Translate this page into:
The accuracy of intraoperative O-arm imaging in assessing thoracolumbar pedicle screws placement
*Corresponding author: Felipe Aguilar-Chavez, Department of Spine Surgery, Star Medica, Chihuahua, Mexico. felipemj23@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aguilar-Chavez F, Arellanes Chavez CA, Martinez Tapia ME, Martinez-Loya C, Gaytan Medina CM. The accuracy of intraoperative O-arm imaging in assessing thoracolumbar pedicle screws placement. J Musculoskelet Surg Res. 2024;8:227-31. doi: 10.25259/JMSR_132_2024
Abstract
Objectives:
Pedicle screw fixation in spine surgery is often considered the gold standard due to its biomechanical advantages. Complications such as screw misplacement may arise during the procedure, leading to severe consequences. Intraoperative 2D/3D imaging system images or a post-operative computed tomography (CT) scan are employed to assess this. This study aimed to determine the agreement between these two imaging systems to evaluate the placement of transpedicular screws using the Zdichavsky classification.
Methods:
Image data from the intraoperative 2D/3D imaging system and CT scans of patients undergoing spine surgery at the neurosurgery department were collected from March 2021 to May 2022. The position of transpedicular screws was evaluated using the Zdichavsky classification.
Results:
Images from 19 patients, 7 males (36.84%) and 12 females (63.16%), aged 28–77 years, were gathered. A total of 131 transpedicular screws were evaluated, ranging from 4 to 10 screws per patient. In the post-operative CT scan, 123 screws were classified as type Ia (93.89%), seven screws as type Ib (5.34%), and one screw as type IIb (0.76%). With the navigation system, 125 screws were classified as type Ia (95.42%), five as type Ib (3.82%), and one screw as type IIb (0.76%).
Conclusion:
It was demonstrated that intraoperative 2D/3D system images can be used to assess screw placement without the need for post-operative studies such as CT scans.
Keywords
Accuracy
Navigation
Pedicle screw
Spine
Surgery
Scoring system Zdichavsky classification
INTRODUCTION
Pedicle screw fixation is a common procedure in spinal surgery and is often considered the gold standard, especially for its adequate fixation throughout the vertebra.[1] Successful fixation requires a stable implant-bone interface. The proximity of neural structures limits the available bone surfaces for instrumentation. In addition, the bone’s size and shape influence the material that can be used. Larger pedicles allow for the placement of larger pedicle screws, increasing fixation stability and strength. It is crucial to consider this variation among patients. At present, modern imaging systems enable pre-operative measurements of the optimal length and thickness of the screw.[2]
