Translate this page into:
The effect of a rehabilitation neck exercise program on biomechanical head alignment, neck pain, and disability among nursing students: A randomized controlled trial
*Corresponding author: Dalia M. A. Elsherbini, Department of Clinical Laboratory Sciences, College of Applied Medical Sciences, Jouf University, Sakaka, Saudi Arabia. dmelsherbini@ju.edu.sa
-
Received: ,
Accepted: ,
How to cite this article: Abd-Eltawab AE, Shormana MA, Elsherbini DM, ElRazkey JY. The effect of a rehabilitation neck exercise program on biomechanical head alignment, neck pain, and disability among nursing students: A randomized controlled trial. J Musculoskelet Surg Res. 2024;8:281-90. doi: 10.25259/JMSR_74_2024
Abstract
Objectives:
The objectives of this study were to investigate the effect of a rehabilitation neck exercise program (RNEP) on head alignment, neck pain, and disability among nursing students.
Methods:
The present study involved 360 university nursing students, with 180 in an experimental group and 180 in a control group. The experimental group received an RNEP consisting of isometric, stretching, and range of motion (ROM) exercises for four weeks, while the control group was instructed to maintain their present level of physical exercise. The measurements obtained from the visual analog scale (VAS) for pain, neck disability index (NDI), and ruler measurements for the ROM were taken before and after treatment for both groups.
Results:
The present work showed a significant difference in the outcome variables for the ruler measurement, NDI and VAS (P < 0.001). Our results showed a significant improvement in ruler measurement and NDI in the experimental group (57.8% and 88.3%, respectively, compared to the control group (0.0%)). On the other hand, those measurements were significantly worse in the control group (28.3% and 63.1%, respectively). The number of participants with no pain was significantly increased in the experimental group (22.8%). The participants with mild pain were increased in the experimental group (40%) compared to baseline (36.1%) while decreased in the control group (35.6%).
Conclusion:
The controlled rehabilitation neck exercises program reduced the neck pain, disability index, and improved the ROM of upper cervical flexion. The occupational field of nursing requires regular exercises for the neck and cervical muscles.
Keywords
Disability
Head alignment
Neck muscles
Nursing
Rehabilitation neck exercise program
INTRODUCTION
Forward head posture (FHP) is characterized by maintaining cervical vertebrae in extension, which causes tightness in posterior musculature and increases the risk of cervical disc prolapse. Normal ear, shoulder, and hip alignment are essential for FHP diagnosis. Misalignment in landmarks, such as the ear in front of the shoulders, is an indicator of FHP.[1]
According to the line of gravity pathway, it was reported to pass anterior to the Atlanta-occipital joints. Therefore, the counterbalanced posterior cervical moment is required to keep the balanced head.[2] Thus, inclined the head anterior reduces the power of the neck and respiratory muscles, respectively.[3] Excessive computer use without proper ergonomics can exaggerate cervical curve vertebrae, affecting neck muscles, and increasing the incidence of cervical disc prolapse.[4]
Thus, the forward head position is one of the postural abnormalities that expose the cervical region to disk prolapse. As reported by Lee et al.[5] and Peng et al.,[6] FHP affects the deep neck receptors that reflect inversely on the neck motion. Lee et al.[7] randomly assigned 28 19-year-old cases to McKenzie and self-stretch exercises, with a 53° craniovertebral angle, for eight weeks, with daily exercises lasting 25 min and performed three times a week. Their study found that all interventions increased the angle of the head, suggesting that the recommended exercises improved forward head and rounded shoulder posture, thereby reducing the risk of disk prolapse. Moreover, neck exercises are vital in controlling neck pain, consequently protecting the cervical region from injuries. Thus, Abdel-Aziem[8] studied the effect of McKenzie protocol exercises on subjects who suffer from chronic neck pain. This study involved 55 chronic neck pain participants divided into two groups: one introduced classic exercises and the other combined McKenzie scapulothoracic exercises. Results showed a decrease in neck pain intensity in both groups.
Mehri et al. revealed that there was a significant effect on the first group that introduced exercise compared with the other group.[9] Thirty-two women with nonspecific neck pain were divided into case and control groups. The first group received neck exercises for eight weeks. Meanwhile, the second group received active self-exercise and a home program.
