Translate this page into:
The impact of COVID-19 pandemic on orthopedic resident training programs: A systematic review
2 College of Nursing, King Saud University, Riyadh, KSA
Corresponding Author:
Raed Alahmadi
Security Forces Hospital Program, Riyadh
KSA
dr.raedalahmadi@gmail.com
| How to cite this article: Alahmadi R, Alotaibi A, Alzahrani E. The impact of COVID-19 pandemic on orthopedic resident training programs: A systematic review. J Musculoskelet Surg Res 2021;5:96-102 |
Abstract
COVID-19 has severely affected health-care services and training throughout the world. This systematic review aimed to evaluate the impact of COVID-19 on orthopedic resident education and training programs globally. A comprehensive literature search was performed on PubMed and Google Scholar, including articles published until September 2020. Studies on orthopedic residents, published in English, including in-rotation or out-rotation orthopedic residents were included, whereas studies with non-orthopedic residents or trainees or non-resident program affiliations were excluded. Of the 178 articles fetched for this systematic review, 7 were included in the present systematic review and analyzed according to the PRISMA guidelines. The use of online learning varied from 86.0% to 34.9%. The impacts on orthopedic residents included impaired surgical and/or clinical training, concerns about annual training goals, anticipated need for an additional year for training, cancelation of teaching and study leaves, problems in completing a dissertation, increased difficulty in recruiting new patients for research, and mental health-related concerns. COVID-19 infection has significantly affected the education and training programs of orthopedic residents. Web-based learning should be updated according to the requirements of residents. Developing and incorporating technologies in the training programs, such as distance learning, virtual meeting platforms, virtual and augmented reality, and simulation-based learning, should be encouraged. Conducting virtual conferences, meetings, and courses should be promoted. Reducing stress and anxiety in the residents with mock tests before virtual examinations and improving interpersonal communication should be of prime importance; examinations should be conducted on time with the necessary precautions in order not to prolong the residency tenure.
Introduction
In March 2020, COVID-19 was declared a pandemic by the World Health Organization. Since then, as of April 2021, over 120 million cases have been reported worldwide.[1] Countries throughout the world have raised the highest level of crisis alerts and adopted diverse measures to actively and quickly deal with the infection and minimize its impact. These approaches involve reducing the transmission rate by following social distancing measures and increasing the inpatient preparedness and capacity in hospitals. Nevertheless, this rapidly evolving emergency situation has overwhelmed the health-care system, which is facing several challenges, such as insufficient manpower and resources, as well as placing risk of infection on frontline health-care staff. All medical specialties have been affected in different ways. In most countries, elective surgeries have been limited, and only essential procedures are being considered. Moreover, surgeons and residents have been deployed on rotations to fields other than their expertise. Health-care education has received a major change in these times, and students face difficulties in receiving education, as well as training due to limited clinical and surgical exposure, primarily due to decreased inpatient and outpatient activities.[2]
The orthopedic practice has also been severely affected by the current situation. On a regular day before the pandemic, the orthopedic resident training typically involves patient visits, surgeries, research, and seminars. However, in the present situation, orthopedic case volume has massively dropped, and nonurgent surgeries and consultations are being postponed or canceled to minimize virus spread. Furthermore, national and international orthopedic training, conferences, and workshops have been postponed, canceled, or the format has been changed to online. In response to the present situation, most of the teaching centers and hospitals worldwide have adopted the web-based teaching and learning model to continue the education and training of orthopedic residents.[3] There has been a paradigm shift from problem-based learning to virtual learning.[4] While the advantages of e-learning are well established, like providing easy access to information and helping share information for a broad array of relevant information, its effectiveness and acceptability for orthopedic education and training in the present scenario is unclear. Furthermore, since this education model has abruptly arrived, its impact on orthopedic residency programs is yet to be fully evaluated. This issue has been highlighted in several health-care fields; however, its effect on worldwide orthopedic education and training is unclear. Therefore, this systematic review aimed to assess the impact of COVID-19 pandemic on orthopedic resident education and training programs in different regions. The results of this systematic review would help identify the strength and weaknesses of orthopedic education and training programs and help improvise this form of training for future orthopedic surgeries.