In recent decades, the placement of transpedicular screws continues to be associated with complications of mispositioning.[3,4] While it may be asymptomatic in most cases, it can significantly damage neurovascular structures. With various conventional placement techniques, a defined incidence rate of misplacement in the thoracolumbosacral region ranges from 15% to 30%.[5] This can be prevented with proper placement using navigation techniques (StealthStation™) and verification using an intraoperative 2D/3D imaging system (O-arm™).[6] If this technology is not available, the surgeon verifies screw placement with an intraoperative 2D fluoroscopy technique or post-operative computed tomography (CT) scan when a freehand technique is performed.[1] However, another procedure is required for screw repositioning if necessary.
There are multiple classifications for assessing proper pedicle screw placement, evaluating this in the axial plane toward medial and lateral directions, whether they are within or outside the pedicle or body. However, there is no consensus on which classification to use or which is the most suitable.[7,8]
Recent research demonstrates that perforations exceeding 4 mm in the medial wall of the pedicle could lead to neurological injuries. However, cadaveric studies suggest that perforations <2 mm in the medial pedicle wall are safe. Therefore, most surgeons consider this a safe perforation zone.[9]
The Zdichavsky classification[10,11] is a tool utilized to determine screw placement, comprising six types. Type Ia retains half or more of the screw within the pedicle and half or more within the vertebral body. In contrast, type Ib has over half of the screw laterally outside the pedicle and half within the vertebral body. Type IIa maintains half or more of the screw within the pedicle and more than half protruding laterally from the vertebral body, and type IIb is characterized by having half or more of the screw’s thickness within the pedicle, with its tip crossing the midline of the vertebral body. Type IIIa depicts more than half of the screw outside laterally, both the pedicle and the vertebral body, whereas type IIIb exhibits more than half of the screw outside the pedicle through the medial cortex, with its tip crossing the midline of the vertebral body [Figure 1].[10,11]
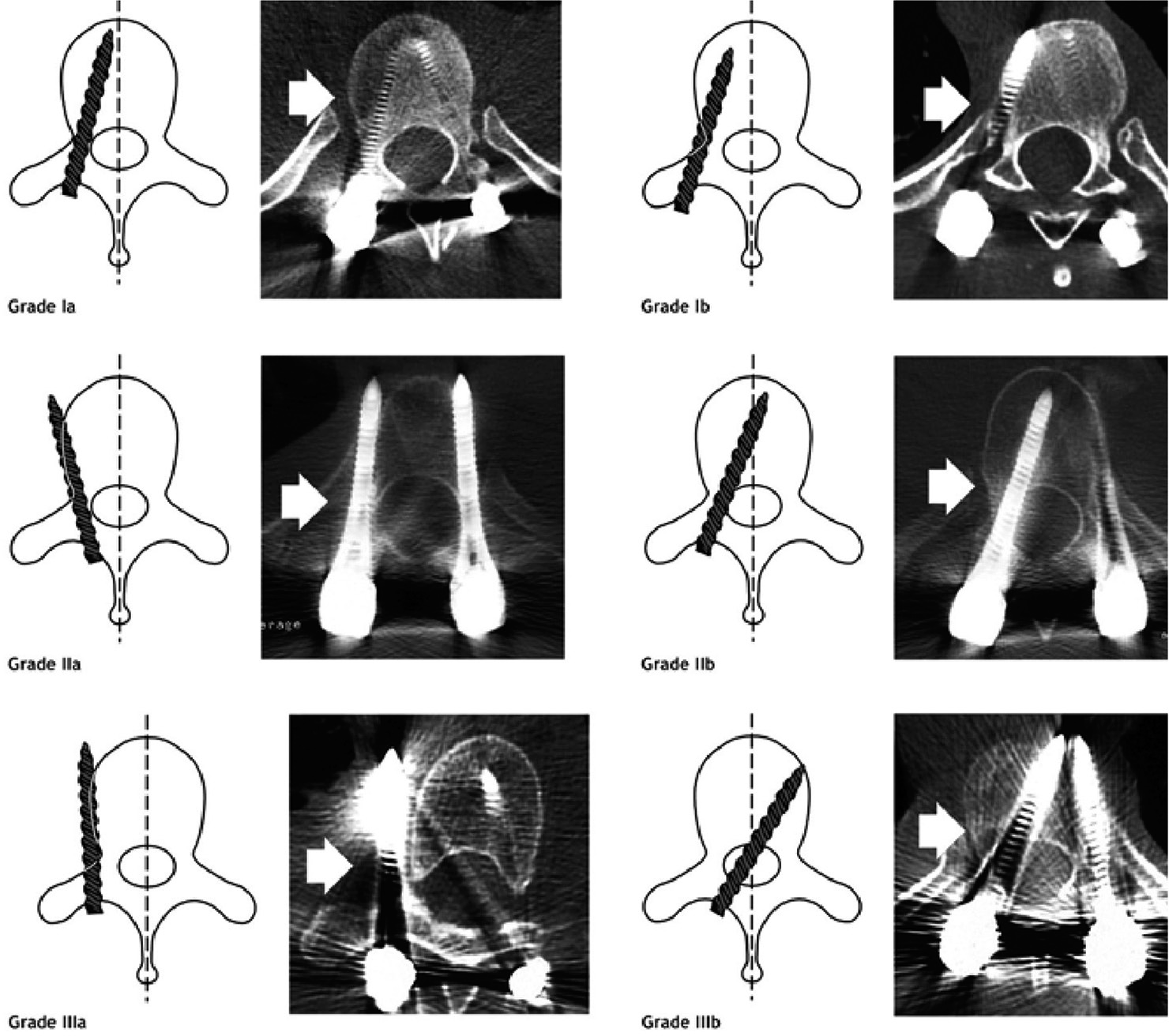
- Zdichavsky et al.’s classification (adapted from Zdichavsky et al.) depicting grades Ia to IIIb with schematic examples of each grade displayed alongside. The white arrow shows the position of the screw.
The objective of this study was to assess the level of agreement between intraoperative O-arm imaging after placing the screws and post-operative CT scan for evaluating the accurate placement of thoracolumbar transpedicular screws using the Zdichavsky classification.
MATERIALS AND METHODS
A cross-sectional, analytical, observational, and retrospective study was conducted involving patients undergoing spinal surgery by three senior spine surgeons (CA, JF, and AP) at the Neurosurgery Department from March 2021 to May 2022. Sample size calculation utilized the formula for proportion with an infinite population, considering an expected proportion of 80%, a confidence level of 95%, and a precision of 7. The statistical software EPIDAT (version 3.5) was utilized, resulting in a minimum sample size of 126 screws.
