Translate this page into:
Therapeutic effects of mobilization in alleviating pain and improving shoulder mobility in adhesive capsulitis – A systematic review
*Corresponding author: Aqdas Shahzad, Department of Physiotherapy, Coventry University, Coventry, United Kingdom. aqdasshahzad39@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shahzad A, Azhar M, Zafar H, Khan MA, Shakir S. Therapeutic effects of mobilization in alleviating pain and improving shoulder mobility in adhesive capsulitis – A systematic review. J Musculoskelet Surg Res. 2024;8:97-107. doi: 10.25259/JMSR_54_2024
Abstract
Frozen shoulder (FS) is a painful clinical disease that lasts over three months and affects 3–5% of the general population. The main goal of this review was to show how mobilization techniques can affect FS treatment compared to other physiotherapy options. A systematic review of randomized controlled studies from CINAHL, MEDLINE, AMED, and PubMed published after 2010. Studies that included patients 18 or older with FS, but no other underlying systemic disorders were eligible. The review focused on two primary outcomes: Pain levels and how effectively patients could move their shoulders. The quality of the studies was assessed using the physiotherapy evidence database (PEDro) technique. Six randomized controlled studies with a PEDro score of 5/10 that met the study requirements were included. The pain was reduced in three of the five investigations with P < 0.05, whereas the remaining studies yielded neutral findings in lowering pain in patients with FS. All of the individuals’ range of motion (ROM) was evaluated. With P < 0.05, four of the six trials showed an improvement in shoulder ROM. Bending, straightening, moving arms away from the body, bringing them back in, internal rotation, and external rotation were all assessed and shown to be significant with P ≤ 0.05. Most studies suggested that patients, who have received mobilization treatment, experienced positive improvements. Techniques such as Mulligan mobilization, scapular mobilization, passive mobilization, and angular joint mobilization have proven effective in addressing pain and improving the ROM in individuals with FSs.
Keywords
Adhesive capsulitis
Frozen shoulder
Mulligan mobilization
Pain
Range of motion
INTRODUCTION
Frozen shoulder (FS), also known as adhesive capsulitis, presents as persistent pain and stiffness lasting over three months.[1] The term “frozen shoulder” was first used in 1934, later it was labeled as “Periarthritic scapulohumeral’ in 1945.[2] This condition affects 3–5% of the general population, with a heightened prevalence of 20% in diabetics[3] and is most commonly seen in manual workers aged 40–60.[4]
While all movement ranges are restricted in FSs, external rotation, abduction, and flexion are notably compromised. These symptoms often do not manifest radiologically. Although its exact cause is unknown, risk factors include diabetes, shoulder injuries, Parkinson’s disease, thyroid issues, stroke, and complex regional pain syndrome.[5,6]
Mobilization of the shoulder offers physiological benefits, including enhancing synovial fluid circulation, which nourishes the cartilage. This boost in circulation, derived from physical activities at the joint, is further amplified by mobilization, enriching the avascular cartilage. Moreover, mobilization expands joint space and mitigates nociceptive pathways in the brainstem, offering pain relief.[7] P. Nakandala et al. underlined the efficacy of manual therapy and physical therapy techniques, such as mobilization, in managing FSs.[8] Maitland mobilization is particularly beneficial in improving the range of motion (ROM) and alleviating pain in FS patients. Meanwhile, the Kaltenborn technique, a specialized mobilization stretch, has shown promise in enhancing joint flexibility, with both Kaltenborn and Maitland approaches demonstrating pain reduction and improved ROM in patients with FSs.[9,10]
Mobilization with movement (MWM), a manual therapy method pioneered by Mulligan, has been recognized for its prompt effects on musculoskeletal pain alleviation and enhancement in joint ROM.[11] On the other hand, the Cyriax approach is grounded in treating soft-tissue lesions, proving advantageous for conditions involving tears in tendons, muscles, bursae, and ligaments surrounding the joint. One of its renowned techniques is friction massage, which has been proposed as a remedial method for the musculoskeletal system.[12] A study by Guler-Uysal and Kozanoglu comparing the effects of the Cyriax approach with MWM, in conjunction with conventional therapies such as hot packs and short-wave diathermy, found that the Cyriax method exhibited promising outcomes in pain mitigation and ROM enhancement.[13]
While existing research acknowledges the potential benefits of mobilization, there remains a gap. A systematic review could offer a more profound insight into the impact of mobilization on FSs, thereby enriching the field and guiding future interventions where clear benefits have yet to be established.
