03 (95% CI: 0.36–2.94; I2 = 0%, P = 0.87) for LLD (surgical vs. nonsurgical treatment), which indicates no significant difference in terms of LLD in distal femur physeal fractures. Furthermore, an analysis comparing AD rates of surgical and nonsurgical treatment included 4 of the 11 studies.[4],[6],[12],[18] This resulted in a pooled OR of 0.40 (95% CI: 0.10–1.57; I2 = 0%, P = 0.79); hence, no significant difference was detected between both treatments. [Figure - 3] and [Figure - 4] display the comparisons of LLD and AD, respectively. No publication bias was evident on funnel plots and Egger test.
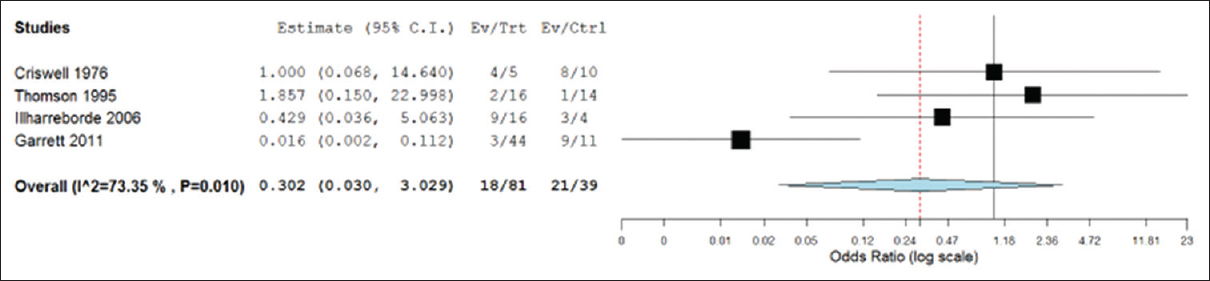 |
| Figure 2: Forest plot of premature physeal closure in distal femur physeal fractures |
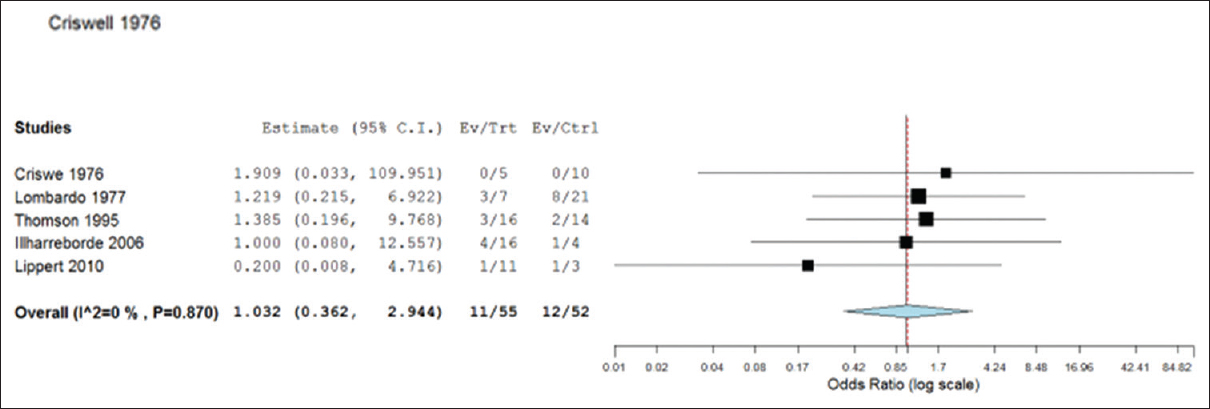 |
| Figure 3: Forest plot of limb length discrepancy of more than 15 mm in distal femur physeal fractures |
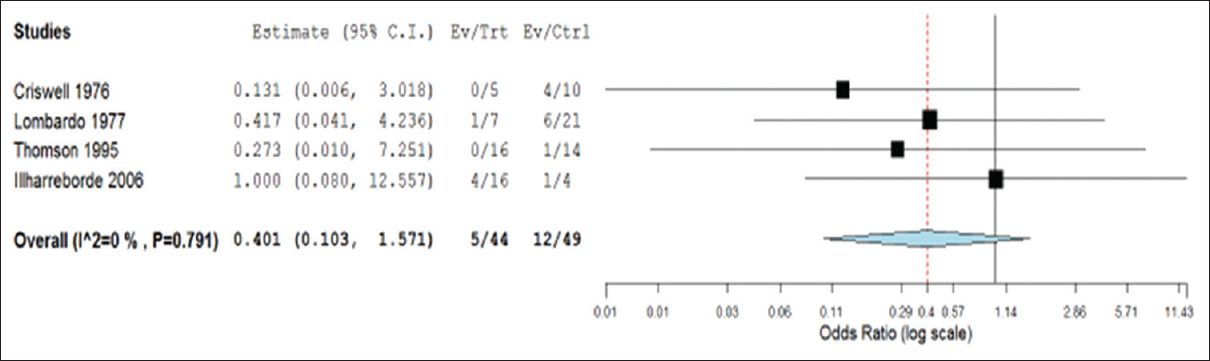 |
| Figure 4: Forest plot of angular deformity of more than 10° in distal femur physeal fractures |
Discussion
The pooled analysis of included studies showed that the PPC rate was 2.5-fold greater in the nonsurgical group (mean PPC rate: 53.8%) than the surgical group (mean PPC rate: 22.2%) despite no statistically significant difference. In the secondary analysis, we compared LLD and AD rates between patients who were managed with surgical and nonsurgical treatments. We found that surgical treatment was associated with an LLD rate of 20% compared to 23% of those who underwent nonsurgical treatment, and this was statistically not significant. In addition, patients who underwent surgical treatment had a 2-fold reduction in AD rate (11.3%) in comparison to nonsurgical treatment (24.4%), and this was also statistically not significant.
Results were consistent across different assumptions. Although some limitations exist in the current literature on this topic such as small sample size and the different methods of analysis and interpretation of results that prevented us from reaching a solid conclusion. Three outcomes were reported in the included study, the rate of PPC, LLD, and AD in distal femur physeal fractures.
The aim of treatment of distal femur physeal fractures is to prevent the outcome of growth disturbances and deformities. We found that there was no statistically significant difference between surgical and nonsurgical treatment for distal femur physeal fractures in terms of growth disturbance.
Multiple risk factors that may affect the growth disturbances in such fractures and consequently could affect the mode of treatment need to be considered in the relevant literature.
