Translate this page into:
The compliance with radiation protection and knowledge about radiation exposure among the orthopedic operating room personnel in Saudi Arabia
*Corresponding author: Abdulrahman H. Almalki, College of Medicine, King Saud University, Riyadh, Saudi Arabia. aahhjj5567@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Almalki AH, Almalki MA, Alballa RS, Alshaygy IS, Alrabai HM. The compliance with radiation protection and knowledge about radiation exposure among the orthopedic operating room personnel in Saudi Arabia. J Musculoskelet Surg Res 2021;5(3):178-86.
Abstract
Objectives:
There is a rapid advancement in surgical techniques requiring real-time visualization and intraoperative X-ray utilization, leading to a higher radiation exposure among operating room (OR) staff. Taking preventive measures and reducing the unnecessary radiation exposure for the patient and the OR staff is essential. The study aimed to assess the compliance with using radiation protection equipment, as well as assessing the level of knowledge about radiation exposure among the orthopedic OR staff.
Methods:
This is a cross-sectional study that was conducted in Saudi Arabia. A 19-Item questionnaire that was developed and validated by Jentzsch et al. was sent to the emails of all the registered members of the Saudi Orthopedic Association, orthopedic physicians, OR nurses, and radiology technicians were included in the study. A Correlation procedure was performed to determine the relationship between knowledge and compliance scores.
Results:
We recruited 242 orthopedic OR personnel, 110 (45.5%) showed good knowledge and 120 (49.5%) showed good compliance. Lead apron was the most commonly used equipment, lead goggles use was the least. Females, radiology technicians, and sports and/or arthroplasty surgeons showed better compliance scores.
Conclusion:
The study reveals inadequate knowledge and compliance among OR staff regarding radiation protection. Therefore, we recommend providing training programs to minimize radiation hazards.
Keywords
Compliance
Fluoroscopy
Knowledge
Orthopedic
Operating room
Radiation
INTRODUCTION
There is a rapid advancement in instrumentation and surgical techniques requiring more real-time visualization and intra-operative X-ray utilization, leading to higher radiation exposure among operating room (OR) staff. Orthopedic OR personnel are exposed to radiation directly from the beam source and indirectly from the scattered radiation.[1] Among those who are significantly affected are trauma surgeons in which the use of X-ray and real-time visualization is essential.
Adding to this, these surgeons are often uneducated regarding the physical and medical properties of radiation.[2] However, another study found that registrars in spinal sub-specialties are exposed to significantly higher doses of ionizing radiation per case and cumulative doses of ionizing radiation per month than non-spinal registrars.[3] Certain operations have been shown to carry a higher risk of radiation exposure than others. The utilization of fluoroscopy in the installment of thoracolumbar pedicle screw makes spine surgeons at significantly greater ionizing radiation levels than other non-spinal musculoskeletal procedures using a fluoroscope.[4,5] Among procedures requiring fluoroscopic utilization, closed locked femoral nailing is found to be accountable for a significant level of scattered radiation exposure to primary surgeons. Advancements in image intensification technology contributed to minimizing the fluoroscopic time required for similar procedures, hence less exposure to the OR staff.[6]
Sources of radiation in the OR include the primary beam, which is located between the beam generator and the image intensifier. The other source would be the scattered radiation from the patient or any object in the way of the primary beam.[7]
Irreparable DNA damage has been shown to be caused by low-dose X-ray radiation.[8] The International Commission on Radiological Protection (ICRP) recommends that effective dose is limited to 20 mSv/year, averaged over defined periods of 5 years, with no single year exceeding 50 mSv, and the equivalent dose to the hands and feet should not exceed 500 mSv/year, 150 mSv for the lens of the eyes.[9] The Radiation Effects Research Foundation found a relative risk of 1.6 for solid organ cancer after 1 Sv of radiation exposure and a 5% risk of mortality from cancer. Therefore, the ICRP effective dose is limited to 20 mSv/year, which means that we will need 50 years before we reach 1 Sv of cumulative radiation. Despite these recommendation limits, many studies have shown an increased incidence of malignancies among orthopedic surgeons who were exposed to radiation, which could be associated with poor radiation safety practices or frequency of intraoperative fluoroscopy use, the proximity, and duration of intraoperative fluoroscopy use.[10,11] Despite these well-known risks and hazards of radiation exposure, there is a significant lack of knowledge of basic principles of radiation protection among orthopedic trainees, and orthopedic trauma surgeons specifically.[12,13] This motivated us to perform a study that assesses the compliance with radiation protection and knowledge about radiation exposure among the orthopedic OR staff, which we believe will assist health-care institutes to provide targeted training programs for healthcare workers.
