Translate this page into:
Symptomatic osteochondroma in the ventral aspect of the scapula in a child with hereditary multiple exostoses
Corresponding Author:
Bander S Alrashedan
Department of Orthopaedic Surgery, Ministry of Health, King Saud Medical City, Ulaishah, 7790 Al Imam Abdul Aziz Ibn Muhammad Ibn Saud, Riyadh 12746 3617
Saudi Arabia
b.alrashedan@gmail.com
| How to cite this article: Alrashedan BS, Chowdhary SK, Mahmoud J, Hamza OM. Symptomatic osteochondroma in the ventral aspect of the scapula in a child with hereditary multiple exostoses. J Musculoskelet Surg Res 2019;3:370-373 |
Abstract
Osteochondroma is the most common bone tumor. It mainly affects the proximal humerus, tibia, and distal femur. It rarely affects the scapula, especially in the ventral aspect and when it does, winging of the scapula can occur, and can lead to a painful range of motion of the shoulder with a snapping sensation and secondary ribs erosion. Hereditary multiple exostoses (HME) is an autosomal dominant disorder causing multiple osteochondromas mainly in the metaphysis of long bones and it rarely affects the scapula. We present an uncommon presentation in a 7-year-old male with HME who presented with a superolateral ventral large osteochondroma measuring 8 cm × 5.5 cm that caused left scapular winging and left shoulder pain with a secondary ribs deformity. The patient was successfully treated surgically through a direct approach and was followed for 18 months and showed a satisfactory outcome with the regression of the ribs deformity.Introduction
Osteochondroma is the most common benign tumor of the bone.[1] It is also the most common benign tumor involving the scapula.[2] Osteochondroma can present as solitary in 85% of patients or multiple in the form of hereditary multiple exostoses (HME) in 15% of patients.[3] HME is an autosomal dominant skeletal disorder and is found in 1 of 50,000 births.[1] The hallmark of the disease is multiple exostoses growth in the skeleton with most cases are diagnosed before 10 years of age.[4] It usually involves the proximal humerus, distal femur, and proximal tibia, with the distal femur being the most commonly affected location.[4] Other common orthopedic manifestations in HME are: shortening of the ulna with a secondary bowing of the radius, leg length discrepancy, varus or valgus angulation of the knee, and disproportionate short stature.[3],[4] It was reported that around two-thirds of the cases have a positive family history with this disorder.[5] A recent study has reported that 96% of cases with HME had a family history of the disease.[4] The Exostosin--1 (EXT1) gene mutation has been attributed to the most cases of HME.[3] The involvement of the flat bones in HME has been reported and scapular lesions account for 15% of all described lesions.[4] Osteochondromas in HME are generally asymptomatic and are usually found incidentally, with the most common presenting symptoms being pain secondary to the mechanical effect on the surrounding tissues and cosmetically unacceptable mass or swelling.[3],[4],[6] Symptomatic lesions are more commonly seen in young affected cases.[6] Rapid osteochondroma growth is usually seen in the first decade of life with cessation of growth around the time of puberty and physeal closure, with the overall recurrence is estimated to be around 2%.[4] It is rarely involving the ventral aspect of the scapula and can be missed until it is cosmetically unpleasant or painful secondary to inflammation of a bursa, which can overly an osteochondroma, or causing a mass effect on surrounding structures or due to a fracture of the stalk following trauma.[7] Scapular lesions can cause mechanical symptoms limiting the scapulothoracic motion and snapping sensation depending on the location and the size of the lesion.[8] Malignant transformation of osteochondromas in HME has been reported in the literature with the scapula being the second-most location for the malignant transformation after the pelvis.[9] Several cases of osteochondromas involving the ventral aspect of the scapula causing pseudo-winging and mechanical symptoms have been reported in the literature, but in the majority of the reported cases, the lesions were located in the lower half of the scapula and were treated with different surgical approaches likely guided by the location of the lesions.[8],[10],[11],[12],[13],[14] We present a 7-year-old boy with HME who presented with a large symptomatic osteochondroma in the ventral superolateral aspect of the left scapula causing a reversible secondary ribs deformity with surgical treatment. The lesion was excised using a direct approach anterolaterally due its proximity to the superolateral ventral edge of the scapula, and the patient was followed for 18 months with a satisfactory outcome.
