Translate this page into:
The impact of obesity on pediatric orthopedic polytrauma patients
*Corresponding author: Talal Ibrahim, DOC Medical Center, Doha, Qatar. dr.talal@docmedc.com
-
Received: ,
Accepted: ,
How to cite this article: Dabboussi A, Abunimer AM, Elmhiregh A, Abdulrahman H, Ibrahim T. The impact of obesity on pediatric orthopedic polytrauma patients. J Musculoskelet Surg Res. 2025;9:64-9. doi: 10.25259/JMSR_324_2024
Abstract
Objectives:
The effect of obesity on fracture care and management in the adult population has been well documented in the literature; there is a scarcity of evidence-based research reporting the impact of obesity on pediatric orthopedic polytrauma patients. The aim of this study was to objectively investigate the impact of obesity on pediatric orthopedic polytrauma patients to optimize care and fracture management.
Methods:
A single-center retrospective cohort study of pediatric polytrauma patients aged 2–18 years old admitted to a level 1 trauma center was conducted over three years. Patients were categorized based on their body mass index (BMI). A logistic regression model was used to identify significant variables between the study groups.
Results:
A total of 60 patients were included in the analysis and divided into normal weight group (n = 36) and overweight/obese group (n = 24). A trend of lower injury severity score (ISS) was observed in the overweight/obese group compared to the normal weight group. Non-orthopedic injuries, including head, chest, and abdominal injuries, were found to be less in the overweight/obese group. Higher rates of spine and extremity fractures were reported in the overweight/obese group, as well as the need for surgical fixation (P = 0.05). No specific differences in complications, outcome, or discharge facility were found between the two groups.
Conclusion:
The paradoxical association between BMI and ISS/non-orthopedic injuries, in contrast to spine and extremity fractures, reflects the complex relationship between obesity and polytrauma patterns. Large multi-center prospective studies are needed to predict clinical outcomes in pediatric orthopedic polytrauma patients.
Keywords
Fracture
Obesity
Orthopedic
Pediatric
Polytrauma
INTRODUCTION
The trends of obesity and its related clinical sequelae have been steadily rising during the past decades, affecting about 40 million children under five years of age and more than 330 million children and adolescents aged between 5 and 19 years worldwide.[1] Although the effects of obesity on fracture care and management in the adult population have been well documented in the literature,[2-4] there is a scarcity of similar data reporting the impact of obesity on pediatric orthopedic polytrauma patients.[1,2] Despite the higher bone mineral density and additional soft-tissue padding, there are higher rates of extremity injuries reported in obese children compared to non-obese children.[5-7]
Multiple studies have reported significant adverse outcomes regarding the associations between obesity and length of stay (LOS), discharge disposition, complications, and other variables.[8-10] Weiss et al.[11] retrospectively studied the outcomes of treating pediatric patients with femoral shaft fractures using flexible intramedullary nails. This study reported higher complication rates in obese patients >50 kg compared to non-obese patients (46.2% and 17.2%, respectively, P = 0.03). The authors reported increased infection rates, re-fractures requiring revision surgery, ulcers from a fracture brace, heel ulcers, peroneal nerve palsy, and nonunion. These results were fundamental in changing the paradigm of treating femoral shaft fractures using flexible intramedullary nails in young children whose weight exceeds 50 kg.
As several physiological challenges are imparted by childhood obesity, there is significant morbidity and mortality encountered in the management of pediatric obese polytraumatized patients.[12] This study aimed to objectively assess the impact of obesity on pediatric orthopedic polytrauma patients to optimize care and fracture management.