MATERIALS AND METHODS
This is a cross-sectional study conducted over the period from January 2021 to May 2021. The study included practicing orthopedic physicians, orthopedic OR nurses, and radiology technicians who operate the X-ray machine in the OR. The sampling technique was by convenience and the data were collected through an electronic survey that was sent to all the registered emails of the members of the Saudi Orthopedic Association (SOA). The survey was open for accepting answers for 8 weeks before it was closed. Responses from undergraduates and medical interns were excluded as well as responses from non-orthopedic physicians. Due to the lack of OR nurses and radiology technicians in the SOA registry, we distributed a portion of the surveys manually in different hospital in the city of Riyadh, Saudi Arabia.
A validated questionnaire that was originally developed by Jentzsch et al. was used in this study.[14] The questions included were about gender, job position, sub-specialty (when applicable), years of practice, as well as ten questions to assess knowledge about radiation protection and hazards. The questions assessed whether certain practices were associated with less or more radiation. Questions (I–III) assessed knowledge about radiation exposure with vertical and horizontal positioning of the C-arm and the practitioner [Figures 1-3]. Question (IV) assessed knowledge about radiation exposure with anteroposterior versus lateral view. Question (V) assessed knowledge about radiation exposure to eyes and hands, and question (VI) assessed knowledge about radiation exposure according to type of surgery (instrumentation of the spine vs. nailing of the femur). Question (VII) assessed knowledge about voltage and current, question (VIII) assessed knowledge about collimation, question (IX) assessed knowledge about distance, and question (X) assessed knowledge about maximal partial body radiation exposure. The total knowledge score was obtained by adding the ten questions and a score range from 0 to 10 had been generated, which meant that the higher the score, the higher the knowledge regarding radiation exposure in the OR. We classified the sample as having good or poor knowledge according to their score compared to the mean: 4.07. The mean score was obtained by adding up the scores and dividing the total by the number of scores, respondents who scored between 5 and 10 were identified as having good knowledge about radiation exposure, while poor knowledge was defined as a score below 5 points.

- Vertical 1. The safe position of the image intensifier close to the patient as seen in (a), while the incorrect alignment with the image intensifier far away from the patient is shown in (b).

- Vertical 2. The safe position of the image intensifier above the patient as seen in (a), while the incorrect positioning with the image intensifier under the patient is shown in (b).

- Horizontal positioning of the image intensifier and the X-ray tube. The safe position of the surgeon on the image intensifier’s side as in (a), the incorrect position of the surgeon on the X-ray tube as seen in (b).
Compliance toward radiation protection was assessed using four items (lead apron, thyroid shield, dosimetry, and protective eye goggles), with two possible answers “≥50% of the times wearing a protection tool” scored with 2 points and “<50% of the times wearing a protection tool” scored with 1 point. The total compliance score has been obtained by adding the four items and a possible score range from 4 to 8 had been generated, which indicates that the higher the score, the higher the compliance with radiation protection. The goal was to determine the overall compliance rate rather than the compliance rate for specific group, as they are all represent the orthopedic OR personnel; hence, we used the mean score (mean: 5.64) as a cutoff point to determine the level of compliance, participants were considered non-compliant if the score range was from 4 to 5.64 points and compliant if the score range was from 5.65 to 8 points.