Case Report
A 7-year-old male presented to our orthopedic clinic with a history of progressive left shoulder pain and a mass in the left axilla with a deformity in the left upper aspect of the back which became noticeable over 2 years. The pain was associated with snapping of the left shoulder with movement. The condition became cosmetically and functionally disturbing for the patient and his parents. There was no history of trauma, fever, change in weight, night sweats, and the patient had no known history of medical illness on the initial presentation. His only brother who is 13-year-old was diagnosed in another medical center with HME in a young age and was found to have EXT1 mutation. He had multiple osteochondromas involving both distal femurs and tibias, which did not need surgical treatment as they were mildly symptomatic and did not cause functional impairment. Genetic testing was not done to both parents, and they did not have any history of musculoskeletal conditions or complaints.
His clinical examination showed a round, painless, hard, and a fixed mass with the most prominent center anterior to the left mid-axillary line associated with ipsilateral static scapular winging in rest and movement [Figure - 1]. There were multiple palpable painless masses involving the proximal humerus area bilaterally, distal femur area bilaterally, and both proximal leg area with a full painless range of motion actively and passively. Active and passive range of motion of the left shoulder is decreased equally when compared to the right shoulder. Abduction of the left shoulder beyond 90° was painful and was limited to around 110° actively and passively. Left shoulder, pelvis, and both knee radiographs were done and showed multiple osseous lesions around metaphysis, epiphysis, and a left axillary mass causing a mass effect and deformity of the left rib cage suggestive of osteochondromas [Figure - 2]. Genetic testing later was positive for EXT1 mutation as in his older sibling. A computed tomography (CT) scan showed a well-defined pedunculated oval mass in the ventral aspect of the left scapula with its base in the superolateral aspect of the scapula measuring around 8 cm × 5.5 cm and causing a mass effect shifting the scapula dorsally with associated chest wall deformity in the form of depression of multiple ribs with associated cartilaginous cap measuring around 5 mm with irregular subchondral bone [Figure - 3]. Surgical management was offered after the failure of resolution or improvement of the child's symptoms on multiple follow-up visits and physiotherapy aiming to gain a functional painless range of motion.
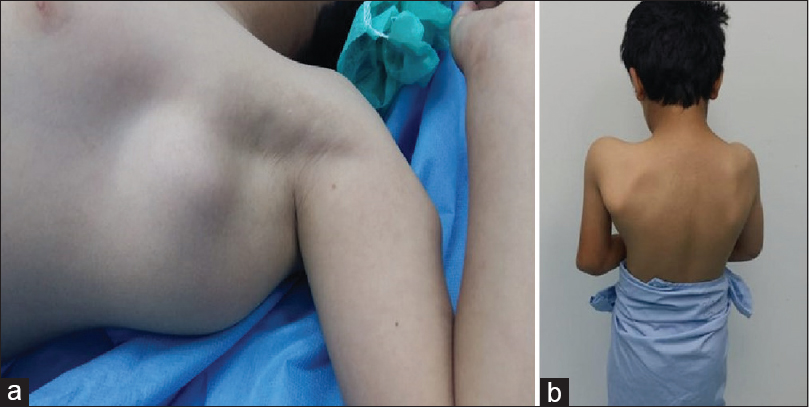 |
| Figure 1: A clinical photograph showing a round mass with the most prominent center anterior to left mid-axillary line (a) with ipsilateral scapular winging on rest while standing (b) |
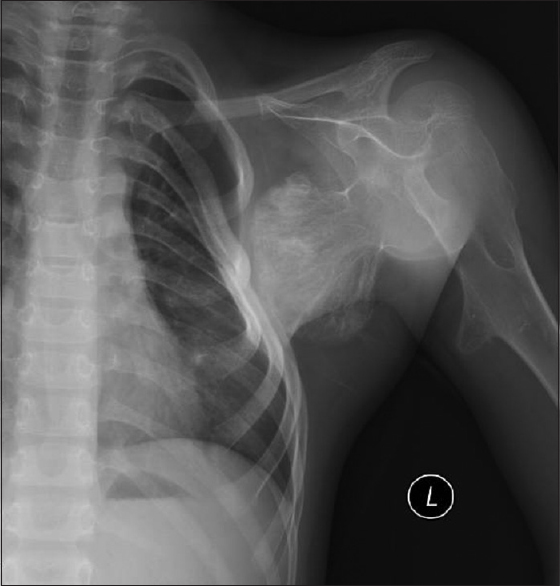 |