This review’s research question was: what is the effect of mobilization on pain and ROM capacity in patients with FSs? The study’s primary goal was to assess the effectiveness of mobilization in alleviating pain and increasing ROM in patients with FSs. The study also aimed to determine the particular efficacy of mobilization strategies in relieving pain and enhancing ROM in these individuals. Finally, the researchers wanted to compare the outcomes of mobilization techniques to those of other physical therapy procedures used to treat FSs.
MATERIALS AND METHODS
This study used the positivist method, a quantitative approach that depends on empirical data and statistical analysis to set research objectives.
The researchers followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses standards in their work.
Eligibility criteria
The eligibility criteria for this study are based on the PICOS framework, where P represents the patient population, I denotes the intervention, C signifies the comparators, O specifies the outcome measures, and S indicates the study design. The PICOS for the present study is presented in Table 1.
| Inclusion | Exclusion | |
|---|---|---|
| Patients/problem | Patients >18 years of age Patients diagnosed as frozen shoulder/adhesive capsulitis by physicians. |
Underlying systemic disease Referred pain Other related musculoskeletal conditions Secondary frozen shoulder Frozen shoulder treated surgically |
| Intervention | Joint mobilizations alone Maitland/Mulligan/Klatenborn/Cyriax mobilization Joint mobilizations combined with other therapy |
|
| Comparison | Conservative treatment/ Placebo/sham intervention Other physical therapy intervention No intervention |
|
| Outcome | Pain and ROM rated on a standard questionnaire. Function measured by any method |
Absence of measure of pain and ROM |
| Study design | Randomized control trials |
ROM: Range of motion, PICOs: Patient, Intervention, Comparison, Outcomes
Justification of inclusion and exclusion criteria
Population
The population under research is made up of people who are at least 18-years-old. This age requirement was established based on the general population’s 3–5% occurrence of FS.[5] Furthermore, 20–30% of cases with FSs are bilateral.[14]
This research included all patients with shoulder discomfort, who were diagnosed with FS by a physician. There are, however, exclusion requirements. The existence of underlying systemic illnesses is an exclusion factor. This is due to the fact that a FS is frequently related to illnesses such as diabetes.[15]
Secondary FS, which can develop in individuals with impingement syndrome, was also an exclusion criterion.[16] Cases involving surgical interventions, such as manipulation under anesthesia, were also excluded from the research. This was done to avoid any misinterpretation of the study’s findings.[2]
Intervention
Joint mobilization is being tested as a therapy option in the clinical study, either alone or in conjunction with other conventional treatments. Maitland mobilization,[9] Kaltenborn mobilization, Cyriax mobilization,[17] and Mulligan mobilization[18] were specifically added to the study. These mobilization techniques were used on patients with FSs as solo therapies or as part of a combined therapy strategy, and they were included in the study’s inclusion criteria.
Comparator
For comparative purposes, conservative therapy is being investigated in this study. The control group may incorporate a variety of interventions, such as placebos or other treatments, but not mobilization. Other physical therapy therapies, such as transcutaneous electrical nerve stimulation (TENS), hot packs, joint stretching, and active exercises, as described,[19] may also be included in the research for comparison. Finally, the comparator group may contain a category in which no intervention was given.