MATERIALS AND METHODS
We conducted a single-center retrospective cohort study over three years, which our Institutional Review Board approved. Study participants included pediatric polytrauma patients aged 2–18 years old who were admitted to our level 1 trauma center. We included all orthopedic polytrauma pediatric patients as defined by sustaining at least one orthopedic injury (e.g., fracture, dislocation, or ligamentous injury) and one of the following or combination of injuries: Head, chest, and abdominal injury. The exclusion criteria were pediatric polytrauma patients without orthopedic injuries, underweight patients, and patients without recorded body mass index (BMI) information. Underweight patients have been excluded as the primary focus of this paper is on obesity, thus, the control group has been categorized as those with normal or healthy weight.
As recommended by the American Academy of Pediatrics and the Centers for Disease Control and Prevention (CDC), the BMI was categorized according to age and gender using the CDC growth charts, which were interpreted as follows: <5th percentile was labeled underweight, 5th–85th percentile was considered normal or healthy weight, 85th–95th percentile as overweight, and above 95th percentile as obese children.[13]
A total of 76 charts were reviewed. Data variables collected included demographics (age, sex, BMI), injury severity score (ISS), medical comorbidities, mechanism of injury, orthopedic and non-orthopedic injuries (head, chest, and abdomen), intensive care unit (ICU) LOS and ventilation days, LOS at the hospital, need for orthopedic surgical intervention, outcomes in terms of alive or deceased, complications, and discharge disposition.
Statistical analysis
Analysis was done after excluding the underweight category (n = 9), as well as patients with missing data or under the age of two years old (n = 7). The overweight/obese group (n = 24) included merged categories of both overweight (n = 12) and obese patients (n = 12) to have a similar comparative group. These BMI groups were correlated with the data variables. In addition, ISS was first sub-grouped into two groups: ≤15 and >15, as any reading >15 signifies a serious trauma/polytrauma.[14] Then, both groups were correlated with all other variables.
All data were coded and analyzed using the Statistical Package for the Social Sciences (IBM, New York, USA). Descriptive statistics were employed, including mean, median, range, and standard deviation. Frequencies (%) and their corresponding 95% confidence intervals (CI) were calculated. The Student t-test and Mann–Whitney U-test were used to compare numerical data, while the Chi-square test and Fisher’s exact test were applied to categorical data. Logistic regression analyses were conducted to determine the significance between groups, with a significance level set at ≤0.05.
RESULTS
The analysis included a total of 60 patients [Table 1]. Of the study sample, 52 (86.7%) patients were male. Most of the patients did not have any comorbidities. However, three patients had asthma (2/3 of them were overweight/obese patients). Although most of the correlations did not show statistically significant results, a trend of lower ISS scores was observed in the overweight/obese group (18.4 ± 9.1) compared to the normal weight group (23.6 ± 11.2). Similar findings were encountered when BMI was correlated with ISS [Figure 1]. All other system injuries, including head, chest and/or abdominal injuries, were found to be less in the overweight/obese group. Patients belonging to the overweight/obese group experienced fewer abdominal injuries compared to the normal weight group (25% and 41.7%, respectively; P = 0.19).