Stretching exercises for the neck muscles have been proven by Amoudi and Ayed to improve neck pain and disabilities.[10] Their study introduced two groups: control and experimental groups. The experimental group was instructed to do systematic neck and shoulder stretching exercises. The control group was instructed to maintain their present level of physical exercise. The total duration was four weeks, and the treatment period was five days/week. Their results revealed that the experimental group showed a better reduction in neck pain and impairment compared to the control group. Wickstrom et al. also revealed that patients who received extension cervical exercises and traction over 17 weeks revealed a decrease in pain level.[11]
A previous study assessed the thickness of side-bending cervical muscles in asymptomatic women aged 20–40. Results showed higher muscle thickness in women with forward heads. The study aimed to reduce neck pain among nursing students by influencing the reaming region of the vertebral column. Morningstar determined the relationship between reducing forward head position and thoracic pain reduction.[12]
However, Mahmoud et al. found a negative correlation between FHP and neck pain severity, citing a systematic review of head position measures in individuals with and without neck discomfort, but the review’s conclusions were influenced by inconsistent findings.[13,14]
Limited research has studied the effect of work-related musculoskeletal head and neck disorders on nursing students in the future of their occupational field. Working long hours can lead to such health issues. Therefore, the present study aimed to evaluate the value of a controlled neck exercise program in reducing the intensity of nursing students’ pain and improving the percentage of neck disabilities index (NDI) by normalizing the angle of leaning head forward.
MATERIALS AND METHODS
Design and setting
This study was a randomized controlled trial registered in Pan African Clinical Trial Registry No (PACTR202305496961094). The Standards Consolidated Trial Reporting were followed in the current work [Figure 1].[15] It was conducted in the Faculty of Nursing, Alexandria University, from January to March 2023.
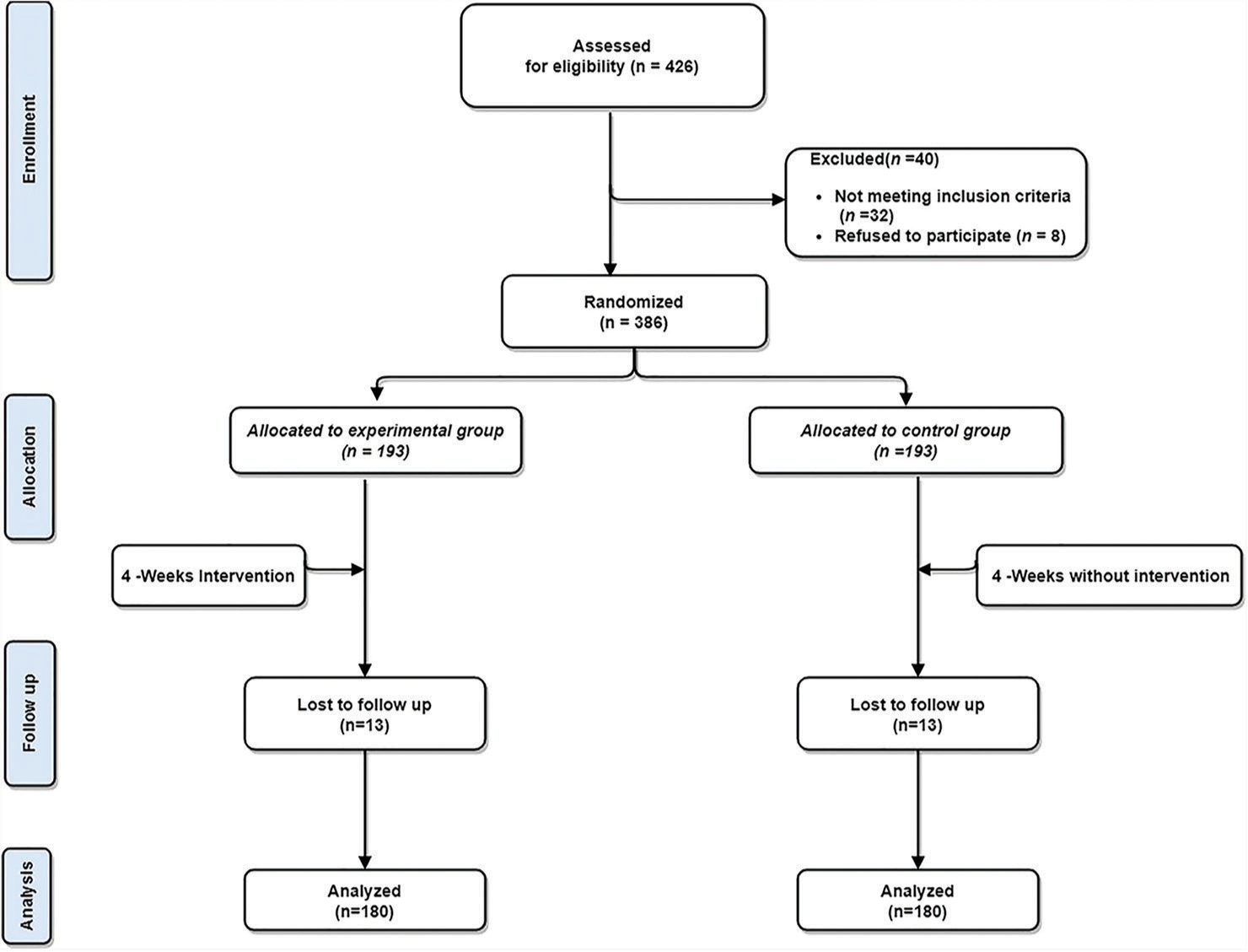
- Consolidated standards of reporting trials (CONSORT) flowchart of the study.
