Translate this page into:
Technique for revision reconstruction of a chronic quadriceps tendon re-rupture using Achilles tendon allograft
*Corresponding author: Stephen P Maier II, Department of Orthopedic Surgery, Emory University, Atlanta, Georgia, United States. stephen.p.maier@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Maier S, Pikowski M, Dean EJ, Jackson ER. Technique for revision reconstruction of a chronic quadriceps tendon re-rupture using Achilles tendon allograft. J Musculoskelet Surg Res. 2024;8:291-6. doi: 10.25259/JMSR_106_2024
Abstract
Quadriceps tendon ruptures can substantially diminish the quality of life for patients, imposing significant functional limitations and persistent pain if untreated. Re-injuring the tendon post-fixation presents further surgical challenges, often complicated by scar tissue development and compromised vascular integrity. In this technical note, we describe a novel technique for revising quadriceps tendon fixation failures using an Achilles tendon allograft through bone tunnels and an augmentation with a trans-tendinous pseudo-Pulvertaft weave. Our technique aims to enhance structural integrity and reduce re-injury risk, offering an effective operative solution to challenges associated with quadriceps tendon re-ruptures.
Keywords
Allograft
Quadriceps tendon reconstruction
Quadriceps tendon rupture
Revision surgery
Transtendinous weave
INTRODUCTION
Quadriceps tendon ruptures are rare but significant injuries, particularly for middle-aged and older adults. If left unrepaired, these injuries can substantially diminish a patient’s quality of life.[1,2] The incidence of such ruptures has increased among the aging population, with a rate of 2.82/100,000 from 1997 to 2014. As a result, there has also been a consistent annual rise of 9% in quadricep tendon reconstruction surgeries.[1] Proper surgical management is integral in restoring the functional ability of the extensor mechanism and facilitating a successful return to activity in this population. Furthermore, the utilization of magnetic resonance imaging continues to serve as a critical tool for evaluating the extent and severity of these ruptures [Figure 1].
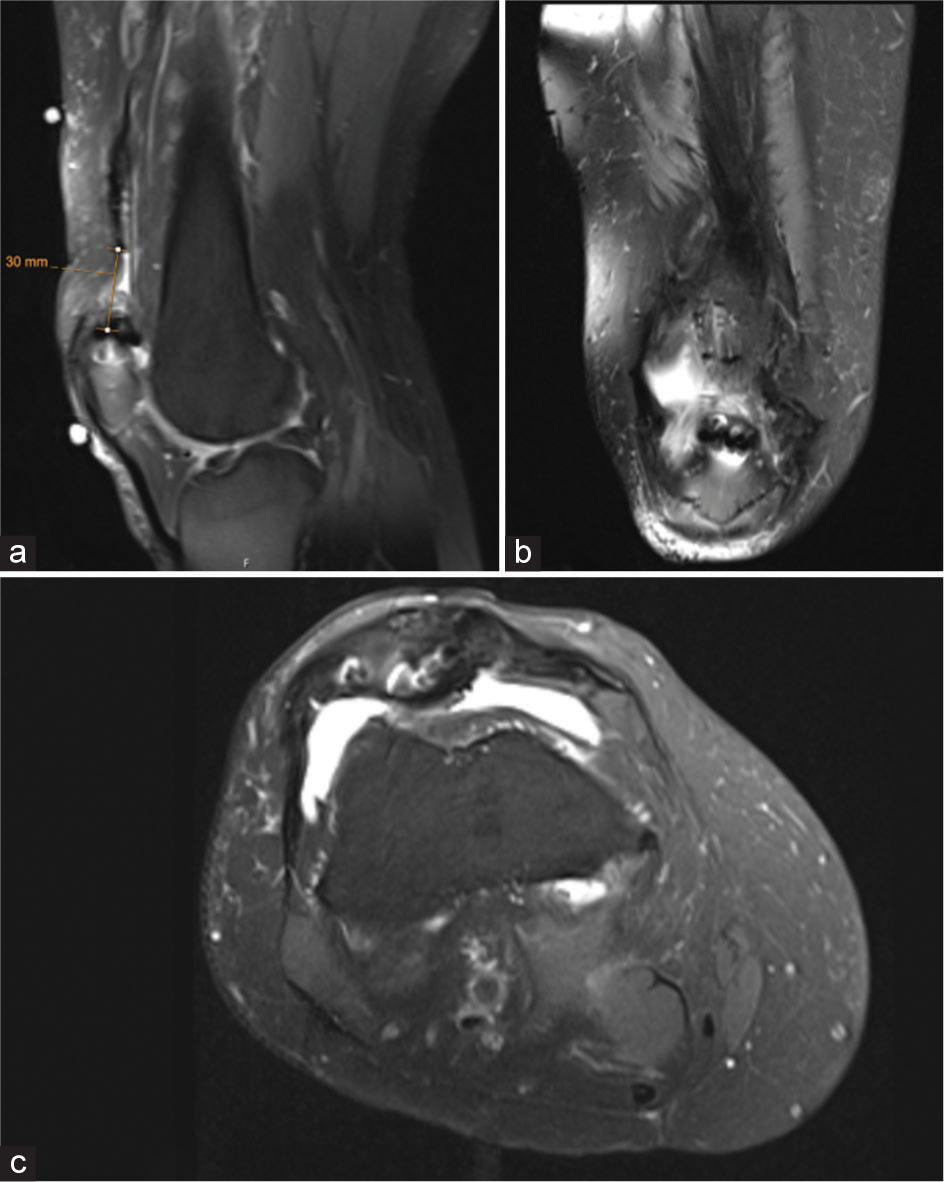