| Variable | Normal weight group (5th –<85th percentile) (n=36) |
Overweight/obese group (>85th percentile) (n=24) | P-value |
|---|---|---|---|
| Age (years), mean (±SD) | 12.4±4.6 | 12.9±4.1 | 0.67 |
| Sex, (%) | |||
| Males | 30 (83.3) | 22 (91.7) | 0.35 |
| Females | 6 (16.7) | 2 (8.3) | |
| Injury severity score, mean (±SD) | 23.6±11.2 | 18.4±9.1 | 0.06 |
| Non-orthopedic injuries, (%) | |||
| Head | 24 (66.7) | 14 (58.3) | 0.19 |
| Chest | 21 (58.3) | 13 (54.2) | |
| Abdomen | 15 (41.7) | 6 (25.0) | |
| Mechanism of injury, (%) | |||
| MVC | 21 (58.3) | 17 (70.8) | 0.40 |
| Fall from height | 7 (19.4) | 3 (12.5) | |
| ATV | 4 (11.1) | 0 (0.0) | |
| Pedestrian hit by car | 2 (5.6) | 2 (8.3) | |
| Motorcycle accident | 2 (5.6) | 1 (4.2) | |
| Self-inflicted | 0 (0.0) | 1 (4.2) | |
| ED disposition on admission, (%) | |||
| ICU | 17 (47.2) | 9 (37.5) | 0.69 |
| Ward | 14 (38.9) | 11 (45.8) | |
| OR | 4 (11.1) | 4 (16.7) | |
| Deceased | 1 (2.8) | 0 (0.0) |
MVC: Motor vehicle collision, ATV: All-terrain vehicle, ED: Emergency department, ICU: Intensive care unit, OR: Operating room, SD: Standard deviation
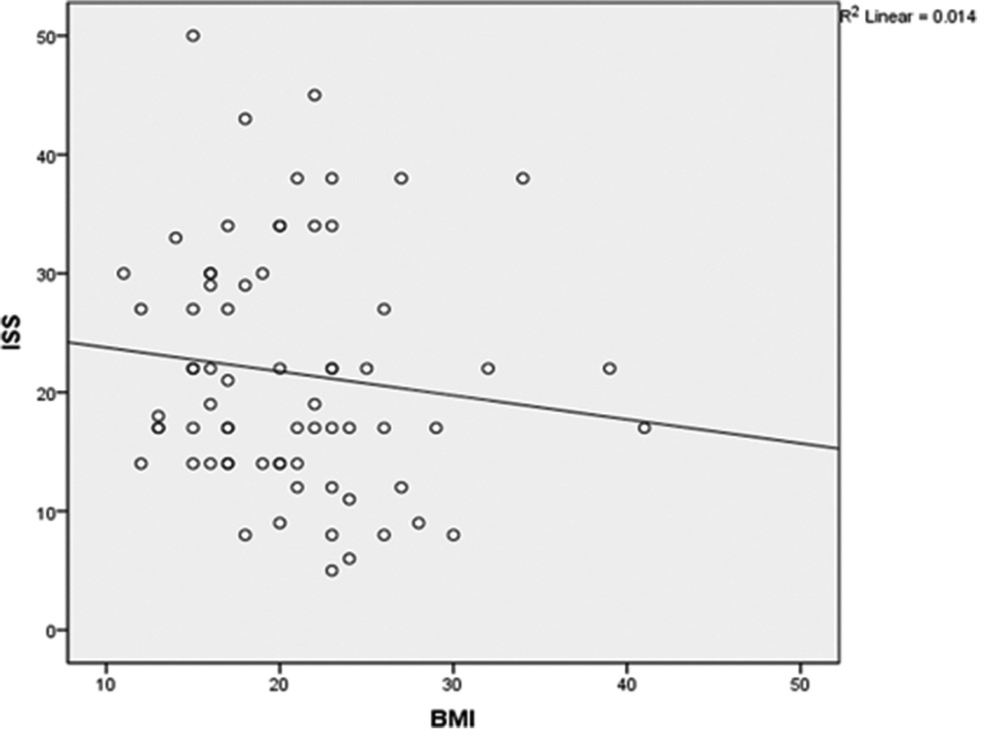
- Regression analysis model correlating injury severity scale and body mass index in pediatric orthopedic polytrauma patients.
In comparison to the normal weight group (25%), a trend of increased spine fractures was observed in the overweight/obese group (45.8%). However, this was not statistically significant [Table 2]. Pelvic fractures showed comparable results, whereas scapula fractures were marginally less frequent in the overweight/obese group compared to the normal weight group (4.2% and 8.3%, respectively). With regard to limb fractures, overweight/obese patients had more upper and lower limb fractures (66.7% each) compared to the normal weight group (47.2% upper limbs and 61.1% lower limbs).