Only sex, age, and images from the required studies were collected from the patient’s clinical record. The study included patients aged 15 years and older, of any sex, with complete intraoperative O-Arm™ (O-arm, Medtronic, Minneapolis, Minnesota, USA) images of all placed screws and complete post-operative CT scans visualizing all screws, the surgeon’s criteria for performing an O-arm scan before placing the screws and post-operative CT scan was not assessed. Patients were excluded if O-arm and/or CT scan images exhibited artifacts or were not visualized correctly.
Intraoperative O-arm images after placing the screws and post-operative CT scan images were collected in December 2022 from the imaging registry for all patients meeting the inclusion criteria. Subsequently, the position of all screws was determined according to the Zdichavsky classification in both studies, conducted by a single observer. Zdichavsky’s classification was chosen, among others, for its widespread use and reproducibility in determining the correct placement of transpedicular screws.[8] Subsequently, the data were transferred to a spreadsheet, and the corresponding statistical analysis was conducted using Epi Info™ software version 7.2. Descriptive analysis was performed using absolute and relative frequency measures. Summary and dispersion measures were utilized for quantitative variables, and the Kappa index was calculated to assess the agreement between the two imaging methods.
RESULTS
Images were collected from a total of 19 patients, comprising 131 transpedicular screws. Among these patients, 7 were male (36.84%) and 12 were female (63.16%). The age of the patients ranged from 28 to 77 years, with a mean age of 57 ± 14 years. The number of screws per patient ranged from 4 to 10, with three patients having 4 screws (15.79%), seven patients with 6 screws (31.58%), six patients with 8 screws (31.58%), one patient with 9 screws (5.26%), and two patients with 10 screws (10.52%), with a mean of 7 ± 2 screws.
Using the Zdichavsky classification system, the 131 screws were categorized with post-operative CT and intraoperative O-arm images randomly by an observer. In the post-operative CT, 123 screws were identified as Type Ia (93.89%), seven screws as Type Ib (5.34%), and one screw as Type IIb (0.76%) [Table 1]. In intraoperative O-Arm images, 125 screws were classified as Type Ia (95.42%), five as Type Ib (3.82%), and one screw as Type IIb (0.76%) [Table 1]. A kappa value of 0.55 was observed for the concordance analysis, indicating a considerable level of agreement, with a confidence interval of 23–87% and P = 0.00 for statistical significance [Table 2].
| Zdichavsky | CT scan (%) | O-Arm (%) |
|---|---|---|
| Ia | 123 (93.89) | 125 (95.42) |
| Ib | 7 (5.34) | 5 (3.82) |
| IIb | 1 (0.76) | 1 (0.76) |
| Total | 131 (100.00) | 131 (100.00) |
CT: Computed tomography
| O-Arm | CT Scan | ||
|---|---|---|---|
| Ia | Ib | IIb | |
| Ia | 121 | 4 | 0 |
| Ib | 2 | 3 | 0 |
| IIb | 0 | 0 | 1 |
CT: Computed tomography
DISCUSSION
Innovative navigation techniques in spinal surgery have greatly contributed to minimizing the incidence of incorrect pedicle screw placement, especially when employed by experienced spinal surgeons.[12] The superiority of these systems is particularly beneficial when applied to patients with anatomical variations and in complex surgeries.[13]
This study compared two diagnostic imaging studies, evaluating the placement of transpedicular screws in an axial plane and categorizing them using the Zdichavsky classification. The Landis and Koch Kappa interpretation system was utilized for statistical evaluation.[14] When comparing the two studies, a moderate agreement between them was demonstrated. However, the confidence interval does not fall within the high-reliability standards, as there is a discrepancy of 23%, which indicates a continuing difference in a small percentage.
Ghodasara et al. show that following spinal instrumentation surgery, indications for performing a CT scan include assessing the condition and placement of the implant, observing the development and status of bone fusion, and identifying any issues such as peri-implant osteolysis, hidden fractures visible only through imaging, and the presence of soft-tissue accumulations.[15] Previously, it was shown that performing only post-operative CT in symptomatic patients is advisable to verify the screw position; however, this would entail an additional procedure for screw repositioning.[16] In contrast, with intraoperative images displayed using the O-Arm, there is the opportunity to reposition the implant during the same procedure, thereby reducing surgical team and patient exposure to radiation and other surgery.[17]
It is worth emphasizing that in both tests, a high percentage of correct placement was demonstrated in our sample due to the navigation technique using StealthStation™ and O-arm, as type Ia, considered appropriate placement, was observed in 93.89% on CT and 95.42% on O-arm images, which is consistent with literature reports.[18,19]
The most notable discrepancy was observed between type Ia and Ib, as these are the two most stable types within the classification without involving a violation of the medial cortex or screw instability with a similar screw direction. Similarly, adequate agreement was observed in type IIb in both tests. In this type, there is a more pronounced screw angulation, and it crosses the midline of the vertebral body, violating the medial wall of the pedicle by <50% of the screw thickness. Therefore, it is demonstrated that in higher types of classification where incorrect screw placement, especially toward the medial wall, is evident, it is more likely to find agreement.