- 67-year-old male following quadriceps tendon repair failure. (a) Sagittal MRI demonstrates the tendon rupture proximal to the patella with 30 mm of retraction of the quadriceps tendon. (b) Coronal and (c) axial views demonstrate evidence of prior suture anchor fixation.
Various techniques are available for repairing or reconstructing quadriceps tendon ruptures, but no definitive gold standard has been established. Consequently, the treatment decision relies on the surgeon’s discretion. Patient-specific factors and tissue quality contribute to guiding treatment decisions. However, considerable variability persists.[1,3] Established techniques for quadriceps repair include suture fixation, anchor fixation, suture-anchor constructs, screw fixation, and patellar bone tunnels. In cases where the tendon integrity is compromised and tendon excursion is limited, reconstructive options using allografts such as Achilles, tibialis anterior, semimembranosus, gracilis, peroneus longus, or iliotibial band tissue should be considered. Autografts using semitendinosus or gracilis have also been described.[4] Synthetic mesh constructs have gained popularity, especially for extensor mechanism reconstruction in patients with a prosthetic knee.[5,6] In cases where persistent gapping or tendon shortening exceeds 5 cm, soft-tissue manipulation options such as V-Y plasty or the Codivilla or Scuderi techniques may be considered.[7-10]
In this technical review, we describe a novel technique for revision reconstruction of a chronic quadriceps tendon re-rupture using an Achilles tendon allograft through bone tunnels and a pseudo-Pulvertaft weave technique through a native remnant tendon.
OPERATIVE TECHNIQUE
Patient positioning
The patient was positioned supine on the operating room table with a hip bump to rotate the lower extremity internally. A tourniquet was placed high on the operative thigh. The operative knee was positioned over a medium triangle in 30° flexion.
Surgical approach
A midline incision was made from the distal thigh to the inferior border of the patella. Subcutaneous dissection exposed the remnant quadriceps tissue and patella while preserving soft tissue on the anterior surface of the patella. The quadriceps tendon was evaluated, and the distal segment proximal to the patella was identified to have roughly 4 cm of abnormal, lax tissue with an intervening scar. This pathologic section was removed. The remaining proximal quadriceps tendon appeared viable and healthy.