| Figure 2: Anteroposterior radiograph of the left shoulder showing an irregular radiopaque pedunculated mass likely arising from the scapula causing a mass effect and deformity of the third to sixth ribs |
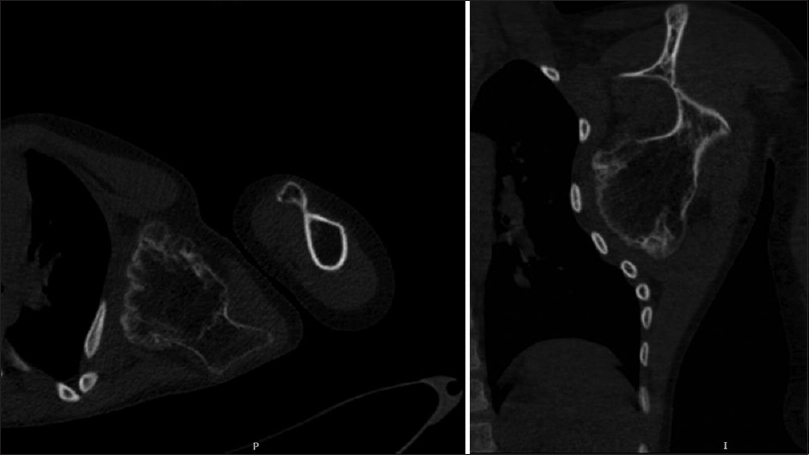 |
| Figure 3: Axial (left), and coronal (right) cuts of a computed tomography scan showing an exostosis arising from the superolateral ventral aspect of the scapula exerting a mass effect on the chest wall causing deformity with associated cartilaginous cap measuring around 5 mm with unremarkable lung parenchyma |
Surgical technique and outcome
Open excision of the mass was done while the patient in a supine position and the left shoulder abducted to 90° and externally rotated with the limb supported using an extension attached to the operation table. A longitudinal incision was made posterior to the mid-axillary line aiming to the superolateral border of the scapula; fascia overlying the latissimus dorsi muscle was found and carefully opened to allow mobilization of the muscle. The latissimus dorsi forming the posterior axillary fold was elevated avoiding dissection medial and anterior to the muscle to avoid injuring the long thoracic and the thoracodorsal nerves. The tumor was found with fibers of subscapularis muscle stretched over the mass and were bluntly dissected. Careful blunt dissection of the mass to its base was carried aiming to clear it from the surrounding adhesions. The mass was excised fully from its base using a curved osteotome with its bursa, and its fibrous periconderium, which was found in continuity with the periosteal covering of the ventral aspect of the scapula. The mass was found to be hard, oval, white, and nodular measuring around 8 cm × 5.5 cm. The patient was discharged without any complications and was instructed to immobilize the limb on a sling. Physical therapy for passive- and active-assisted range of motion exercises of the left shoulder was started 10 days postoperatively. Biopsy results were found to be a typical osteochondroma with a thick cartilaginous cap showing no evidence of malignancy. His range of motion and strength of the left shoulder along with the scapular winging, and the ribs deformity have improved gradually over the course of 18 months postoperatively on multiple follow-up visits. At 18 months postsurgical management, the patient was found to have a symmetrical strength and full range of motion actively and passively in both shoulders with no evidence of static or dynamic scapular winging on the left side. There were newly found two hard painless masses in the inferomedial and dorsal aspect of the left scapula each measuring around 0.5 cm × 0.5 cm which were not evident before this visit. They were prominent during the wall push test and not seen at rest. The left rib cage deformity has almost completely subsided on chest radiograph [Figure - 4].