Materials and Methods
Search strategy and selection criteria
A targeted literature search was performed on PubMed and Google Scholar, including articles published till September 2020. The following keywords were used for literature search: “Coronavirus,” “COVID,” “SARS-CoV-2,” “Severe acute respiratory syndrome coronavirus 2,” “2019nCov,” “HCoV-19,” “orthoped*,” “musculoskeletal,” “educat*,” “train*,” “curriculum,” “impact,” and “effect.” The references of relevant articles were manually searched for additional studies. The inclusion criteria were orthopedic residents, who graduated from a medical college and enrolled to a residency training program in orthopedic surgery, articles published in English, hospital or home setting, and orthopedic residents in-rotation (in an orthopedic specialty rotation) or out-rotation (orthopedic residents in nonorthopedic specialty program rotation, e.g., intensive care unit (ICU), plastic surgery, neurosurgery, and general surgery). The exclusion criteria were interns (or 1st-year postgraduates in the USA), nonorthopedic residents or trainees, board holders (finished residency), nonresident program affiliations (e.g., volunteers, in-service, and temps), consultants, registrars, and senior officers. Moreover, since the primary objective was measuring the impact of COVID-19 on the training of orthopedic residents, articles such as letters to the editor, perspectives, and reviews were excluded.
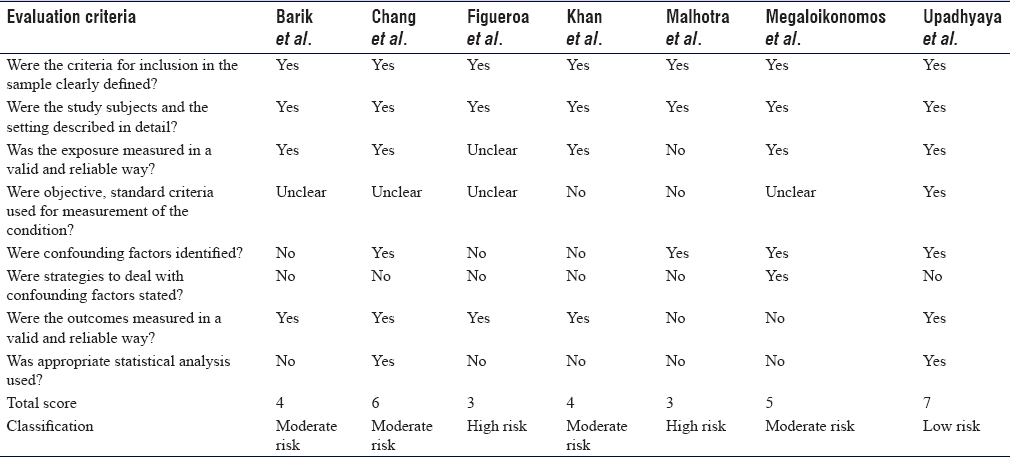
Risk of bias in individual studies
All the included studies were assessed for quality and risk of bias using the Joanna Briggs Institute Critical Appraisal Checklist for analytical cross-sectional studies.[5] The checklist uses eight components to evaluate the studies. Each component was rated as “yes,” “no,” “unclear,” or “not applicable” by two researchers independently. All discordant ratings were resolved by discussion within the study team. The risk of bias is classified as high (1–3 yes), moderate (4–6 yes), or low (7–8 yes).
Data extraction
Data comprising author information, publication year, country of the population studied, sample size, sample characteristics, assessment tools, and scores were evaluated.
Results
Study selection
Overall, 163 studies were initially fetched using electronic databases, and additionally, 15 studies were identified after manual search. After duplicate removal, the titles and abstracts of 126 studies were screened for eligibility, of which 94 studies were excluded. The full text of 32 articles was screened for the inclusion and exclusion criteria. Finally, 7 studies were included in the systematic review. [Figure - 1] demonstrates the PRISMA flowchart for the study selection.