It was observed that there is greater agreement between the two imaging studies in types of the Zdichavsky classification where incorrect placement is more evident, such as violating pedicle walls or crossing the midline of the vertebral body.
Limitations
A limitation of the study is that, due to the high rate of accurate placement provided by O-arm navigation, we lack a comparison point for Zdichavsky types IIa, IIIa, and IIIb since they were not present in the present study. The utilization of post-operative CT for assessing transpedicular screws remains questionable, particularly in asymptomatic patients when the control X-ray shows proper placement.
CONCLUSION
As mentioned earlier, a follow-up study such as CT is important in symptomatic patients postoperatively and when the control X-ray shows screw malposition. However, it was demonstrated that intraoperative O-arm images can be used as a post-operative control for screw position with minimal risk of inaccuracies and half radiation dose than CT scan.
Recommendations
Although patient clinical data were not the focus of this study, future research with a larger sample size and representation of all classification types is necessary to clarify these uncertainties. We also recommend including more clinical issues of the patients.
AUTHORS’ CONTRIBUTIONS
FA conceived of the presented idea. FA and CGM collected the data. CMT and FA did the statistical analysis. FA wrote the manuscript with support from CML and CMT. CA reviewed the paper and made corrections with support from FA. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This retrospective study was approved by the Hospital and Institution Committee and the Investigation Board dated July 08, 2022, and November 15, 2022, [HCINVESTIGACION/INTERNO-3/2022], and begin the recollection of data in December 2022 from the imaging registry for all patients undergoing spinal surgery at the Neurosurgery Department in the period of March 2021 to May 2022.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that no artificial intelligence (AI)-assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000;82:1458-76.
- [CrossRef] [PubMed] [Google Scholar]
- La columna según Rothman-Simeone y Herkowitz. In: Amolca. Vol 2. Netherlands: Elsevier; 2020. p. :1194-5.
- [Google Scholar]
- Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: A literature review of 35,630 pedicle screws. Neurosurg Focus. 2011;31:E8.
- [CrossRef] [PubMed] [Google Scholar]
- Pedicle screw loosening: A clinically relevant complication? Eur Spine J. 2015;24:1005-16.
- [CrossRef] [PubMed] [Google Scholar]
- Pedicle screw placement in spinal neurosurgery using a 3D-printed drill guide template: A systematic review and meta-analysis. J Orthop Surg Res. 2020;15:1.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoperative navigation in spine surgery: Effects on complications and reoperations. World Neurosurg. 2022;160:e404-11.
- [CrossRef] [PubMed] [Google Scholar]
- Methods to determine pedicle screw placement accuracy in spine surgery: A systematic review. Eur Spine J. 2015;24:990-1004.
- [CrossRef] [PubMed] [Google Scholar]
- Pedicle screw placement accuracy impact and comparison between grading systems. Surg Neurol Int. 2017;8:131.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15:11-4.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of pedicle screw placement in thoracic spine fractures-Part II: A retrospective analysis of 278 pedicle screws using computed tomographic scans. Eur J Trauma. 2004;30:241-7.
- [CrossRef] [Google Scholar]
- Accuracy of pedicle screw placement in thoracic spine fractures-Part I: Inter-and intraobserver reliability of the scoring system. Eur J Trauma. 2004;30:234-40.
- [CrossRef] [Google Scholar]
- Accuracy and reliability of spinal navigation: An analysis of over 1000 pedicle screws. J Orthop. 2020;18:197-203.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine (Phila Pa 1976). 2012;37:E473-8.
- [CrossRef] [PubMed] [Google Scholar]
- The measurement of observer agreement for categorical data. Biometrics. 1977;33:159.
- [CrossRef] [Google Scholar]
- Postoperative spinal CT: What the radiologist needs to know. Radiographics. 2019;39:1840-61.
- [CrossRef] [PubMed] [Google Scholar]
- Pedicle screw accuracy in thoracolumbar fractures-is routine postoperative CT scan necessary? BMC Musculoskelet Disord. 2021;22:986.
- [CrossRef] [PubMed] [Google Scholar]
- Implications of navigation in thoracolumbar pedicle screw placement on screw accuracy and screw diameter/pedicle width ratio. Brain Spine. 2023;3:101780.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus. 2014;36:E1.
- [CrossRef] [PubMed] [Google Scholar]
- Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: Comparison between free-hand and O-arm based navigation techniques. Eur Spine J. 2011;20:875-81.
- [CrossRef] [PubMed] [Google Scholar]