Age at the time of injury is considered an important determinant for growth disturbances. Riseborough et al.[3] found that 80% of children had LLD and AD when compared to 50% of adolescents who sustained distal femur physeal fractures, thus indicating worse outcomes with younger age groups. In contrast, two studies by Arkader et al.[8] and Garrett et al.[13] found no significant association with patients' age and the occurrence of growth disturbances.
The configuration of distal femur physeal fractures has been debated as a prognostic risk factor. The S-H[11] classification is widely used to classify such fractures. Lombardo and Harvey[4] concluded in a retrospective review of 34 distal femur physeal fractures that the S-H is not a reliable indicator alone for the development of growth disturbances. Furthermore, Riseborough et al.[3] reported that the S-H classification is insufficient to predict growth disturbances and particularly in the distal femur. Similarly, Eid and Hafez[10] reported similar conclusions in their retrospective study of 151 fractures. On the other hand, Arkader et al.[8] found that the S-H classification was a significant predictor of growth disturbances in distal femur physeal fractures. Similarly, Garrett et al.[13] concluded that the S-H classification provided a significant prediction for growth disturbances in a retrospective review of 55 cases of distal femur physeal fractures. In addition, Lippert et al.[14] found that S-H Type III distal femur physeal fractures had a high rate of poor outcomes. Ilharreborde et al.[12] were in favor of the S-H classification; however, they suggested that the classification can be improved by subdividing S-H Type II fractures into two groups depending on the presence or absence of metaphyseal comminution, with the latter harboring worse outcomes.
Displacement of distal femur physeal fracture is considered to be directly proportionate to the rate of growth disturbances. In a study of 34 distal femur physeal fractures, Lombardo and Harvey[4] reported that the initial displacement and quality of reduction of the fracture correlated with the incidence of growth disturbances. Likewise, Thomson et al.[6] found that physeal complications were significantly increased in displaced fractures when compared to the nondisplaced. However, Arkader et al.[8] concluded that growth disturbances were significantly predicted by the presence of residual displacement after reduction rather than the degree of initial displacement. This was supported by Garret et al.[13] as they concluded that the degree of initial displacement was an irrelevant predictor of physeal arrest. Displaced fractures may be initially reduced in the emergency department, and thus, any significant displacement might be reported as minimally or nondisplaced. Therefore, we believe that any initial displacement is unreliable and importance should be emphasized on the quality of the definitive reduction.