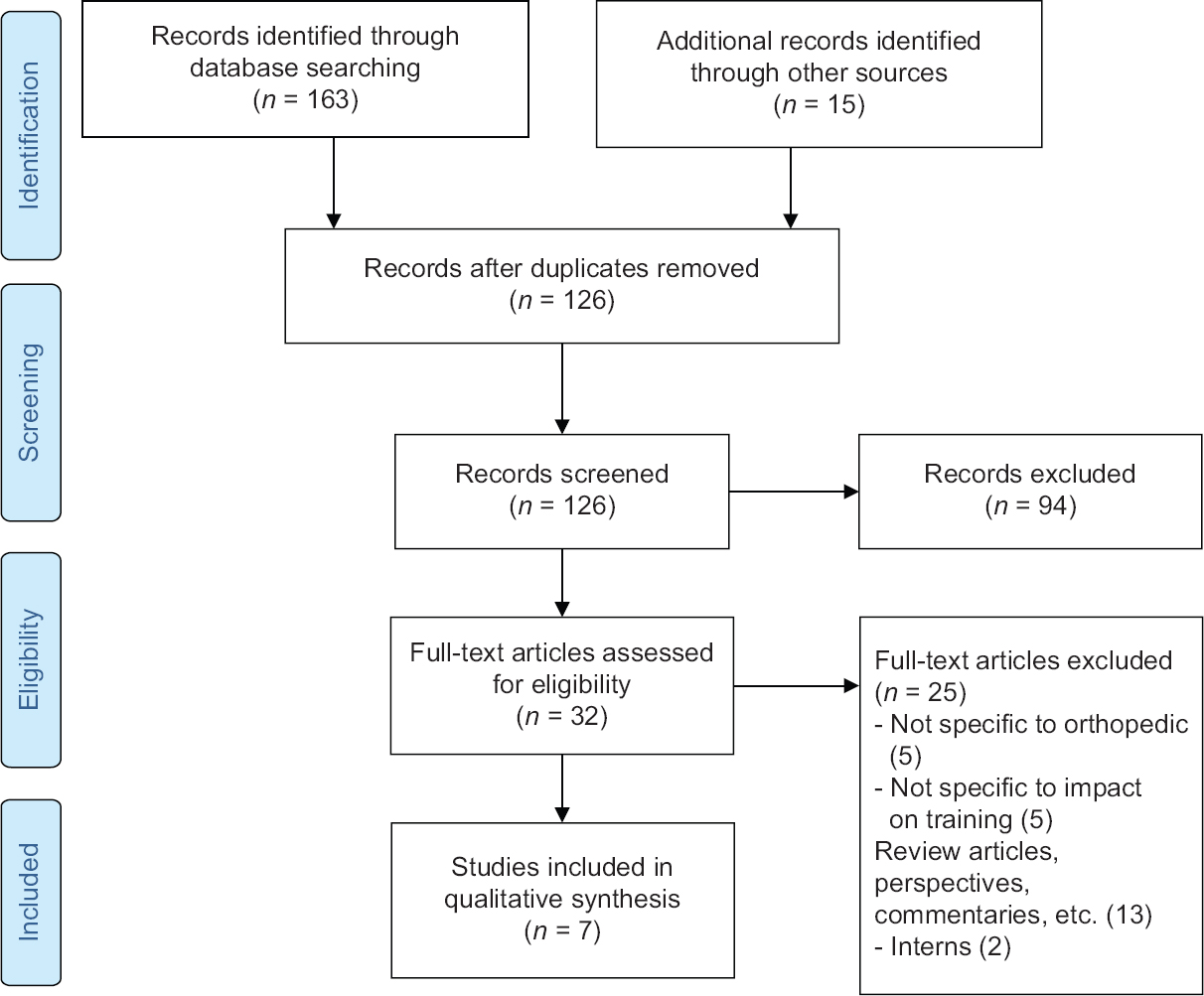 |
| Figure 1: PRISMA flowchart for the study |
Study characteristics
[Table - 1] presents the main findings of the 7 articles included in the present systematic review. Three studies included orthopedic residents from India, and one study was each from South Korea, Chile, UK, and Europe. The studies incorporated a broad range of teaching and evaluation strategies.[6],[7],[8],[9],[10],[11],[12] Data from surgeons and residents were collected as surveys and questionnaires. Furthermore, the examination strategies were assessed in two studies. Three studies reported following online-based learning, including webinars, online presentations, and/or tests. However, one study following the virtual examination pattern reported high satisfaction scores in both examiner and examinee groups. Moreover, one study also reported mental health-related concerns in the orthopedic residents.

[Table - 2] depicts the summary assessment of the risk of bias across the included studies. The risk of bias was high, moderate, and low for 2, 4, and 1 studt, respectively.