Descriptive statistics were summarized using numbers and percentages. Variables were compared to the knowledge and compliance scores using Mann–Whitney U-test or Kruskal– Wallis test, whenever appropriate. Normality test had been performed by using Kolmogorov–Smirnov test or Shapiro– Wilk test. The data followed an abnormal distribution. Thus, non-parametric tests were applied. A P-value cutoff point of 0.05 at 95% CI was used to determine statistical significance. A correlation procedure was performed to determine the linear relationship between knowledge and compliance scores. Data analyses were carried out by a biostatistician and performed using Statistical Packages for the Software Sciences version 21 (Armonk, New York, IBM Corporation).
RESULTS
We recruited 242 orthopedic OR personnel to measure their compliance with radiation protection and their knowledge about radiation exposure. Table 1 presented the socio-demographic characteristics of the respondents. Orthopedic physicians represented 76% of the sample, while radiology technicians accounted for 12.4% and 11.6% were orthopedic OR nurses. The majority were males (71.1%). Nearly one-third (32.2%) had <5 years in practice and 29.8% had 5–10 years of experience. In addition, the most commonly mentioned rank was resident (32.2%), followed by consultant (23.1%) and fellow/specialist (20.7%). Of the 106 consultants and fellow/specialist 22.6% were general orthopedics, followed by pediatric orthopedics (20.8%) and sports and/ or arthroplasty surgeons (20.8%), while oncology surgeons were the least (7.5%). The majority of the sample (90.9%) believes that they need further training regarding radiation protection and hazards, and 66.1% said that there was a lack of radiation protection equipment when needed.
| Study variables | n(%) |
|---|---|
| Gender | |
| Male | 172 (71.1) |
| Female | 70 (28.9) |
| Have you ever needed radiation protection tools and didn’t find them available? | |
| Yes | 160 (66.1) |
| No | 82 (33.9) |
| Do you believe that you need further training regarding radiation hazards? | |
| Yes | 220 (90.9) |
| No | 22 (09.1) |
| Years in practice | |
| <5 years | 78 (32.2) |
| 5–10 years | 72 (29.8) |
| 11–15 years | 50 (20.7) |
| >15 years | 42 (17.4) |
| Position | |
| Resident | 78 (32.2) |
| Fellow/specialist | 50 (20.7) |
| Consultant | 56 (23.1) |
| OR nurse | 28 (11.6) |
| Radiology technician | 30 (12.4) |
| Subspecialty of the orthopedic consultants and fellow/specialist* | |
| General orthopedics | 24 (22.6) |
| Pediatric orthopedics | 22 (20.8) |
| Sports and/or arthroplasty | 22 (20.8) |
| Trauma and reconstructive surgery | 20 (18.9) |
| Spine | 10 (9.4) |
| Orthopedic oncology | 8 (7.5%) |
A total of 110 (45.5%) showed good level of knowledge [Figure 4], the correct answer was chosen 986 (40.7%) times [Table 2]. The top three knowledge indicators where the majority of respondents demonstrated correct answers were; type of surgery, as 140 (57.9%) answered that nailing of the femur has more radiation exposure than instrumentation of the spine. That was followed by distance, where 57% answered that doubling the distance from the X-ray machine leads to a four-fold reduction in radiation exposure, 132 (54.5%) answered that the proper positioning of the image intensifier is close to the patient as shown in Figure 1.
| Knowledge indicator | Incorrect answer n(%) |
Correct answer n(%) |
Total n(%) |
|---|---|---|---|
| Voltage and current | 202 (83.5) | 40 (16.5) | 242 (100) |
| Collimation | 198 (81.8) | 44 (18.2) | 242 (100) |
| Maxima partial body radiation | 184 (76.0) | 58 (24.0) | 242 (100) |
| C-arm Horizontal | 154 (63.6) | 88 (36.4) | 242 (100) |
| X-ray view | 152 (62.8) | 90 (37.2) | 242 (100) |
| C-arm Vertical 2 | 116 (47.9) | 126 (52.1) | 242 (100) |
| Exposure (Hands vs. Eyes) | 112 (46.3) | 130 (53.7) | 242 (100) |
| C-arm Vertical 1 | 110 (45.5) | 132 (54.5) | 242 (100) |
| Distance | 104 (43.0) | 138 (57.0) | 242 (100) |
| Surgery | 102 (42.1) | 140 (57.9) | 242 (100) |
| Total | 1434 (59.2) | 986 (40.7) | 2420 (100) |
OR: operating room
A total of 120 (49.5%) were compliant with radiation protection protocols [Figure 4]. The most commonly used radiation protection tool was the lead apron (89.3%), while protective eye goggles were the least used (6.6%). The participants with overall good compliance scores who chose ≥50% of the time for the above four compliance indicators were 398 (41.1%) [Table 3].