The mechanism of injury is another prognostic factor of the occurrence of growth disturbances of distal femur physeal fractures. Riseborough et al.[3] found that children had a higher rate of PPC after high-energy trauma mechanism. Similarly, Garrett et al.[13] reported that PPC in distal femur physeal fractures occurred in 5.3% of patients who sustained low-energy trauma compared to 31% in those who sustained high-energy trauma.
The quality of studies that assessed the rates of PPC, LLD, and AD among distal femur physeal fractures was the main limitation of this review. All of the included studies were case series, which have limitations in design to provide significant results. In addition, surgically treated cases tend to be significantly displaced and might have worse outcomes when compared to the nonsurgically treated cases, and this can lead to biased outcomes. The meta-analysis was performed to reflect the results of interesting outcomes. We could not include other important factors such as the type of operative fixation used, number of attempted reductions, degree of initial and residual displacement, and mechanism of injury, further prospective studies are required in this regard. Hence, a limited conclusion can be drawn from the current literature.
Conclusions
Although our meta-analysis on case series showed that there was no statistically significant difference between both methods of treatment and surgeons can use both treatment methods based on case. Therefore, multicenter prospective cohort studies will be required to answer the main debate whether surgical or nonsurgical treatment can decrease the growth disturbances following distal femur physeal fractures.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AA conceived and designed the study, conducted research, provided research materials, and collected and organized data. wrote initial and final draft of the article MY collected and organized data analyzed and interpreted data. wrote initial and final draft of the article AFA wrote initial and final draft of the article. TI conceived and designed the study, review the initial and final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Cassebaum WH, Patterson AH. Fractures of the distal femoral epiphysis. Clin Orthop Relat Res 1965;41:79-91. [Google Scholar] |
| 2. | Edmunds I, Nade S. Injuries of the distal femoral growth plate and epiphysis: Should open reduction be performed? Aust N Z J Surg 1993;63:195-9. [Google Scholar] |
| 3. | Riseborough EJ, Barrett IR, Shapiro F. Growth disturbances following distal femoral physeal fracture-separations. J Bone Joint Surg Am 1983;65:885-93. [Google Scholar] |
| 4. | Lombardo SJ, Harvey JP Jr. Fractures of the distal femoral epiphyses. Factors influencing prognosis: A review of thirty-four cases. J Bone Joint Surg Am 1977;59:742-51. [Google Scholar] |
| 5. | Basener CJ, Mehlman CT, DiPasquale TG. Growth disturbance after distal femoral growth plate fractures in children: A meta-analysis. J Orthop Trauma 2009;23:663-7. [Google Scholar] |
| 6. | Thomson JD, Stricker SJ, Williams MM. Fractures of the distal femoral epiphyseal plate. J Pediatr Orthop 1995;15:474-8. [Google Scholar] |
| 7. | Khoshhal KI, Kiefer GN. Physeal bridge resection. J Am Acad Orthop Surg 2005;13:47-58. [Google Scholar] |
| 8. | Arkader A, Warner WC Jr., Horn BD, Shaw RN, Wells L. Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop 2007;27:703-8. [Google Scholar] |
| 9. | Graham JM, Gross RH. Distal femoral physeal problem fractures. Clin Orthop Relat Res 1990;255:51-3. [Google Scholar] |
| 10. | Eid AM, Hafez MA. Traumatic injuries of the distal femoral physis. Retrospective study on 151 cases. Injury 2002;33:251-5. [Google Scholar] |
| 11. | Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am 1963;45:587-622. [Google Scholar] |
| 12. | Ilharreborde B, Raquillet C, Morel E, Fitoussi F, Bensahel H, Penneçot GF, et al. Long-term prognosis of salter-harris Type 2 injuries of the distal femoral physis. J Pediatr Orthop B 2006;15:433-8. [Google Scholar] |
| 13. | Garrett BR, Hoffman EB, Carrara H. The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. J Bone Joint Surg Br 2011;93:689-94. [Google Scholar] |
| 14. | Lippert WC, Owens RF, Wall EJ. Salter-harris Type III fractures of the distal femur: Plain radiographs can be deceptive. J Pediatr Orthop 2010;30:598-605. [Google Scholar] |
| 15. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol 2009;62:e1-34. [Google Scholar] |
| 16. | Byron CW, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 2012;49:5. [Google Scholar] |
| 17. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Google Scholar] |
| 18. | Criswell AR, Hand WL, Butler JE. Abduction injuries of the distal femoral epiphysis. Clin Orthop Relat Res 1976;115:189-94. [Google Scholar] |
Fulltext Views
4,239
PDF downloads
1,639