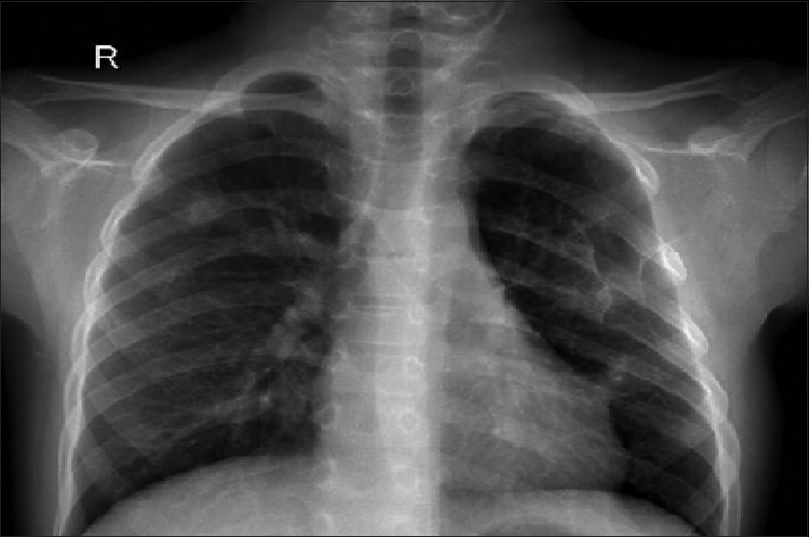 |
| Figure 4: Anteroposterior radiograph of the chest 18 months following surgery demonstrating regression of the left chest wall deformity seen preoperatively |
Discussion
Ventral osteochondromas may lead to snapping of the scapula, painful crepitus, pseudowinging, and bursa formation.[7],[10],[11],[12] It may be difficult to identify or delineate lesions involving the scapula on plain radiographs making CT the study of choice when an osteochondroma is suspected as in our case.[7] Winging of the scapula was initially described as the prominence of the medial (vertebral) border secondary to neuromuscular disorders, and the classic cause is serratus anterior muscle impairment secondary to long thoracic nerve palsy. Scapular tumors; such as osteochondroma, have been described as a cause of pseudowinging, which is a scapular prominence present and unchanged in rest and movement.[14],[15] The center of the lesion in our case is found in the superolateral aspect and was large enough to cause scapular winging and prominence in the left axilla. This, along with the pain, were very concerning for the family, which necessitated surgical management. Several surgical approaches have been described for the treatment of ventral scapular osteochondromas and likely guided by the location of the lesion.[8],[10],[11],[12] Nascimento and Claudio's case was successfully approached arthroscopically since it was in the ventral superomedial aspect of the scapula to avoid injuring the neurovascular structures.[8] Suresh's case was successfully approached through an open posterior approach with a satisfactory outcome as the lesion was also in the superomedial border.[10] In our case, the lesion was in the superolateral border, and the base was close to the superolateral edge of the scapula. For this reason, an anterolateral direct approach was utilized through reflecting the humeral part of latissimus dorsi muscle belly since we had direct access to the lesion's base through relatively smaller area dissected compared to the larger area needed to be dissected through a posterior approach. Given the accessibility of the lesion through intermuscular approach, dissection medial and anterior to the latissimus dorsi humeral muscle was avoided to minimize the risk of injuring the long thoracic and thoracodorsal nerves.[15] Sivananda et al. reported an adult patient with an osteochondroma of the ventral scapula causing secondary rib erosion.[7] In our case, the patient presented with multiple ribs deformities secondary to the lesion, which dramatically decreased 1 year following the excision of the lesion. We believe the young age of the patient is an important factor affecting deformity formation and regression. We were concerned about the serratus anterior and latissimus dorsi functions as their innervation lies close to the surgical field, physical examination was unremarkable for any abnormalities suggesting iatrogenic injury at 18 months postsurgical treatment. Considering the age at presentation, the size of the lesion, and the location of the lesion; the base centered in the superolateral aspect causing secondary rib deformity, which was decreased following surgical intervention made us consider reporting this case in literature.