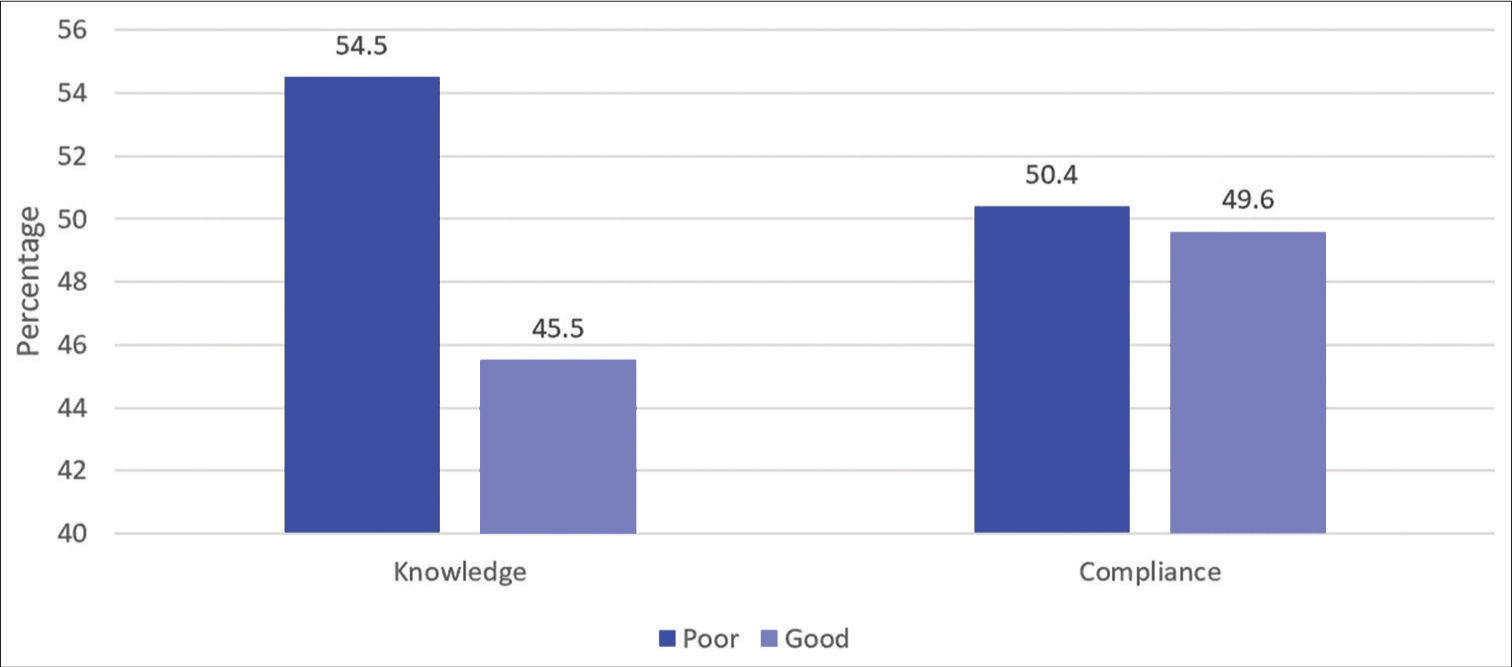
- Levels of knowledge and compliance.