Outcome
The systematic review emphasized two major components: pain and ROM. The pain was measured using a variety of tools, including the visual analog scale (VAS), the numeric pain rating scale (NPRS), and the shoulder pain and disability index (SPADI); ROM in the shoulder was measured using goniometry, which involved assessing movements to determine shoulder mobility.[20-22]
Study design
In this study, only randomized controlled trials (RCTs) were included, as specified by Whittal et al.[23]
Search strategy
The articles for this study were sourced from various databases, including CINAHL, Medline, AMED, and PubMed. Specific keywords were used to identify relevant articles, and searches were conducted through the search form provided by Coventry University. These databases were selected because they are specialized in health-related conditions. Each database was individually searched to maximize the number of articles retrieved for the study. The following search terms were used with Booleans AND, OR: Adhesive capsulitis, Frozen shoulder, Joint mobilization, Maitland mobilization, Mulligan mobilization, Kaltenborn mobilization, Cyriax mobilization, conservative treatment, conservative management, non-surgical, non-operative, placebo effect, pain, ROM, and flexibility.
Study selection
The authors thoroughly screened all the articles obtained from the databases, adhering to the predefined inclusion and exclusion criteria. A comprehensive analysis was undertaken on the pertinent articles that passed this first screening to determine their alignment with the complete eligibility requirements.
Quality appraisal tool
Various techniques are available for evaluating research quality, but the Physiotherapy Evidence Database (PEDro) tool is the most often utilized. It focuses on determining a study’s internal validity. The PEDro questionnaire has 11 questions, the first of which is not scored. As a result, it has a total of ten potential ratings, and the marks assigned to each item define its quality. The PEDro instrument is deemed valid and trustworthy for determining study quality in systematic reviews.[24]
Reliability of quality assessment tool
Two physiotherapists (AS and MA) used the PEDro instrument to evaluate the paper’s quality and ensure the author’s ability to use the assessment tool properly. This dual assessment technique gave strong proof of the author’s ability to use the assessment instrument properly.
Data extraction
Data extraction was carried out at the following levels:
Author/Year
Study design
Patient characteristics
Intervention
Outcome measures
Result
RESULTS