Operative impact
The impacts on orthopedic residents included impaired surgical and/or clinical training, concerns about annual training goals, anticipated need for an additional year for training, cancelation of teaching and study leaves, problems in completing dissertation, no clinical case discussions being held presently, and increased difficulty in recruiting new patients for research. The majority of participants (84.5%) in one study reported a substantial decrease in their basic skillsets for common orthopedic procedures, such as skin and skeletal traction application, local and intra-articular injections, cast application, and wound dressing. This was reflected in a feeling of lack of competency in the residents. In one study, 5.4% of respondents suggested continued surgical practices in the orthopedic department, and 57.1% reported the occurrence of only emergency procedures.[11]
Nonoperative impact
Only a small fraction of the respondents (24.5%) could complete their dissertations, which was attributable to no hospital visits, changes in work schedule, redeployment to other places, as well as decreased surgeries, OPD cases, and new patients. One study reported concerns in annual target achievements in 58.2% of participants. Of these, achieving the desired practical skills and completing the logbook were major concerns, followed by the final examination's uncertainty. Most of the postgraduate students in 1 (71.5%) study were redeployed to nonorthopedic departments, with COVID-19 patients as well as noninfected patients.[12] Another study reported that 7.0% and 18.0% of young arthroplasty surgeons were redeployed to ICU and non-ICU/emergency units, respectively.[13]
Impact on education
Overall, 86.0% to 34.9% of residents confirmed that their programs were using online education, including webinars, online presentations, and/or tests. While web-based learning was found to be easier by 44.2% of participants in one study,[6] another one reported low satisfaction levels with the same.[7] One study reported webinars and online presentations to be satisfactory, whereas online tests and patient evaluations were reported unsatisfactory.
Assessment of the impact of COVID-19 on teaching showed that, during the pandemic, complete disruption of clinical teaching was reported by most of the respondents (65.8%), whereas 2–3 times a week and once a week classes were reported by 9.4% and 23.9% of respondents, respectively. Another study reported a lack of clinical teaching (96.0%) and case presentations (91.0%), thus having a significantly negative impact on course completion. One study reported the impact on surgical education with reduced preoperative planning (49.2%), operation execution (58.6%), and postoperative care sessions (46.7%). Furthermore, bedside clinical education was impaired (56.0%), but remote clinical learning improved (55.3%). Examination strategies were assessed in two studies. One study suggested that following the virtual examination pattern had high satisfaction scores in both examiner and examinee groups. The other study reported that interface-based viva voce was difficult for 45.8% of residents, whereas multiple-choice questions or objective-structured clinical and practical examination (OSCE and ODSE) were well accepted.
Impact on mental health and well-being
The impact of COVID-19 on the mental health of the residents was also evaluated. One study reported 96.0% of orthopedic residents to be stressed in COVID-19 pandemic times. The major contributors to the stress and anxiety included surgical training period loss, fear of COVID-19 infection, staying away from family, possible infection spread to coworkers, and less confidence in surgical skills.[12]
Discussion
The present systematic review evaluated the challenges faced by orthopedic residents due to COVID-19 pandemic. These challenges were evident as redeployment of orthopedic residents to different departments that contributed to disrupted training due to decreased clinical and surgical practice, as well as and incorporation of web-based learning and examination strategies.
Challenges with orthopedic training
Redeployment of orthopedic residents addressed urgent health-care support requirement; however, it disrupted the education plans. Disrupted training was a major finding in all studies, primarily resulting from a dramatic fall in the surgical volume and surgery nature. Since clinical and surgical practice is a vital part of the orthopedic training curriculum, its disruption had profound effects, especially in the development of surgical skills.