| Protective device | ≥50% of the time (%) | <50% of the time (%) | Total (%) |
|---|---|---|---|
| Dosimetry | 84 (34.7) | 158 (65.3) | 242 (100) |
| Thyroid shield | 82 (33.9) | 160 (66.1) | 242 (100) |
| Lead apron | 216 (89.3) | 26 (10.7) | 242 (100) |
| Protective eye goggles | 16 (6.6) | 226 (93.4) | 242 (100) |
| Total | 398 (41.1) | 569 (58.9) | 967 (100) |
OR: operating room
When comparing the knowledge and compliance scores in relation to the socio-demographic characteristics of the respondents, females showed significantly better compliance scores than males (T= −1.775; P = 0.030). We also observed that those who believe that they need further training regarding radiation hazards (T = 2.379; P = 0.021), those who had more than 10 years in practice (T = −2.379; P = 0.006), and those who were fellow/specialist (F = 7.434; P = 0.005) demonstrated significantly better knowledge score than the other groups. Furthermore, radiology technicians demonstrated significantly better scores in both knowledge (F = 18.447; P < 0.001) and compliance (F = 24.744; P < 0.001). On the other hand, among consultants and fellows/specialists, general orthopedics (F = 2.419; P = 0.020) exemplified significantly lower compliance scores than their counterparts from the other orthopedic subspecialties [Table 4]. The correlation between the knowledge and compliance scores was positively statistically significant (r = 0.129; P = 0.046), indicating that while the score in knowledge increased, the score in compliance also increased [Figure 5].
| Factor | Knowledge | F/T test; | Compliance | F/T test; |
|---|---|---|---|---|
| Score (10) | P-value | Score (8) | P-value | |
| Mean±SD | Mean±SD | |||
| Gendera | ||||
| Male | 4.17±1.84 | T=1.311; | 5.58±0.89 | T=-1.775; |
| Female | 3.83±1.90 | 0.112 | 5.80±0.79 | 0.030‡ |
| Do you believe that you need further training regarding radiation hazards?a | ||||
| Yes | 4.16±1.86 | T=2.379; | 5.65±0.88 | T=0.558; |
| No | 3.18±1.68 | 0.021‡ | 5.55±0.80 | 0.789 |
| Years in practicea | ||||
| ≤10 years | 3.85±1.89 | T=−2.379; | 5.67±0.79 | T=0.501; |
| >10 years | 4.43±1.76 | 0.006‡ | 5.61±0.99 | 0.399 |
| Job positionb | ||||
| Physician|| | 3.71±1.81 | F=18.447; | 5.52 ± 0.83 | F=24.744; |
| OR nurse | 4.86±1.79 | <0.001‡ | 5.43 ± 0.74 | <0.001‡ |
| Radiology technician | 5.60±1.16 | 6.60 ± 0.62 | ||
| Physician’s† | ||||
| Resident | 3.15±1.68 | F=7.434; | 5.67±0.80 | F=2.392; |
| Fellow/Specialist | 4.32±1.75 | 0.005‡ | 5.48±0.81 | 0.088 |
| Consultant | 3.93±1.83 | 5.36±0.86 | ||
| Subspecialtyb* | ||||
| General orthopedics | 4.25±1.73 | F=2.154; | 4.92 ± 0.50 | F=2.419; |
| Trauma and reconstructive surgery | 4.60±1.79 | 0.078 | 5.50±1.05 | 0.020‡ |
| Pediatric orthopedics | 4.09±1.72 | 5.55±1.01 | ||
| Sports and/or arthroplasty | 3.64±2.01 | 5.64±0.66 | ||
| Spine surgery | 5.00±1.76 | 5.60±0.84 | ||
| Orthopedic oncology | 2.75±0.46 | 5.50±0.53 |

- Linear correlation (Pearson-r) between knowledge and compliance scores.