| Variable | Normal weight group (5th –<85th percentile) (n=36) |
Overweight/obese group (>85th percentile) (n=24) |
P-value |
|---|---|---|---|
| Upper extremity fractures, (%) | 17 (47.2) | 16 (66.7) | 0.14 |
| Lower extremity fractures, (%) | 22 (61.1) | 16 (66.7) | 0.66 |
| Pelvic fracture, (%) | 12 (33.3) | 8 (33.3) | 0.60 |
| Spine fracture, (%) | 9 (25.0) | 11 (45.8) | 0.09 |
| Scapula fracture, (%) | 3 (8.3) | 1 (4.2) | 0.53 |
| ORIF, (%) | 9 (25.0) | 12 (50.0) | 0.05 |
| External fixator application, (%) | 1 (2.8) | 4 (16.7) | 0.06 |
ORIF: Open reduction internal fixation
Regarding post-operative complications, these were found to be minor and did not follow a specific pattern among the groups. All encountered complications were correlated separately with the BMI and ISS groups and were found not to be statistically significant.
The clinical outcomes of both groups are summarized in Table 3. The total length of hospital stay was significantly greater in the overweight/obese group compared to the normal weight group (19.1 ± 12.9 and 14.5 ± 15.58 days, respectively). Surprisingly, the overweight/obese group required less ICU LOS and a shorter duration of ventilation days compared to the normal weight group.
| Variable | Normal weight group (5th –<85th percentile) (n=36) | Overweight/obese group (>85th percentile) (n=24) | P-value |
|---|---|---|---|
| ICU LOS (Days), mean (±SD) | 5.7±13.1 | 3.5±4.5 | 0.42 |
| Ventilation days, mean (±SD) | 3.9±13.0 | 1.8±3.1 | 0.43 |
| Total hospital LOS (Days), mean (±SD) | 14.5±15.6 | 19.1±12.9 | 0.23 |
| Outcome, (%) | |||
| Alive | 33 (91.7) | 24 (100.0) | 0.15 |
| Deceased | 3 (8.3) | 0 (0.0) | |
| Home disposition, (%) | 27 (75.0) | 19 (79.2) | 0.34 |
| Transferred to long-term facility, (%) | 6 (16.7) | 5 (20.8) | 0.82 |
ICU: Intensive care unit, LOS: Length of stay, SD: Standard deviation
We investigated the need for orthopedic surgical intervention in the form of open reduction internal fixation (ORIF) or external fixator application between the groups. The results showed a significant increase of ORIF in overweight/obese young patients compared to the normal-weighted patients (P = 0.05). Regarding the external fixator application, the results were not statistically significant. However, surgical interventions, in the form of ORIF and/or external fixators, were applied more in the overweight/obese group. No statistically significant difference in mortality rates was observed between the groups. Regarding discharge disposition, most patients were discharged from the hospital and sent home.
DISCUSSION
The prevalence of childhood obesity has been rising at an alarming rate, particularly over the past few decades. Obesity’s relationship to trauma and orthopedic injuries has been studied extensively in the adult population and to a lesser degree, in the pediatric age group. Numerous research studies have employed BMI as a measurement tool to quantify and categorize weight status. In this study, we used the BMI age- and gender-specific CDC growth charts to categorize our patients. Few studies have reported specific findings related to orthopedic injuries and polytrauma in pediatric patients. Taylor et al.[15] performed a cross-sectional study investigating excessive weight and orthopedic outcomes in children and adolescents. Their results showed overweight and obese patients experienced a higher risk of fractures. The study also showed an increased prevalence of impaired mobility, musculoskeletal discomfort, and lower limb malalignment of both metaphyseal-diaphyseal and anatomic tibiofemoral angle measurements in the overweight and obese patient group.