The profound impact of the pandemic on trauma and orthopedic training has been linked with decreased operative exposure, cancelation of courses and examinations, and modifications in annual appraisals and specialty recruitments.[14] Other medical fields have also reported similar effects, and 84.5% of respondents in a study reported disruption of gastroenterology training due to the COVID-19 situation, which resulted in a major training gap and a substantial decrease in specialty training activities.[15] Studies in the neurosurgery and urology field have also reported a significant decrease in the exposure of residents to patients.[16],[17] The assessment of insights of residents showed fear of not reaching the desired goals in many respondents. This was primarily attributable to inadequate practical and surgical skills. The perspective of the training period not being utilized and the suspension of final assessment examinations was also reported in some respondents. This led to the development of a popular belief that the resident might require an additional year to complete the training. Several previous studies have also reported this fear. Culp et al.[13] reported the feeling of inadequate training in several arthroplasty surgeons, with a lack of confidence to establish a career. Another study by Ramos et al.[18] reported an almost 3-month loss of elective surgery experience in fellows receiving spine surgery training. The increased off-service time with the residents did not directly reflect in increased research activity during the pandemic since the results were mixed, with 36.1% of respondents of one study postulating a decrease in research and 27.1% suggesting an increase.[11] Nearly half of the participants in one study reported increased difficulty recruiting patients for research and conducting prospective research. Conversely, other studies have reported an increase in the research activity during times.[17] A study on orthopedic surgeons in Saudi Arabia has reported good knowledge, attitude, and practice toward COVID-19 pandemic.[19]
Training and education of orthopedic residents should follow a strategic approach involving improved coordination between the trainer and trainee to manage the workload and improvise the virtual training. Following telemedicine program is highly recommended for health-care centers for judicious use of resources and minimal virus exposure. The effectiveness of the 5-day telemedicine program was evaluated by Loeb et al.,[20] who focused on patient triage, technological requirements, credentialing, educating the health-care staff and patients, scheduling appointments, and regulatory requirements. Following a methodological approach by focusing on the key factors was suggested to achieve approximately 50.0% of the typical clinical volume in 2 weeks. Virtual training is likely to play a bigger role in the future; training programs should incorporate unique and novel methods to improvise e-learning. The American Association of Hip and Knee Surgeons (AAHKS) has put forth the Fellows Online COVID-19 AAHKS Learning initiative has suggested a collaborative approach to amplify the virtual lectures to make them available for all in the USA. However, its desired results require further cultivation and improved implementation of this approach.[3] Videos of virtual surgical practices could be performed using an interactive screen to improve participation and understanding of the residents. Developing and incorporating technologies in the training program, such as distance learning, virtual meeting platforms, virtual and augmented reality, and simulation-based learning, should be encouraged.[21] A study by Hedman and Tsai[22] has suggested a wide applications of virtual and simulated surgical training in helping the residents achieve better competence. This can help in maintaining the acquired skills and prevent skill decay. Psychomotor training coupled with 3D visualization can help the residents practice simulated surgical tasks. Therefore, attempts to improve the surgical skills outside the operating room should be the focus. Conducting virtual conferences, meetings, and courses should be encouraged.
Challenges with online learning
The education method was majorly changed, and a decline in teaching time, as well as traditional teaching methods, was reported in all the studies, and web-based virtual training was incorporated at all the centers. While the incorporation of webinars and online presentations was successfully adopted, high levels of dissatisfaction were reported for patient evaluations. Nevertheless, the residents also reported issues with work overload and scheduling due to the handling multiple activities such as webinars, lectures, and presentations.
In a survey of urological program, 48.0% of respondents reported a negative effect of COVID-19 on urological training-related didactics and that video conferencing was widely incorporated and was to be continued in the postpandemic educational program as well.[23] The literature regarding conducting end of training examinations for orthopedic residents was limited. In some countries, the final examination pattern is followed to evaluate the training of residents. One study comprehensively assessed different virtual examination styles and found most of them to be satisfactory for both examiners and examinees, except orthopedic physical examination and patient communication.[10] Trainers have also faced several challenges, especially in preparing the training materials. Due to unexpected circumstances, the quality of education has suffered, especially since most of the training material relies on freely accessible videos and images on the internet. This could limit the choice of education material for the trainer; therefore, the residents may already be familiar with the online material.[10]
These findings are important for several reasons. First, web-based learning cannot completely substitute the core surgical training imparted in operation theatres. Second, it provides a promising opportunity to implement web-based learning with advanced technologies for training the residents. Third, it makes teaching accessible globally without travel, so residents could attend teaching activities outside their region or even country, as this became the new norm. Examinations should be conducted on time with the necessary precautions, so that the residency tenure is not prolonged, or at least shorten the prolongation period if it was deemed extremely necessary.
Challenges with mental health
Uncertainty regarding the pandemic period was shown to affect the mental well-being of orthopedic residents, and the majority of the respondents had concerns regarding loss of surgical training and the risk of infection during work. In a systematic review, Hope et al. reported increased stress in 54.9% to 91.6% of trainees.[24] Mild-to-severe anxiety in medical students during COVID-19 pandemic was also reported in other studies, which reduced after online learning.[25]
Therefore, institutions should be aware of potential mental health-related challenges in orthopedic residents and include counseling sessions to improve mental health and well-being. Furthermore, reducing stress and anxiety in the residents with mock tests before virtual examinations and improving interpersonal communication should be of prime importance.