DISCUSSION
The results of this study reveal the inadequacy of knowledge about radiation exposure, as well as lack of compliance with radiation protection among the participants, which is consistent with other studies in different countries among orthopedic physicians.[15,16]
In Jentzsch et al., study, 65% of the sample has chosen the correct knowledge answers,[14] which significantly higher than that in our study (40.7%) [Table 2]. Their results also demonstrated that the participants were mostly compliant with lead apron.
In a study conducted by Tunçer et al., revealing that lead apron was the most commonly used protective equipment (88%), the study concluded that orthopedic surgeons have insufficient knowledge about the safe use and risks of fluoroscopy and how to prevent damage. However, their study did not include OR nurses nor radiology technicians.[17]
Many factors determine the radiation dose in orthopedic theaters, such as the duration and volume of intraoperative X-ray, the positioning of the surgeons, the patient, and the X-ray machine, as well as the experience of the surgeon and the type of surgery; hence, any preventive measure should target modifying the latter risk factors to reduce radiation exposure to all.[18,19]
There are many preventive measures against radiation exposure, training remains the most important one, around 90.9% of our sample believe that they need further training regarding radiation protection, in a study carried out by Gendelberg et al., orthopedic registrars who underwent a structured radiation safety training program were able to reduce radiation time and exposure for themselves and their patients.[20] In another study conducted by Bott et al., in which they described a training method that aimed to further educate surgeons in positioning C-arm with a computer-based training and simulation system, the results were remarkable as 79% stated that they had gained new knowledge.[21] Using protective equipment contribute to significantly lower radiation exposure, for example, a thyroid shield is found to decrease radiation exposure by 20-fold,[22] while a lead apron with a standard 0.5-mm thickness can attenuate around 90% of the scatter radiation. A 0.5- or 0.75-mm Lead glasses reduce more than 95% of scatter radiation to the eyes.[23] Eye protection is often taken for granted as our results suggest, recent evidence suggests that radiation-induced cataract might form acutely from one time radiation exposure without a defined threshold and at lower doses, the evidence also concluded that current lead glasses might offer sub-optimal protection against radiation.[24]
The importance of dosimetry to healthcare workers is to measure the amount of radiation dose received during the radiological procedure, to work properly dosimeters need to be accurate, precise, tissue equivalent, and energy independent.[25]
Protective equipment needs to cover the greatest exposure areas of the surgeon, such as the extremities and the head and neck.[26,27]
Other preventive measures include reducing X-ray duration, which can be achieved by short pedal taps. Moreover, positioning the surgeon on the image intensifier side reduces exposure to the scattered radiation [Figure 3], reducing the current, and increasing the voltage is correlated with a less contrasted image. However, it is also associated with less radiation, when feasible, this preventive measure should be employed.[14]
Standing at a distance of 0.5 m away from the patient helps in a four-fold reduction in radiation exposure. Hence, maintaining a proper distance when taking the image is crucial.[28] Collimation, which is defined as controlling the beam’s diameter to the needed region of the patient, hence, protecting the rest of the patient and OR staff from the scattered radiation, can be employed when a small area needs to be filmed and should be used when possible.[29]
The low compliance rates were evident in our study may be increased by constantly reminding surgeons and OR nurses to use radiation protection tools and by implementing policies that mandate using them. This motivated some countries to mandate radiation protection programs for physicians who are going to be exposed to radiation as part of their career despite the exposure dose.[30] Another method of increasing compliance is increasing knowledge about radiation protection and hazards, as participants who had higher knowledge levels were more compliant with radiation protection.
In our study, females showed significantly higher compliance rates than males, which might be attributed to fear of developing breast or thyroid cancer, both of which radiation is a major risk factor, especially among females.[31] In a study conducted by Chou et al., it was found that female orthopedic surgeons had a statistically significant 2.9-fold higher prevalence of breast cancer compared to the general U.S. female population, and a prevalence that was 85% higher than the general U.S. female population.[10]
Radiology technicians had significantly higher compliance rates and knowledge scores. This might be owed to the different background and pre-graduate training that radiology technicians receive.