Sample size calculation
Epi info software (Version 3.01 Sullivan 2003–2008)[16] was applied to determine the sample size. The information available from the rehabilitation neck exercise program (RNEP) and control group were used to detect the size affected (d) and then, through equal allocation, divide by the four levels, from each 90. The minimum sample size was determined according to the final sample size, which was 360. The software adjusted the following percentages for the final sample size calculation: the confidence level at 95, the confidence limit at five, and the expected frequency at 50.
Participants
University nursing students participated in the present study. All participants met the following inclusion criteria: they were 19–21 years old and had a body mass index ranging from 20 to 24 kg/m2. The primary complaint was chronic neck pain without referred pain to the arm or hands. The NDI scored above 15 out of 50. Besides, the visual analog score using a visual analog scale (VAS) was six out of ten. Students with FHP were also included in this study. Participants with previous trauma or surgery in the head, cervical regions, and upper extremities were excluded from the present study. Proper history-taking and clinical assessment for all participants were done to rule out any systemic disease that could interfere with the interventions.
Randomization
University students (426) were assessed for eligibility; 32 were excluded from the trial because they did not meet the inclusion criteria, and eight refused participation. As a result, 386 students were included in the current trial. They were randomly divided into two equal-sized groups; each group included 193 students. There was a nonresponse of 13 students’ dropouts as they did not attend the follow-ups due to sick leave from students or personal circumstances.
The study used computer-induced randomization to stratify cases into groups, with assignments concealed using closed, black envelopes. The same physical therapist administered the interventions for both groups, with only researchers and trainers aware of the randomized assignments. Assessors were kept in the dark about the randomization and not involved in the exercise interventions. Evaluations were conducted before and after the intervention for four weeks. An RNEP in the form of isometric, stretching, and range of motion (ROM) exercises was introduced for the experimental group, in addition to maintaining their physical activities (n = 180), with 54 male and 126 female cases. However, the control group was instructed to maintain their present level of physical exercise (n = 180), 57 male and 123 female cases.[10]
Measurements taken with a ruler were used to determine the FHP of each participant, focusing on the horizontal distance from a wall to the right tragus. The left tragus was measured using the same method. Participants were instructed to stand with their chin tucked in, shoulders back, knees extended, and heels and buttocks against the wall. This method, known as the tragus measurement tool or tragus-to-wall (TWD) measurement, was used to measure the distance between the back of their head and a wall using a ruler while standing with their back to the wall.[17] The TWD test was validated by Bohannon et al. It is an easy-to-use, objective measure of forward-flexed posture, as it indicates that the greater the distance from the wall, the greater the degree of FHP.[17]
The NDI was adopted to assess disability related to neck pain. It includes four items related to subjective symptoms and six items related to activities of daily living.[18] The NDI includes six probable responses for functional activities in each sector (from 0 to 5). If it varied from zero to 50, a higher score indicated greater disability. The degree of disability was obtained by percentage. The minimum varied percentage from zero up to 20, moderate varied from 21 up to 40, and severe documented from 41 until 60. The consistency and validity of the NDI had been approved.[19] The English version of the NDI was translated into Arabic (NDI-Ar) and back-translated using established procedures. Sixty-five patients with neck discomfort performed the NDI-Ar twice over one week to measure test-retest reliability. Internal consistency, construct validity (factor structure), and responsiveness were all assessed as part of additional psychometric testing. The Arabic version of the NDI has a 2-factor, 10-item format and is a dependable, valid, and responsive tool for evaluating neck pain in Arabic-speaking patients. As a result, it can be suggested for clinical and scientific applications. In addition, the VAS was adopted to measure pain. It is a numerical scale from 0 up to 10. Participants were asked to circle the respective numbers according to his/her pain level. The VAS is a subjective measurement tool. However, it has been studied and proven to be a reliable and valid measure of chronic pain intensity.[20]
Intervention
RNEP
Exercises were done in ten repetitions for 10 s hold, three sessions per week, for up to four successive weeks.[10] It was demonstrated as follows:
Stretching neck flexors muscle
The participant sat on a chair and relaxed by stretching the neck flexors muscle sternocleidomastoid muscle bilaterally (10 repetitions), then unilateral (5 repetitions) hold from 6–10 s. The participant did neck extension (pressed the chin while straightening the neck). The therapist stood behind the participant, stabilizing the front head with the other hand on the anterior chest and then applying a stretch. On the unilaterally affected side, the participant bent the neck against it and rotated it to the same side of the shortened muscles. The therapist stood behind the participant, stabilizing his head with one hand around the side of the participant’s head to position their head against the therapist’s trunk. Then, place the other hand against the top of the thoracic cage, asking them to inhale and exhale while applying stretching.[21]
Manual strengthening neck extensors
Participants were instructed to sit on a chair, relax, and apply manual strength. They were asked to sit with a full head flexion, with one hand on the occiput and the other on the shoulder for stabilization. They were, then, asked to move their head up and receive submaximal resistance.[22]
Active self-stretching
Participants were instructed to stand beside a table holding its underside. The head was in extension, with the opposite side bending with rotation toward the same side of the muscle being stretched away from the affected side. To stabilize the scapula, the participant had to reach down with the hand on the affected side, holding onto the chair’s seat.