The superior pole of the patella was exposed, and all overlying soft tissue was debrided. The patella was prepared to create a rough surface for optimal healing. Three guidewires were then placed equidistantly along the superior pole of the patella, exiting through the inferior pole [Figure 2]. Each pin was over-reamed with a 5.5 mm reamer, and a passing suture was placed into each tunnel after being gently dilated.
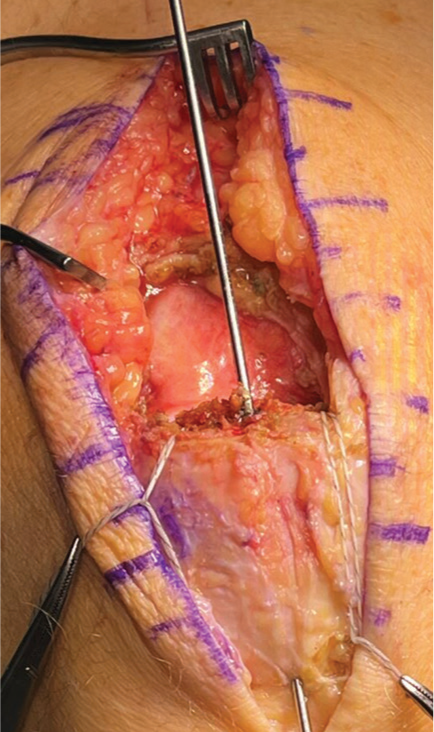
- 67-year-old male following quadriceps tendon repair failure undergoing revision reconstruction. Exposed patella with a middle guidewire in place. Medial and lateral tunnels have been drilled, reamed, and dilated, with passing suture placed in the tunnels.
The tourniquet was deflated, and excellent hemostasis was obtained. The quadriceps tendon excursion was evaluated, demonstrating appropriate length and tension, which obviated the need for a V-Y plasty. A longitudinal incision was made in the tendon roughly 5 cm proximal to the distal edge of the quadriceps tendon stump, and a passing suture was placed in this rent, awaiting the passage of the graft.
Graft preparation
A 20 cm Achilles tendon allograft was selected for this procedure. Grafts used are fresh-frozen from donors under 40 years of age and have more than five years of viable shelf life remaining until expiration. The proximal portion of the graft was left unprepared, while the distal segment of the graft was divided into three equal-sized limbs, each approximately 20 mm in length. A whipstitch was passed up and down each limb [Figure 3]. The limbs were then sized to 5 mm in diameter, and the graft was placed under a moist sponge on tension awaiting introduction.
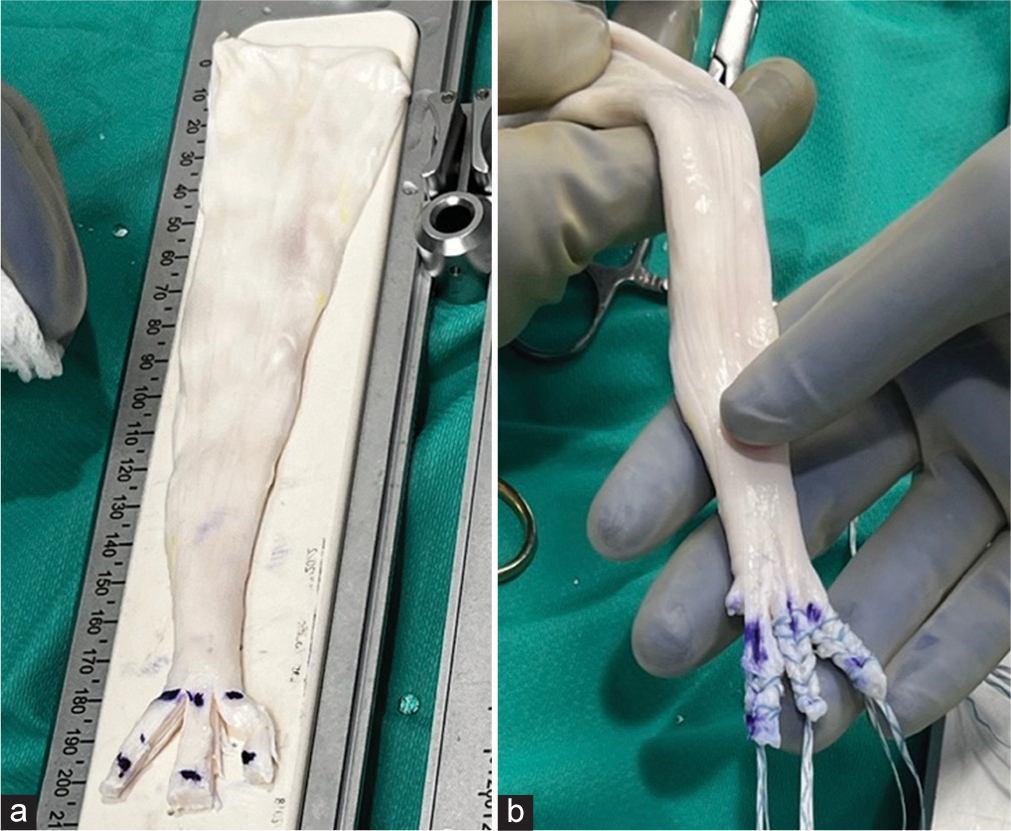
- Preparation of Achilles allograft without bone block demonstrating equal-sized limbs in length and width (a) before and (b) after being whipstitched and sized to 5 mm in diameter.
GRAFT INTRODUCTION
Using previously placed passing sutures, the graft limb whipstitches were shuttled through their respective patellar tunnels. Slack was eliminated from the graft limbs, pulling them taut into their patellar tunnels and anchoring each limb in place using a 5.5 mm polyetheretherketone (PEEK) suture anchor. The proximal end of the graft was passed through the rent in the healthy quadriceps tendon. The graft was tensioned and folded distally over itself. A