Nevertheless, the introduction of online education was beneficial to residents in some studies helping them learn new skills that they would not learn otherwise, such as dealing with a major pandemic, working under extreme stress, and planning for these. These dire circumstances also resulted in a major change in the online activity that would not have been done otherwise. In these unprecedented times, the mentor–student relationship has changed, with more support from mentors to increase residents' confidence in treating patients. Collaborations between health-care professionals and policymakers are required to resume clinical activities and surgeries, depending on the region. Redeployment of orthopedic residents to unfamiliar specialties could be seen as a time to adapt to surroundings, as they change.[26],[27]
The present systematic review had a few limitations. First, literature regarding the impact of COVID-19 on orthopedic training was scarce; therefore, only limited studies could be included. Furthermore, since the studies were from different countries, variations were observed in severity levels, which were reflected in the differences in strategies adopted by the different health-care centers. Furthermore, since most of the surveys included in this systematic review included multiple-choice questions, some nuances could be missed. Furthermore, the response rate in some studies was very low, thus affecting the generalizability of the results.
Conclusion
COVID-19 infection significantly affected the training and education programs for orthopedic residents. Negative impacts were not only limited to surgical and clinical experience but also to online education and mental health. Many residents were deployed to nonorthopedic units. In addition, a reduction in surgical volume disrupted the training, causing anxiety. Web-based learning was successfully adopted in most of the centers; however, work overload due to webinars and presentations was seen.
Recommendation
The following recommendations and solutions could be included to address the challenges faced by orthopedic residents. Web-based learning should be updated and customized for improved integration with the curriculum according to the requirements of residents. Developing and incorporating technologies in the training programs, such as distance learning, virtual meeting platforms, virtual and augmented reality, and simulation-based learning, should be encouraged. Conducting virtual conferences, meetings, and courses should be promoted; However, in the near future, national and international scientific societies will hold fewer conferences and more practical courses. With online sessions, groups from different cities or even countries could get teaching at the same time without the cost of travel. Telemedicine and virtual training sessions should be followed to improve the clinical and surgical skills of the residents. Reducing stress and anxiety in the residents with mock tests before virtual examinations and improving interpersonal communication should be of prime importance; examinations should be conducted on time with the necessary precautions in order not to prolong the residency tenure.
Ethics approval
The authors confirm that this review has been prepared in accordance with the COPE roles and regulations. Given the nature of the review, the IRB review was not required.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Author contributions
RMA has contributed to the conception, design, articles collection, data acquisition and statistical analysis, manuscript preparation, editing, and review of this article. EAA has performed literature search and statistical analysis. AFA supervised the research, review, and editing of the manuscript. All authors read and approved the final version of the manuscript.
| 1. | Coronavirus Disease (COVID-19) – World Health Organization. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Google Scholar] |
| 2. | Mavrogenis AF, Quaile A, Scarlat MM. The virus crisis affects orthopaedic surgery and scientific activities worldwide. Int Orthop 2020;44:813-7. [Google Scholar] |
| 3. | Stambough JB, Curtin BM, Gililland JM, Guild GN 3rd, Kain MS, Karas V, et al. The past, present, and future of orthopedic education: Lessons learned from the COVID-19 pandemic. J Arthroplasty 2020;35:S60-4. [Google Scholar] |
| 4. | Kogan M, Klein SE, Hannon CP, Nolte MT. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg 2020;28:e456-64. [Google Scholar] |
| 5. | The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Analytical Cross Sectional Studies. Available from: https://jbi.global/critical-appraisal-tools. [Google Scholar] |