Active self-strengthening
The participant was instructed to press the back of the head into both hands to strengthen the posterior muscular structure group of the neck. Besides, the participant was instructed to actively elevate both shoulders with rotation and side-bending to both sides[22] [Supplementary Figure S1].
Statistical analysis
The study applied a paired t-test using GraphPad Prism version 9 to analyze data, comparing outcomes within two groups. Two-way repeated measures analysis of variance (ANOVA) was used to determine differences in input variables. A generalized estimating equations correction was used by a linear regression model, and the variation in the ruler measurement, NDI, and visual analog scale over time for each group compared with the baseline was determined and assessed. The homogeneity and normality of variance were evaluated before using the parametric assumption. Eliminated extremes were filtered. Significance was considered when P = 0.05.
RESULTS
Demographic data were collected for the participants [Table 1]. The sample included 360 cases (180 for the tested and 180 for the control groups). The difference was not significant for sex (P = 0.73).
| Sex | Experimental group (n=180) | Control group (n=180) | χ2 | P-value | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Male | 54 | 30.0 | 57 | 31.7 | 0.117 | 0.73 |
| Female | 126 | 70.0 | 123 | 68.3 | ||
χ2: Chi-square test
Data for clinical measures before and after the RNEP are presented in Table 2 and Figure 2. Ruler measurement, NDI, and VAS showed a significant increase in the control group but a significant decrease in the experimental group after four weeks of intervention compared to the baseline (P < 0.001). There was also a significant improvement in clinical measures in the experimental group compared to the control group after four weeks of intervention (P < 0.001).
| Variable | Experimental group | Control group | Group X time interaction P-value | p-valueb between groups | Effect size (η2) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | After 4 weeks | MD (95%CI) | p-valuea within group | Baseline | After 4 weeks | MD (95%CI) | p-valuea within group | ||||
| Ruler measurement | 10.83±0.10 | 10.15±0.11 | −0.68 (−0.78−0.58) | <0.001 | 10.61±0.15 | 11.13±0.14 | 0.52 (0.38–066) | <0.001 | <0.001 | <0.001 | 0.08 |
| NDI | 23.31±1.09 | 19.49±0.90 | −4.88 (−5.37−4.28) | <0.001 | 22.98±0.97 | 26.01±0.92 | 3.03 (2.19–3.86) | <0.001 | <0.001 | <0.001 | 0.06 |
| VAS | 4.65±0.17 | 2.86±0.16 | −1.79 (−1.97−1.60) | <0.001 | 4.37±0.17 | 4.64±0.17 | 0.27 (0.15–0.38) | <0.001 | <0.001 | <0.001 | 0.11 |
Values are shown as mean±standard error of the mean. NDI: Neck disability index, VAS: Visual analog scale, MD: Mean difference, CI: Confidence interval. P-valuea: Value within the group from paired-samples t-test. P-valueb: Value between control and experimental group after four weeks from Independent-Samples t-test. η2: Partial eta square between control and experimental group after four weeks. Group X time interaction P-value from two-way repeated measures analysis of variance (ANOVA).