heavy, nonabsorbable, and ultra-high molecular weight polyethylene (UHMWP) suture was used in a simple interrupted fashion to secure the graft in a spot-welding manner at the rent in the healthy quadriceps tendon and graft interface. A separate, non-absorbable UHMWP suture was used to secure both layers of the medial border of the graft to the native quadriceps tissue in a running fashion. The lateral border of the graft was secured similarly [Figure 4]. The medial and lateral retinacular defects were closed with a non-absorbable UHMWP suture. The knee was taken through 30° flexion to assess the stability of the reconstruction.

- 67-year-old male following quadriceps tendon repair failure undergoing revision reconstruction. (a) Introduction of the allograft using the whipstitch suture limbs of the graft passed through transosseous tunnels in the patella. (b) After graft limbs are shuttled into the patellar tunnels and tensioned, the graft is fixed proximally with a suture anchor. (c) The unprepared proximal portion of the graft is passed through a transverse rent made in the native viable quadriceps tendon. (d) The graft is held using tension sutures at the appropriate length to approximate native quadriceps tension, (e) Then the Achilles graft is folded over itself, tensioned, and fixed with a non-absorbable suture. (f) The wound is closed in a multi-layer fashion before being placed into a controlled range of motion hinged knee brace.
The knee underwent extensive irrigation, antibiotic powder administration in the wound, and tissue closure in layers. A sterile dressing and cylinder cast were placed, and the knee was immobilized in extension.
Post-operative protocol
The operative lower extremity is placed in a cylinder cast and kept strictly in extension (0° of flexion) for eight weeks. Six weeks post-surgery, the patient initiates in-cast isometric exercises, including quadriceps activation (i.e., straight leg raises and quadriceps sets) and global lower extremity conditioning. In week eight, the cast is removed, and the lower extremity is placed into a hinged knee brace. The knee range of motion is initiated and progressed over the subsequent weeks. At month 4, isotonic strengthening begins. The expected total recovery timeline is a minimum of 8 months. Physical therapy has a heavy aquatic focus, and central tenets include strengthening, range of motion, and proprioceptive training.