Conclusion
Osteochondroma of the scapula can present as part of HME. They can be located in the superolateral ventral aspect. Lesions can grow to a profound size and can lead to limitation in range of motion, pain, secondary multiple ribs deformity, and scapular pseudo-winging. Surgical treatment using a direct anterolateral approach reflecting the latissimus dorsi anteriorly is useful in a case of scapular osteochondroma in the ventral superolateral aspect due to the proximity of the lesion to the superolateral edge of the scapula. Secondary ribs deformity can subside following surgical excision of the mass with a good functional outcome.
Ethical consideration
Patient's identification is not revealed, and the parents were informed that data from the case would be submitted for publication and gave their written consent for publication.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the parents have given their consent for the patient's images and other clinical information to be reported in the journal. The parents understand that name and initials will not be published and due efforts will be made to conceal identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
BSA, SKC, JM, and OMH, conceived the study. BSA, SKC, and JM collected, provided, organized materials and data of the patient. BSA wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Saglik Y, Altay M, Unal VS, Basarir K, Yildiz Y. Manifestations and management of osteochondromas: A retrospective analysis of 382 patients. Acta Orthop Belg 2006;72:748-55. [Google Scholar] |
| 2. | Khan Z, Gerrish AM, Grimer RJ. An epidemiological survey of tumour or tumour like conditions in the scapula and periscapular region. SICOT J 2016;2:34. [Google Scholar] |
| 3. | de Souza AM, Bispo Júnior RZ. Osteochondroma: Ignore or investigate? Rev Bras Ortop 2014;49:555-64. [Google Scholar] |
| 4. | Guo XL, Deng Y, Liu HG. Clinical characteristics of hereditary multiple exostoses: A retrospective study of mainland Chinese cases in recent 23 years. J Huazhong Univ Sci Technolog Med Sci 2014;34:42-50. [Google Scholar] |
| 5. | Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features.In Vivo 2008;22:633-46. [Google Scholar] |
| 6. | Tong K, Liu H, Wang X, Zhong Z, Cao S, Zhong C, et al. Osteochondroma: Review of 431 patients from one medical institution in South China. J Bone Oncol 2017;8:23-9. [Google Scholar] |
| 7. | Sivananda P, Rao BK, Kumar PV, Ram GS. Osteochondroma of the ventral scapula causing scapular static winging and secondary rib erosion. J Clin Diagn Res 2014;8:LD03-5. [Google Scholar] |
| 8. | Nascimento AT, Claudio GK. Snapping scapula. Arthroscopic resection of osteochondroma of the subscapularis superomedial angle. Case report and literature review. Rev Bras Ortop 2017;52:220-3. [Google Scholar] |
| 9. | Czajka CM, DiCaprio MR. What is the proportion of patients with multiple hereditary exostoses who undergo malignant degeneration? Clin Orthop Relat Res 2015;473:2355-61. [Google Scholar] |
| 10. | Suresh SS. Superomedial angle osteochondroma of the scapula as a cause of snapping scapula. Kerala J Orthop 2011;25:37-42. [Google Scholar] |
| 11. | Fukunaga S, Futani H, Yoshiya S. Endoscopically assisted resection of a scapular osteochondroma causing snapping scapula syndrome. World J Surg Oncol 2007;5:37. [Google Scholar] |
| 12. | Alatassi R, Koaban S, Almugebel I, Alshehri A. Scapular osteochondroma with winging: A case report. Int J Surg Case Rep 2018;45:138-42. [Google Scholar] |
| 13. | Tittal P, Pawar I, Kapoor SK. Pseudo-winging of scapula due to benign lesions of ventral surface of scapula-Two unusual causes. J Clin Orthop Trauma 2015;6:30-5. [Google Scholar] |
| 14. | Kwon OS, Kelly JI. Delayed presentation of osteochondroma on the ventral surface of the scapula. Int J Shoulder Surg 2012;6:61-3. [Google Scholar] |
| 15. | Jaklitsch MT. Thoracic incisions. In: David JS, Raphael B, Yolanda C, Michael J, Mark JK, Steven M, editors. Adult Chest Surgery. 2nd ed. New York: McGraw-Hill Education; 2014. p. 4-17. [Google Scholar] |
Fulltext Views
4,775
PDF downloads
1,703