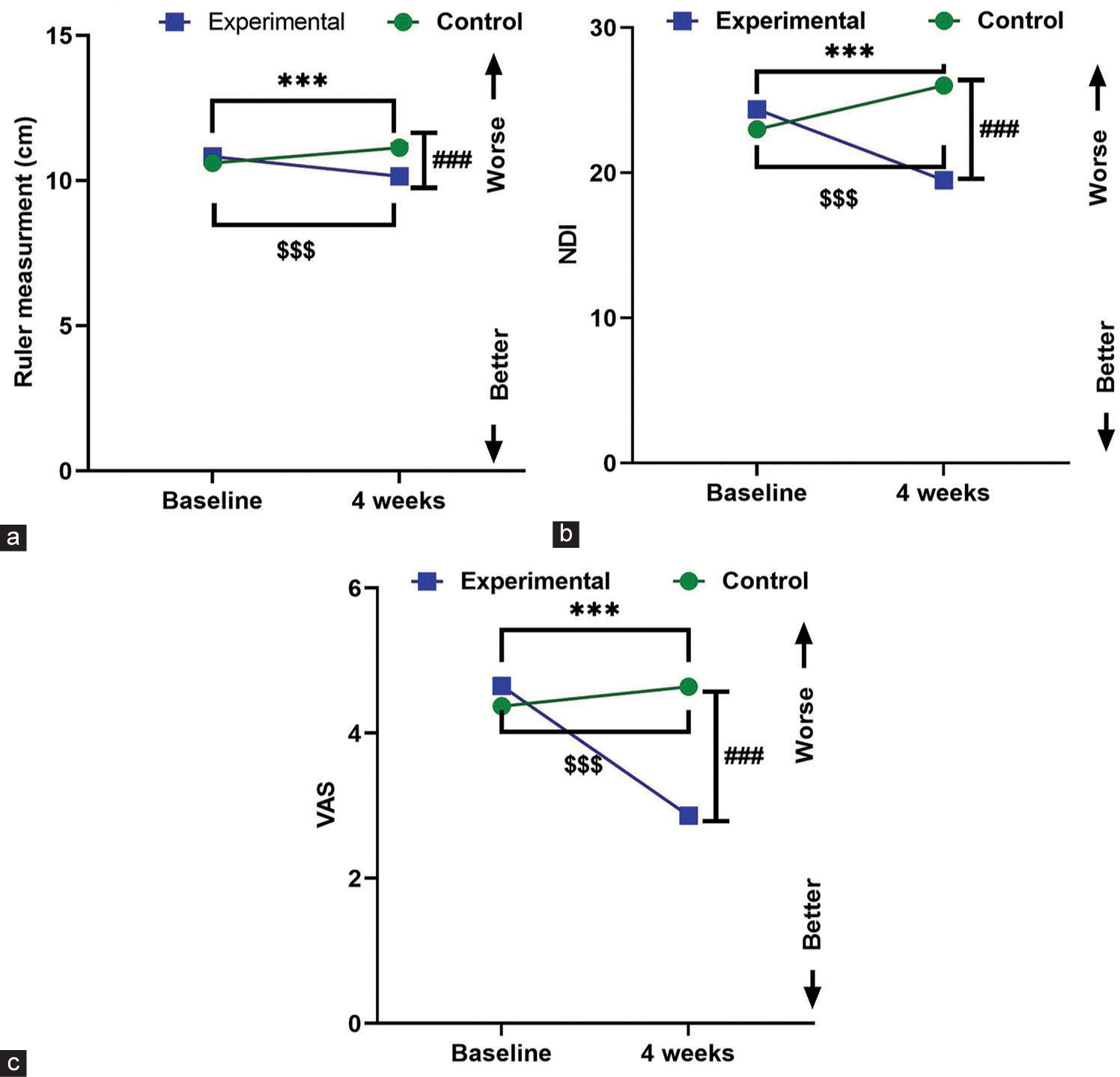
- a) Change in ruler measurement over time in each group. b) Change in NDI over time in each group. c) Change in VAS over time in each group. Data are expressed as mean ± Standard error of the mean (SEM). ***p < 0.001 within experimental group at baseline vs.after four weeks, $$$p < 0.001 within control group at baseline vs. after four weeks. ###p < 0.001 of experimental vs. control group after four weeks. NDI: Neck Disability Index; VAS: Visual analogue scale.
Two-way repeated measures ANOVA showed a significant change for the ruler outcome variable, F (1, 358) = 23.40, P < 0.001, η2 = 0.08. It also showed significant change for the NDI and VAS outcome variables, (F [1, 358] = 15.54, P < 0.001, η2 = 0.06 and F (1, 358) = 39.20, P < 0.001, η2 = 0.11), respectively.
Significant improvement in ruler measurement and NDI in the experimental group (57.8% and 88.3%, respectively) compared to the control group (0.0%) is shown in Table 3. On the other hand, those measurements were significantly worse in the control group (28.3% and 63.1%, respectively) compared to the experimental group.
| Outcome | Ruler measurement | NDI | ||||
|---|---|---|---|---|---|---|
| Experimental group (n=180) | Control group (n=180) | χ2 (P-value) | Experimental group (n=180) | Control group (n=180) | χ2(P-value) | |
| n(%) | n(%) | |||||
| Improved | 104 (57.8) | 0 (0.0) | 168.70 (<0.001)* | 159 (88.3) | 0 (0.0) | 288.97 (<0.001)* |
| No change | 76 (42.2) | 129 (71.7) | 21 (11.7) | 115 (63.9) | ||
| Worse | 0 (0.0) | 51 (28.3) | 0 (0.0) | 65 (36.1) | ||
χ2: Chi-square test. *P≤0.05-Stastically significant Chi-square. NDI: Neck disability index
The number of participants with no pain [Table 4] was significantly increased in the experimental group (22.8%). The number of participants with mild pain increased in the experimental group (40%) compared to baseline (36.1%), while it decreased in the control group (35.6%). The percentage of participants with severe pain significantly declined in the experimental group after four weeks, 6.1% compared to the baseline 18.9%, and remained unchanged in the control group. Participants with the worst pain presented 0.0% in the experimental group after four weeks compared to baseline (3.9%) and remained unchanged in the control group. This was reflected in the percentage of improvement in the experimental group, reaching 92.8%, while the percentage of unchanged or worse results was apparent in the control group.