Similarly, Rana et al.[5] conducted a retrospective review of 1314 pediatric trauma cases at a level 1 trauma center and recorded 294 obese patients. They found no significant difference in ISS and mechanism of injury between obese and non-obese patients. Furthermore, no significant differences were observed between obese and non-obese patients with regard to hospital LOS, ICU and ventilator days, or mortality. In addition, their cohort reported a significantly increased prevalence of extremity fractures in patients with an obese BMI record compared to the non-obese group (55% and 40%, respectively; P < 0.001). Their analysis showed an increased incidence of surgical intervention for fractures encountered in obese patients compared to non-obese patients (42% and 30%, respectively, P < 0.001). In consensus with published literature, this study reported an increased incidence of upper and lower limb fractures in obese children. It is postulated that higher forces are transmitted through the extremities of overweight and obese patients during impact and thus resulting in more extremities fractures.[16,17] This, in turn, resulted in an increased need for surgical intervention, in the form of ORIF and/or external fixator application, for the overweight/obese group. Furthermore, as seen in our results, there are paradoxical findings reporting lower ISS in overweight/obese patients. This could be explained by the cushion effect which proposes that the increased fat layer acts as an insulating tissue that absorbs part of the impact energy, thereby associating an increased BMI with less injury following trauma.[18] In addition, no clinical significance is seen between the mechanism of injury and ISS among our cohort, partly attributed to our small sample size.
Although decreased ICU LOS and fewer ventilation days were observed in the overweight/obese cohort, they experienced an overall lengthier hospital stay compared to non-obese patients (19.1 ± 12.9 and 14.5 ± 15.58 days, respectively). Furthermore, our findings showed an increased need for orthopedic surgical procedures in the form of ORIF for overweight and obese patients compared to non-obese patients (50% and 25%, respectively; P = 0.05). This could explain the reason for the longer total LOS in overweight and obese patients, as they had higher rates of orthopedic surgical intervention and subsequent post-operative physical therapy as inpatients before discharge.
Multiple retrospective studies have conveyed higher risks of pelvic and spine fractures ascribed to obese pediatric patients; however, these findings did not reach statistical significance when compared to non-obese patients.[5,10,17] This study showed a trend of increased spine fractures in the overweight/obese group compared to the normal weight group (45.8% and 25%, respectively). The implication of this trend results in increased surgical intervention. On the other hand, scapula fractures were found to be lower in obese patients compared to the normal weight group (4.2% and 8.3%, respectively). Fewer scapula fractures and lower prevalence of chest injuries occurring in overweight and obese patients might be partly explained by the cushion effect described by Arbabi et al.[18] and other authors in the literature. Hence, the normal weight group in our study had a higher rate of non-orthopedic (chest and abdominal) injuries that resulted in longer ICU stays and longer required ventilation days.
A large body of the literature has identified significant adverse outcomes in polytraumatized obese patients.[5,6] Adverse complications commonly encountered in obese patients include deep vein thrombosis, decubitus ulcers, postoperative fistulas, wound infections, and sepsis. Compared to the literature, we found the occurrence of complications to be minimal and did not follow a specific pattern between the two study groups. This could be attributed to this study’s relatively small sample size.
Limitations
This study is not devoid of limitations. One is the relatively small sample size for a quantitative study, which could limit the possibility of adverse complications. Second, this study is constrained by its retrospective design and single-site setting. Multi-centric prospective studies are needed to yield statistically significant outcomes that can be generalized to the pediatric orthopedic polytrauma population.
CONCLUSION
This study demonstrated a higher prevalence of spine and extremity fractures among the overweight/obese group, with comparable pelvic fractures between the two groups. Our findings demonstrate an increased need for surgical intervention for overweight/obese young patients. A slight inverse relationship between the BMI and ISS was noted. Considering the study results, obesity in pediatric polytrauma patients has been found to have a cushion effect with a favorable outcome, resulting in a comparably lower ISS than normal-weighted patients. Obesity in pediatric polytrauma patients leads to higher fracture prevalence, such as spine and extremities fractures, resulting in higher rates of surgical intervention, which, in turn, increases hospital LOS as a result of post-operative physiotherapy and rehabilitation. Contrarily, normal-weighted patients have higher ICU stays due to other system injuries. As such, obesity should be considered in decision-making when treatment plans are adjusted for the higher prevalence of certain types of fractures in obese children.