| 6. | Barik S, Paul S, Kandwal P. Insight into the changing patterns in clinical and academic activities of the orthopedic residents during COVID-19 pandemic: A cross-sectional survey. Knee Surg Sports Traumatol Arthrosc 2020;28:3087-93. [Google Scholar] |
| 7. | Chang DG, Park JB, Baek GH, Kim HJ, Bosco A, Hey HW, et al. The impact of COVID-19 pandemic on orthopaedic resident education: A nationwide survey study in South Korea. Int Orthop 2020;44:2203-10. [Google Scholar] |
| 8. | Figueroa F, Figueroa D, Calvo-Mena R, Narvaez F, Medina N, Prieto J. Orthopedic surgery residents' perception of online education in their programs during the COVID-19 pandemic: Should it be maintained after the crisis? Acta Orthop 2020;91:543-6. [Google Scholar] |
| 9. | Khan H, Williamson M, Trompeter A. The impact of the COVID-19 pandemic on orthopaedic services and training in the UK. Eur J Orthop Surg Traumatol 2021;31:105-9. [Google Scholar] |
| 10. | Malhotra R, Gautam D, George J, Goyal D, Ansari MT. Conducting orthopaedic practical examination during the Covid-19 pandemic. J Clin Orthop Trauma 2020;11:S448-55. [Google Scholar] |
| 11. | Megaloikonomos PD, Thaler M, Igoumenou VG, Bonanzinga T, Ostojic M, Couto AF, et al. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery training in Europe. Int Orthop 2020;44:1611-9. [Google Scholar] |
| 12. | Upadhyaya GK, Jain VK, Iyengar KP, Patralekh MK, Vaish A. Impact of COVID-19 on post-graduate orthopaedic training in Delhi-NCR. J Clin Orthop Trauma 2020;11:S687-95. [Google Scholar] |
| 13. | Culp BM, Frisch NB. COVID-19 impact on young arthroplasty surgeons. J Arthroplasty 2020;35:S42-4. [Google Scholar] |
| 14. | Dattani R, Morgan C, Li L, Bennett-Brown K, Wharton RM. The impact of COVID-19 on the future of orthopaedic training in the UK. Acta Orthop 2020;91:627-32. [Google Scholar] |
| 15. | Marasco G, Nardone OM, Maida M, Boskoski I, Pastorelli L, Scaldaferri F, et al. Impact of COVID-19 outbreak on clinical practice and training of young gastroenterologists: A European survey. Dig Liver Dis 2020;52:1396-402. [Google Scholar] |
| 16. | Bambakidis NC, Tomei KL. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg 2020;133:1-2. [Google Scholar] |
| 17. | Rosen GH, Murray KS, Greene KL, Pruthi RS, Richstone L, Mirza M. Effect of COVID-19 on urology residency training: A nationwide survey of program directors by the society of academic urologists. J Urol 2020;204:1039-45. [Google Scholar] |
| 18. | Ramos O, Mierke A, Eastin M, Morrison MJ, Wongworawat DM, Danisa O. COVID-19 pandemic and the implications for orthopaedic and neurosurgery residents and fellows on spine rotations. North Am Spine Soc J 2020;1:100006. [Google Scholar] |
| 19. | AlMarshad AY, Binsultan GM, Alshayban MA, Alhusseini N, Alrifai O, Alhussainan TS, et al. Orthopedic surgeons' knowledge, attitude, and practice in view of COVID-19 in Saudi Arabia: A cross-sectional study. J Musculoskelet Surg Res 2021;5:51. [Google Scholar] |
| 20. | Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg 2020;28:e469-76. [Google Scholar] |
| 21. | Plancher KD, Shanmugam JP, Petterson SC. The changing face of orthopaedic education: Searching for the new reality after COVID-19. Arthrosc Sports Med Rehabil 2020;2:e295-8. [Google Scholar] |
| 22. | Hedman LR, Felländer-Tsai L. Simulation-based skills training in non-performing orthopedic surgeons: Skills acquisition, motivation, and flow during the COVID-19 pandemic. Acta Orthop 2020;91:520-2. [Google Scholar] |
| 23. | Pennington Z, Lubelski D, Khalafallah AM, Ehresman J, Sciubba DM, Witham TF, et al. Letter to the editor “changes to neurosurgery resident education since onset of the COVID-19 pandemic”. World Neurosurg 2020;139:734-40. [Google Scholar] |
| 24. | Hope C, Reilly JJ, Griffiths G, Lund J, Humes D. The impact of COVID-19 on surgical training: A systematic review. Tech Coloproctol 2021;25:1-6. [Google Scholar] |
| 25. | Saddik B, Hussein A, Sharif-Askari FS, Kheder W, Temsah MH, Koutaich RA, et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the united Arab Emirates. Risk Manag Healthc Policy 2020;13:2395-406. [Google Scholar] |
| 26. | Al-Mohrej OA, Aldakhil SS. Letter to editor: Editorial: Postcards from war zones-personal experiences during the COVID-19 pandemic. Clin Orthop Relat Res 2020;478:1953. [Google Scholar] |
| 27. | Almarshad A, Alghamdi A. Orthopedic trainees' perspective on coronavirus disease 2019. J Musculoskelet Surg Res 2020;4:166. [Google Scholar] |
Fulltext Views
1,875
PDF downloads
377