| Visual analog scale | Baseline | After 4 weeks | ||||||
|---|---|---|---|---|---|---|---|---|
| Experimental group (n=180) | Control group (n=180) | Experimental group (n=180) | Control group (n=180) | |||||
| No. | % | No. | % | No. | % | No. | % | |
| No pain (0) | 3 | 1.7 | 0 | 0.0 | 41 | 22.8 | 0 | 0.0 |
| Mild (1–3) | 65 | 36.1 | 76 | 42.2 | 72 | 40.0 | 64 | 35.6 |
| Moderate/severe (4–6) | 71 | 39.4 | 58 | 32.2 | 56 | 31.1 | 70 | 38.9 |
| Very severe (7–9) | 34 | 18.9 | 42 | 23.3 | 11 | 6.1 | 42 | 23.3 |
| Worst pain possible (10) | 7 | 3.9 | 4 | 2.2 | 0 | 0.0 | 4 | 2.2 |
| χ2(P-value) | 6.83 (0.145) | 65.16 (<0.001*) | ||||||
| Experimental group (n=180) | Control group (n=180) | |||||||
| No. | % | No. | % | |||||
| Improved | 167 | 92.8 | 0 | 0.0 | ||||
| No change | 6 | 3.3 | 156 | 86.7 | ||||
| Worse | 7 | 3.9 | 24 | 13.3 | ||||
| χ2(P-value) | 315.21 (<0.001*) | |||||||
χ2: Chi-square test. *: Statistically significant at P≤0.05
Comparison of males and females according to ruler measurement, NDI, and VAS improvements is shown in Table 5.. Regarding ruler measurement improvement, it was revealed that the percentage of improvement was significantly higher in females than in males in the experimental group (P < 0.05).
| Experimental group (n=180) | Control group (n=180) | |||||||
|---|---|---|---|---|---|---|---|---|
| Males (n=54) | Females (n=126) | Males (n=57) | Females (n=123) | |||||
| No. | % | No. | % | No. | % | No. | % | |
| Ruler measurement | ||||||||
| Improved | 25 | 46.3 | 79 | 62.7 | 0 | 0.0 | 0 | 0.0 |
| No change | 29 | 53.7 | 47 | 37.3 | 33 | 57.9 | 96 | 78.0 |
| Worse | 0 | 0.0 | 0 | 0.0 | 24 | 42.1 | 27 | 22.0 |
| χ2(P-value) | 4.169 (0.041*) | 7.79 (0.005*) | ||||||
| OR (CI 95%) | 1 | 1.95 (1.02–3.80) | ||||||
| Fisher’s exact test (P-value) | 0.05* | |||||||
| Neck disabilities index | ||||||||
| Improved | 44 | 81.5 | 115 | 91.3 | 0 | 0.0 | 0 | 0.0 |
| No change | 10 | 18.5 | 11 | 8.7 | 50 | 87.7 | 65 | 52.8 |
| Worse | 0 | 0.0 | 0 | 0.0 | 7 | 12.3 | 58 | 47.2 |
| χ2(P-value) | 3.514 (0.061) | 20.532 (<0.001*) | ||||||
| OR (CI 95%) | 1 | 2.38 (0.91–5.94) | ||||||
| Fisher’s exact test (P-value) | 0.08 | |||||||
| Visual analog scale | ||||||||
| Improved | 48 | 88.9 | 119 | 94.4 | 0 | 0.0 | 0 | 0.0 |
| No change | 3 | 5.6 | 3 | 2.4 | 57 | 100.0 | 99 | 80.5 |
| Worse | 3 | 5.6 | 4 | 3.2 | 0 | 0.0 | 24 | 19.5 |
| χ2(P-value) | 1.820 (0.403) | 12.833 (<0.001*) | ||||||
| OR (CI 95%) | 1 | 2.13 (0.65–6.08) | ||||||
| Fisher’s exact test (P-value) | 0.21 | |||||||
χ2: Chi-square test, OR: Odds ratio, CI: Confidence interval. *: Statistically significant at P≤0.05
On the other hand, the percentage of cases getting worse was significantly higher in males than in females in the control group (P < 0.01). A link was established between the likelihood of improvement and the gender in the experimental group (odds ratio [OR]: 1.95, 95% confidence interval [CI] [1.02– 3.80]; P = 0.05). In the context of NDI improvement, it was revealed that the percentage of improvement was higher in females than in males in the experimental group, which was insignificant (P = 0.061). On the other hand, the percentage of cases getting worse was significantly higher in females than in males in the control group (P < 0.001). An insignificant link was established between the likelihood of improvement and the gender in the experimental group (OR: 2.38, 95% CI [0.91–5.94]; P = 0.08). Analyzing VAS improvement, it was revealed that the percentage of improvement was higher in females than in males in the experimental group, which was insignificant (P = 0.403). On the other hand, the percentage of cases getting worse was significantly higher in females than in males in the control group (P < 0.001). An insignificant link was established between the likelihood of improvement and the gender in the experimental group (OR: 2.13, 95% CI [0.65–6.08]; P = 0.21).