As suggested in the literature, radiation exposure and screening times decreased with increasing level of experience, showing that less experienced surgeons receive higher radiation dose. Surgeons who are more experienced have better surgical skills, which reduces the number of intraoperative X-ray images, as well as the duration of radiation exposure.[32-35] In our results, experience was also significantly associated with better knowledge as participants having more than or equal to 10 years of experience had better scores. The lack of protective equipment might also play a role in the low compliance rates, as the majority of the sample stated that they did not find radiation protection tools available when they needed them. Hence, we encourage health institutions not only to make sure that there is an abundant supply of radiation protection equipment but also check the protective equipment’s regularly as many of as many of the aprons are old and do not protect because of bad storing leading to brakes in the shield. In the current study, surgeons showed less compliance with radiation protection compared to OR nurses and radiology technicians, Meisinger et al. concluded that possible causes of this difference include the inconvenient positioning of shields, heavyweight of aprons, tight and unhygienic thyroid collars, and stiff lead gloves, all of which hinder the surgeons’ movement and further complicate the surgery.[36]
In our results, it has been found that sports and/or arthroplasty surgeons are more compliant with using radiation protection tools. This might be attributed to the fact that intraoperative imaging is seldom used in their practice compared to other sub-specialties.
More generalizable results could have been achieved with the probability sampling technique. However, we chose non-probability sampling technique for easier access and quicker time to gather the data. The smaller number of OR nurses and radiology technicians compared to orthopedic staff is also a limitation of the present study. There were few local papers that measured the level of compliance with radiation protection to compare our results with, which imposed another limitation to the study.
CONCLUSION
Intraoperative radiation is necessary for the orthopedic OR, which imposes a risk to the orthopedic OR personnel, adequate knowledge about radiation and compliance with radiation protection is necessary to prevent radiation hazards, in our study, the participants showed a lack of both knowledge and compliance.
RECOMMENDATIONS
Based on our results, we recommend that healthcare institutions should implement and enforce policies to lower radiation exposure by enhancing compliance with radiation protection tools. Health-care institutions should pay more attention to conducting radiation protection training sessions that attend to specific orthopedic needs, such as the safe positioning of the C-arm as well as the proper use of their foot pedals. Furthermore, the supply of protective gears and checking them for effectiveness, we also recommend the change of the old X-ray machines to newer ones that reduce the duration of radiation exposure without compromising the quality of the image. ORs should be equipped with ceiling-mounted radiation shielding.
AUTHORS’ CONTRIBUTIONS
AHA conceived and designed the study, conducted literature research, provided research materials, and collected and analyzed data as well as initial and final manuscript preparation and editing. RSA and MAA have contributed to the design of the study, data collection and interpretation, manuscript preparation and editing. ISA and HMA have contributed to the design of the study as well as data analysis and data interpretation, and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
An Institutional Review Board (IRB) approval from King Khalid University Hospital IRB committee numbered (E-21-5865) was obtained for this study on 23 March 2021.
Declaration of participants consent
The authors certify that they have obtained all appropriate participants consent forms. In the form, the participants have given their consent to be reported in the journal.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
References
- Radiation: Are we and our patients protected enough? J Musculoskelet Surg Res. 2021;5:83-4.
- [CrossRef] [Google Scholar]
- Tracking cumulative radiation exposure in orthopaedic surgeons and residents: What dose are we getting? J Bone Joint Surg Am. 2017;99:1324-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ionising radiation exposure to orthopaedic trainees: The effect of sub-specialty training. Ann R Coll Surg Engl. 2006;88:297-301.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976). 2000;25:2637-45.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of radiation exposure from X-ray imaging among scoliotic patients at a tertiary care hospital. J Musculoskelet Surg Res. 2021;5:41-5.
- [CrossRef] [Google Scholar]
- Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: A systematic review. Eur J Med Res. 2012;17:28.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005;13:69-76.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence for a lack of DNA double-strand break repair in human cells exposed to very low x-ray doses. Proc Natl Acad Sci USA. 2003;100:5057-62.
- [CrossRef] [PubMed] [Google Scholar]
- Patient and Staff Radiological Protection in Cardiology. Compend Dose Coefficients based ICRP Publ No. 60. :130.