DISCUSSION
Numerous techniques are available for managing extensor mechanism ruptures. Primary reparative methods may require grafts to enhance the structural integrity in chronic or recurrent tissue injury cases. In this technical review, we present a novel approach for revising quadriceps reconstruction by utilizing an Achilles tendon allograft weaved proximally through a healthy quadriceps tendon in a pseudo-Pulvertaft fashion and passed distally through patellar bone tunnels.
When a tendon is injured, the healing process initiates the formation of a collagen fiber matrix, resulting in scar tissue development.[11] However, the newly formed tendon lacks the same tensile strength and vascularization as the native tendon, making it susceptible to re-injury.[11,12] These alterations in the tendon composition can pose challenges during repair, such as difficulty in tissue approximation and increased stress on the repair site. To address these issues and achieve a higher quality reconstruction with reduced risk of re-injury, an Achilles tendon allograft is proposed for tendon augmentation.[7] Factors contributing to failed repairs may include inadequate initial fixation, compromised tissue quality, and infection.[13] Establishing a recommended standard of care could help prevent a subset of avoidable failures.
A suture anchor repair technique was previously described by Paez et al. for recreating the quadriceps tendinous footprint across the superior pole of the patella.[7] This involved utilizing a V-Y plasty to allow for necessary tendon excursion, along with an Achilles allograft overlaid superficially for biological augmentation. Our technique adopts similar principles, employing three evenly-spaced bone tunnels to maximize the potential healing surface. The Achilles allograft augmentation is paired with adequate suture repair, utilizing the graft in a transosseous fashion for double fixation. This involves tying the suture tails over the inferior pole of the patella and securing the graft limbs in the superior pole using interference fixation. In addition, we employ a transtendinous weave to integrate and incorporate the graft and tendon, enabling proper reduction of the remaining quadriceps tendon to the patella. This approach ensures a robust fixation, resembling a belt-over-suspenders style, connecting graft-to-graft, tendon-to-tendon, and graft-to-tendon.
A reconstruction technique utilizing the ipsilateral semitendinosus tendon as an autograft has been described. This involves passing the tendon through a transverse tunnel in the patella and securing it to the freshly debrided native quadriceps tendon using strong, absorbable sutures.[4] Additional fixation is achieved by suturing the graft to the periosteum of the patellar tunnel exit holes. Our technique passes the graft through longitudinal patellar bone tunnels to maximize the graft-to-patella healing surface. Furthermore, a rent is created in the native quadriceps tendon, allowing it to be folded over itself to double the graft thickness. The doubled tendon is then secured with spot welding suture fixation and attached to the medial and lateral borders of the native tendon, facilitating excellent fixation and integration of the donor tissue with the native tissues.
A technique proposed by Kunze et al. involves using a trapezoidal plug of Achilles tendon allograft inserted into the patella through an 8 cm standard anterior approach.[14] This technique aims to minimize soft-tissue trauma and donor site morbidity by promoting bone-to-bone healing for improved fixation, as opposed to tendon-to-bone healing. However, the authors acknowledge the potential risk of inadequate reduction and stabilization of the graft. In our described technique, although a slightly longer incision is required to expose the entire patella, donor site morbidity is comparatively reduced by employing the proper technique in drilling bone tunnels to minimize the risk of patella fracture. The extended incision also allows for additional fixation over the inferior pole of the patella, providing further protection against tendon-bone healing failure. Furthermore, our technique avoids a sizeable bony defect in the patella, thereby reducing the risk of anterior knee pain or patellar fracture. We believe that our technique offers an excellent restoration of the extensor mechanism with secure fixation, while being mindful of potential iatrogenic complications.