DISCUSSION
Reduced daily physical activity can lead to improper posture, particularly FHP, due to abnormalities in the line of gravity. An RNEP can help enhance FHP, particularly among younger students who benefit from the advised program.[23]
The present study found a significant difference in output variables for ruler measurement, NDI, and VAS (P < 0.001). The experimental group showed a significant improvement in these variables compared to the control group and a decrease in the same variable for the control group, which was observed after four weeks of intervention compared to the baseline.
The current results support Amoudi and Ayed.[10] Their study evaluated the effectiveness of exercise stretching for nurses’ neck pain, with the first group receiving a recommended program and the second group did not, based on the improvement in pain and disability levels for the first group. Besides, Karimian et al.[24] conducted a study on the impact of eight-week neck exercises on nurses. The study involved 216 nurses, with 29 participating in the neck exercises for eight weeks, revealing a decrease in musculoskeletal neck disorders.
Kang et al.[25] conducted a study on nursing students’ work habits and prolonged computer use. They compared cervical angle and head protrusion between those working for over 6 h and those who rarely used computers. The study found that prolonged computer use exposed the head to a lean forward posture and disrupted balance. The study involved 30 volunteers per group.
In accordance with the results obtained by Haughie et al.,[26] they found a correlation between head posture, cervical bending backward, and neck pain. Office workers and nursing students experienced similar pain during prolonged computer use. They used a cervical ROM device to study the relationship between FHP and extended cervical bending position. The study found a correlation between pain intensity, neck posture, FHP, and head backward position. Moreover, Shin et al.[27] found that increasing shoulder ROM significantly increased neck pain measurement in young females with FHP, indicating a negative correlation. The VAS, with its numerous response categories, is more sensitive to changes in pain intensity than measures with limited responses. However, it may not produce reliable ratings across different patient groups due to individual interpretations of the scale.[28] Another limitation of the VAS is that it is complex and requires translating sensory experiences into linear formats, which some patients find abstract or difficult to understand, with reported noncompliance rates ranging from 7% to 26%.[29]
Moreover, Gasibat et al.[30] proved that stretching exercises can reduce pain, disabilities, and increase muscle flexibility and endurance in individuals with musculoskeletal disorders. This aligns with our findings, as they improve cervical ROM, quality of life, and decrease cervical disc prolapse in nursing students. Examining neck exercises’ effects on high school students’ necks also yielded results similar to those obtained by the present study on nursing faculty students. Lee et al.[31] found that strengthening exercises for anterior cervical spine muscles are crucial for maintaining head stability and head and back posture in high school students. Thus, the strengthening program for the neck muscle proved that their results were in accordance with the results obtained by De Vitta et al.[32] They showed that the increased ROM and improved performance of NDI for the cervical muscles might be attributed to the reduction of pain. The same was obtained by Im et al.,[33] comparing two groups: one with scapular rehabilitation for 35 minutes and the other with relaxation exercises. The results showed that the first group had a positive effect on improved quality of life compared to the second group. Kisner and Colby[34] proved that exercise plays a crucial role in improving bone concentration and general health, preventing osteoporosis, and enhancing joint ROM. The study’s main limitation is its inability to assess the impact of RNEP on participants’ physical and mental quality of life, including psychological state and functional variance. The study was brief and only included those with FHP, and it did not determine the long-term benefits of RNEP for FHP students. A longitudinal study is recommended.
CONCLUSION
Regular neck muscle rehabilitation programs have shown clinical benefits for nursing students, improving NDI performance and head alignment, and reducing neck pain. These programs, along with variables like ruler measurement, VAS, and NDI, help students protect their cervical and neck muscles from overuse-related work injuries, preparing them for future nursing careers.
Recommendations
Given these findings, we recommend comparing various categories of neck pain diseases and fitness levels among nursing students to meet occupational requirements. Following the trial, we encourage the control group to practice RNEP to benefit from the program. Students dealing with patients in intensive care or emergency units should receive special instructions to maintain head alignment and avoid increasing the degree of FHP, which increases the liability for disc prolapse. Future nursing student training should take into account future results.
AUTHORS’ CONTRIBUTIONS
AEA, MAAS, and JYE were involved in the conception and design. MASS and JYE conducted the experimental studies. DMAE and JYE were involved in data acquisition, AEA, MAAS, and DMAE analyzed data, AEA wrote the initial and final draft of the article, and DMAE edited and reviewed the article’s final draft. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Faculty of Nursing Research Ethics Committee, Alexandria University, Alexandria, authorized the study on July 17, 2022 (Serial Number: 2022-9-39).