- [Google Scholar]
- Increased breast cancer prevalence among female orthopedic surgeons. J Womens Health (Larchmt). 2012;21:683-9.
- [CrossRef] [PubMed] [Google Scholar]
- Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond). 2005;55:498-500.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness and attitudes amongst basic surgical trainees regarding radiation in orthopaedic trauma surgery. Biomed Imaging Interv J. 2010;6:e25.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of knowledge and awareness regarding radiation safety and fluoroscopy use among orthopedic surgeons in Saudi Arabia. J Musculoskelet Surg Res. 2021;5:35-40.
- [CrossRef] [Google Scholar]
- The compliance with and knowledge about radiation protection in operating room personnel: A cross-sectional study with a questionnaire. Arch Orthop Trauma Surg. 2015;135:1233-40.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation safety knowledge and practices among Irish orthopaedic trainees. Ir J Med Sci. 2015;184:369-73.
- [CrossRef] [PubMed] [Google Scholar]
- Orthopaedic surgeons' use and knowledge of ionizing radiation during surgical treatment for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2016;24:3962-70.
- [CrossRef] [PubMed] [Google Scholar]
- Orthopedic surgeons' knowledge regarding risk of radiation exposition: A survey analysis. SICOT J. 2017;3:29.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring intraoperative radiation exposure of the trauma surgeon, Measuring eye, thyroid gland and hand with highly sensitive thermoluminescent detectors. Unfallchirurg. 1999;102:371-6.
- [CrossRef] [PubMed] [Google Scholar]
- X-ray in trauma and orthopedic surgery, Physical and biological impact, reasonable use, and radiation protection in the operating room. Oper Orthop Traumatol. 2011;23:70-8.
- [Google Scholar]
- A radiation safety training program results in reduced radiation exposure for orthopaedic residents using the mini C-arm. Clin Orthop Relat Res. 2016;474:580-4.
- [CrossRef] [PubMed] [Google Scholar]
- Improving education on C-arm operation and radiation protection with a computer-based training and simulation system. Int J Comput Assist Radiol Surg. 2009;4:399-407.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure during fluoroscopy: Should we be protecting our thyroids? Aust N Z J Surg. 1999;69:847-8.
- [CrossRef] [PubMed] [Google Scholar]
- Operator shielding: How and why. Tech Vasc Interv Radiol. 2010;13:167-71.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation-induced cataractogenesis: A critical literature review for the interventional radiologist. Cardiovasc Intervent Radiol. 2016;39:151-60.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic radiology dosimetry: Status and trends. Appl Radiat Isot. 2016;117:74-81.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. J Clin Diagn Res. 2015;9:RC01-4.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure to the orthopaedic surgical team during fluoroscopy: How far away is far enough? J Orthop Trauma. 1997;11:392-8.
- [CrossRef] [PubMed] [Google Scholar]
- Electronic collimation of radiographic images: Does it comprise an overexposure risk? Br J Radiol. 2018;91:20170958.
- [CrossRef] [PubMed] [Google Scholar]
- Exposure to solar ultraviolet radiation and breast cancer risk: A dose-response meta-analysis. Medicine (Baltimore). 2020;99:e23105.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure of the hands and thyroid gland during percutaneous wiring of wrist and hand procedures. Acta Orthop Belg. 2006;72:194-8.
- [Google Scholar]
- Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: A clinical study. Arch Orthop Trauma Surg. 2004;124:659-64.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation exposure to the hands of orthopaedic surgeons during procedures under fluoroscopic X-ray control. Br J Radiol. 1993;66:899-901.
- [CrossRef] [PubMed] [Google Scholar]
- Does surgical experience decrease radiation exposure in the operating room? J Pediatr Orthop. 2021;41:389-94.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation protection for the fluoroscopy operator and staff. AJR Am J Roentgenol. 2016;207:745-54.
- [CrossRef] [PubMed] [Google Scholar]