RECOMMENDATION
Orthopedic surgeons should be aware of the need for increased surgical intervention for obese pediatric polytrauma patients, noting this early on to recuperate their patient’s orthopedic health. Further research on how underweight pediatric polytrauma patients might differ in outcomes related to fracture prevalence and subsequent perioperative complications is also warranted to explore intervention strategies. Large multi-center prospective studies are required to investigate further relationships between obesity and other complications in pediatric orthopedic polytrauma patients. Orthopedic surgeons ought to be aware of the impacts of obesity on pediatric polytrauma patients to tailor surgical interventions based on evidence-based research.
AUTHORS’ CONTRIBUTIONS
AMD contributed to manuscript preparation, editing, review, literature research, and statistical analysis. AMA contributed to manuscript preparation and statistical review. AE contributed to data acquisition and literature research. HA contributed to data collection and data organization. TI was involved in conception, study design, and manuscript review. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Ethical approval has been granted by the Hamad Medical Corporation IRB with waiver of patient consent, reference number 16083 dated April 20, 2020.
DECLARATION OF PATIENT CONSENT
Patient’s consent was not required as there was a waiver of patient consent in this study.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing, editing, or review of the manuscript.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019;17:212.
- [CrossRef] [Google Scholar]
- The relationship of obesity to increasing health-care burden in the setting of orthopaedic polytrauma. J Bone Joint Surg Am. 2015;97:e73.
- [CrossRef] [Google Scholar]
- Obesity in orthopedics and trauma surgery. Orthop Traumatol Surg Res. 2014;100:S91-7.
- [CrossRef] [Google Scholar]
- Association between obesity and risk of fracture, bone mineral density and bone quality in adults: A systematic review and meta-analysis. PLoS One. 2021;16:e0252487.
- [CrossRef] [Google Scholar]
- Childhood obesity: A risk factor for injuries observed at a level-1 trauma center. J Pediatr Surg. 2009;44:1601-5.
- [CrossRef] [Google Scholar]
- The impact of obesity on severely injured children and adolescents. J Pediatr Surg. 2006;41:88-91.
- [CrossRef] [Google Scholar]
- Body mass index and injury risk among US children 9-15 years old in motor vehicle crashes. Inj Prev. 2008;14:366-71.
- [CrossRef] [Google Scholar]
- Does obesity impact the pattern and outcome of trauma in children? J Pediatr Surg. 2012;47:1404-9.
- [CrossRef] [Google Scholar]
- Severity of injury and outcomes among obese trauma patients with fractures of the femur and tibia: A crash injury research and engineering network study. J Orthop Trauma. 2009;23:634-9.
- [CrossRef] [Google Scholar]
- Obesity in trauma patients: Correlations of body mass index with outcomes, injury patterns, and complications. Am Surg. 2011;77:1003-8.
- [CrossRef] [Google Scholar]
- Complications with flexible nailing of femur fractures more than double with child obesity and weight >50 kg. J Child Orthop. 2009;3:53-8.
- [CrossRef] [Google Scholar]
- Effects of obesity on pediatric fracture care and management. J Bone Joint Surg Am. 2012;94:855-61.
- [CrossRef] [Google Scholar]
- The role of obesity in pediatric orthopedics. J Am Acad Orthop Surg Glob Res Rev. 2019;3:e036.
- [CrossRef] [Google Scholar]
- Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117:2167-74.
- [CrossRef] [Google Scholar]
- Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res. 2013;471:1199-207.
- [CrossRef] [Google Scholar]
- Injury patterns in obese versus nonobese children presenting to a pediatric emergency department. Pediatrics. 2010;125:681-5.
- [CrossRef] [Google Scholar]