DECLARATION OF PARTICIPANTS CONSENT
The authors certify that they have obtained all appropriate participants’ consent forms for this study. In the forms, the participants consented to their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that no artificial intelligence (AI)-assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
Supplementary DOI
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Flexion dysfunction of atlanto-occipital joint associated with cervical spondylosis. Orthop Surg. 2021;13:267-75.
- [CrossRef] [Google Scholar]
- The impact of chronic neck pain on respiratory functions among female university students. J Health Sci Med Res. 2021;40:349-57.
- [CrossRef] [Google Scholar]
- Effect of rehablitation on muscle imbalance in upper cross syndrome. Int J Recent Trends Sci Technol. 2016;6:57-63.
- [Google Scholar]
- Correlation between trunk posture and neck reposition sense among subjects with forward head neck postures. Biomed Res Int. 2015;2015:689610.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical proprioception impairment in neck pain-pathophysiology, clinical evaluation, and management: A narrative review. Pain Ther. 2021;10:143-64.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in rounded shoulder posture and forward head posture according to exercise methods. J Phys Ther Sci. 2017;29:1824-7.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of deep neck flexor exercise for neck pain: A randomized controlled study. Türk Fiziks Rehabil Derg. 2016;62:107-15.
- [CrossRef] [Google Scholar]
- Effects of corrective exercises on posture, pain, and muscle activation of patients with chronic neck pain exposed to anterior-posterior perturbation. J Manipulative Physiol Ther. 2020;43:311-24.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of stretching exercise program among nurses with neck pain: Palestinian perspective. Sci Prog. 2021;104:368504211038163.
- [CrossRef] [PubMed] [Google Scholar]
- Non-surgical relief of cervical radiculopathy through reduction of forward head posture and restoration of cervical lordosis: A case report. J Phys Ther Sci. 2017;29:1472-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical curve restoration and forward head posture reduction for the treatment of mechanical thoracic pain using the pettibon corrective and rehabilitative procedures. J Chiropr Med. 2002;1:113-5.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between forward head posture and neck pain: A systematic review and meta-analysis. Curr Rev Musculoskelet Med. 2019;12:562-77.
- [CrossRef] [PubMed] [Google Scholar]
- Studies comparing surrogate measures for head posture in individuals with and without neck pain. Phys Ther Rev. 2010;15:12-22.
- [CrossRef] [Google Scholar]
- CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012;10:28-55.
- [CrossRef] [PubMed] [Google Scholar]
- Tragus-to-wall: A systematic review of procedures, measurements obtained, and clinimetric properties. J Back Musculoskelet Rehabil. 2019;32:179-89.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement properties of the neck disability index: A systematic review. J Orthop Sports Phys Ther. 2009;39:400-17.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-cultural adaptation, reliability, and validity of the arabic version of neck disability index in patients with neck pain. Spine (Phila Pa 1976). 2013;38:E609-15.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e088.
- [CrossRef] [PubMed] [Google Scholar]
- Stretching exercises vs manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. J Rehabil Med. 2007;39:126-32.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of effectiveness of isometric exercises with and without stretching exercises in non specific cervical pain. Int J Physiother. 2016;3:371-5.
- [CrossRef] [Google Scholar]
- Postural patterns of daily life of male high school students by positional distortion. Unpublished master's thesis. Cheongwon-Gun: Korea National University of Education;
- [Google Scholar]
- The effect of corrective exercises on musculoskeletal disorders. HSR. 2010;6:520-8.
- [Google Scholar]
- The effect of the forward head posture on postural balance in long time computer based worker. Ann Rehabil Med. 2012;36:98-104.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of forward head posture and cervical backward bending to neck pain. J Man Manip Ther. 1995;3:91-7.
- [CrossRef] [Google Scholar]
- Correlations among visual analogue scale, neck disability index, shoulder joint range of motion, and muscle strength in young women with forward head posture. J Exerc Rehabil. 2017;13:413-7.
- [CrossRef] [PubMed] [Google Scholar]
- A descriptive study of the use of visual analogue scales and verbal rating scales for the assessment of postoperative pain in orthopedic patients. J Pain Symptom Manage. 1999;18:438-46.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of selected pain assessment tools for use with the elderly. Appl Nurs Res. 1993;6:39-46.
- [CrossRef] [PubMed] [Google Scholar]
- Stretching exercises to prevent work-related musculoskeletal disorders-a review article. Am J Sports Sci. 2017;5:27-37.
- [CrossRef] [Google Scholar]
- Effects of neck exercise on high-school students' neck-shoulder posture. J Phys Ther Sci. 2013;25:571-4.
- [CrossRef] [PubMed] [Google Scholar]
- Neck pain and factors associated in university students: A cross sectional study. Ciênc Mov. 2020;22:89-101.
- [CrossRef] [Google Scholar]
- Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J Phys Ther Sci. 2015;28:951-5.
- [CrossRef] [PubMed] [Google Scholar]
- Range of motion In: Therapeutic exercise foundations and techniques. United States: F.A. Davis; 2012. p. :61-73.
- [Google Scholar]