It is important to consider the chronicity and retraction of these tears, as well as the quality of the tissue at the time of reconstruction. The primary goal of our technique is to restore function and alleviate pain, understanding that a certain degree of extensor lag and associated weakness may persist. As suggested by Oliva et al., this technique proves valuable in cases of chronic quadriceps tears older than six weeks, defects longer than 2 cm, failed previous repairs, and situations where an appropriate approximation of the tendon ends cannot be achieved.[4]
This technique is not without risk. Potential complications include infection, stiffness, patella fracture, and reconstruction failure. It is critical to address these risks preemptively, which we do with perioperative antibiosis (both systemic and local), controlled post-operative range of motion parameters with a specific rehabilitation protocol, longer incisions with greater exposure to facilitate proper placement and spacing of the patellar bone tunnels, and optimal fixation with durable sutures, PEEK anchors, and meticulous soft-tissue handling.
CONCLUSION
This review presents a novel approach to the revision reconstruction of chronic quadriceps tendon ruptures. Our technique involves incorporating an Achilles tendon allograft through transosseous patellar bone tunnels and utilizing a pseudo-Pulvertaft weave technique within the native remnant tendon. Re-injured tissue offers operative challenges such as compromised vascular quality and diminished tensile strength. Given the absence of a standardized technique and an increasing prevalence of quadriceps tendon ruptures, our proposed approach offers a reconstructive option to enhance patient outcomes and minimize complications. The objective of this technique is to enhance structural integrity and reduce the risk of re-injury, and we believe the post-operative results provide supportive evidence of its effectiveness.
AUTHORS’ CONTRIBUTIONS
EJ and SM contributed to the conception and technique design. SM, MP, and ED contributed to the literature search, manuscript preparation, and manuscript editing and reviewing. EJ also contributed to the manuscript editing and reviewing. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board approval is not required.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained appropriate verbal patient consent. In the verbal consent, the patient has agreed to the use of his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit.
References
- The increasing incidence of surgically treated quadriceps tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2019;27:3644-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy, bony pelvis and lower limb: Thigh quadriceps muscle In: StatPearls. Treasure Island, FL: StatPearls Publishing LLC; 2024.
- [Google Scholar]
- Allograft reconstruction for extensor mechanism injuries. J Knee Surg. 2014;27:489-96.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic quadriceps tendon rupture: Quadriceps tendon reconstruction using ipsilateral semitendinosus tendon graft. J Orthop Surg Res. 2023;18:355.
- [CrossRef] [PubMed] [Google Scholar]
- A modified surgical technique of patellar tendon reconstruction in total knee arthroplasty using achilles tendon allograft. Arthroplast Today. 2022;14:22-8.
- [CrossRef] [PubMed] [Google Scholar]
- Synthetic mesh vs. allograft extensor mechanism reconstruction in total knee arthroplasty-a systematic review of the literature and meta-analysis. Knee. 2018;25:2-7.
- [CrossRef] [PubMed] [Google Scholar]
- Suture anchor repair with V-Y plasty and achilles allograft augmentation for chronic quadriceps tendon injury. Arthrosc Tech. 2020;9:e1033-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quadriceps tendon rupture. J Am Acad Orthop Surg. 2003;11:192-200.
- [CrossRef] [PubMed] [Google Scholar]
- Ruptures of the quadriceps tendon; study of twenty tendon ruptures. Am J Surg. 1958;95:626-34.
- [CrossRef] [PubMed] [Google Scholar]
- Acute and old ruptures of the extensor apparatus of the knee in adults (excluding knee replacement) Orthop Traumatol Surg Res. 2013;99(1 Suppl):S67-76.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical, biological, and biomaterials perspective into tendon injuries and regeneration. Tissue Eng Part B Rev. 2017;23:44-58.
- [CrossRef] [PubMed] [Google Scholar]
- Biologics for tendon repair. Adv Drug Deliv Rev. 2015;84:222-39.
- [CrossRef] [PubMed] [Google Scholar]
- Tendon and ligament regeneration and repair: Clinical relevance and developmental paradigm. Birth Defects Res C Embryo Today. 2013;99:203-22.
- [CrossRef] [PubMed] [Google Scholar]
- Trapezoidal achilles tendon allograft plug for revision quadriceps tendon repair with a large tendon defect. Arthrosc Tech. 2019;8:e1031-6.
- [CrossRef] [PubMed] [Google Scholar]