Study selection
The process of identifying and selecting articles for the review is illustrated in Figure 1. Initially, 37 records were identified through database searches, with 26 coming from CINAHL, 4 from Medline, 1 from AMED, and 6 from PubMed, after removing duplicate entries. During the screening phase, 22 articles were excluded, with 13 of them having interventions that were unrelated to the study’s focus. This left 15 articles that met the eligibility criteria. After further evaluation, six non-RCTs were excluded, and three full-text articles were also removed because they did not fulfill the inclusion criteria. Those studies were focused on different outcome measures compared to the predefined criteria. Ultimately, six studies were included in the quantitative synthesis and consequently were incorporated into this systematic review.
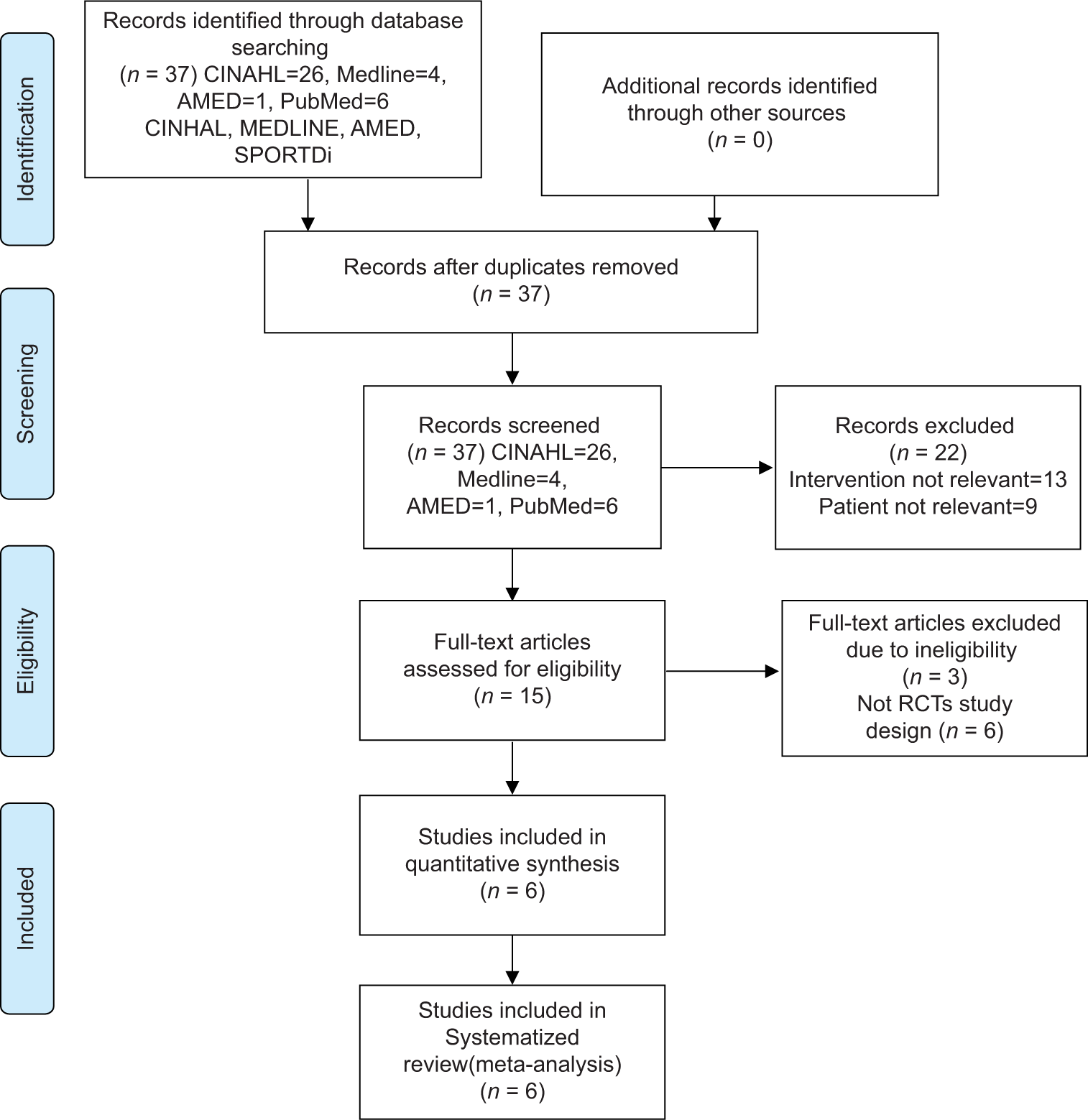
- PRISMA flow diagram. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. RCTs: Randomized controlled trials.
Study characteristics
The main points of all of the included studies are outlined in Table 2. All of these studies had both control and intervention groups. The intervention group received Mulligan mobilization, angular joint mobilization, passive mobilization, end-range mobilization, and scapular mobilization. In contrast, the control group underwent therapies such as the muscular energy method, capsular stretching, and traditional therapy.
| Authors/Year | Yang et al., 2011[32] | Doner et al., 2013[29] | Duzgun et al., 2019[33] | Noureen et al., 2021[30] |
Razzaq et al., 2022[28] | Yiasemides et al., 2022[31] |
|
|---|---|---|---|---|---|---|---|
| Study design | RCT | RCT | RCT | RCT | RCT | RCT | |
| Patient demographics | Number of participants n=32 CG: (10) Males 5 Females 5 Average age: 54.3 (7.6) years Criteria of CG: (12) Males 2 Females 10 Average age: 54.9 (10.3) years Criteria of IG: (10) Males 3 Females 7 Average age: 56.8 (7.2) years |
Number of participants n=40 IG: (20) Males 7 Females 13 Average age: 59.25 (9.17) years CG: (20) Males 2 Females 18 Average age: 58.55 (8.57) years |
Number of participants n=54 IG: (27) Average age: 51.2±9.08 years CG: (27) Average age: 53.04±7.8 years |
Number of participants n=50 IG: (25) Average age: 44.52 years CG: (25) Average age: 47.44 years |
Number of participants n=64 IG: (32) Average age: 49.93±6.69 years CG: (32) Average age: 49.17±8.92 years |
Number of participants n=98 IG: (47) Males 20 Females 27 Average age: 62 years CG: (51) Males 27 Females 24 Average age: 58 years |
|
| Intervention | CG: Subjects having larger shoulder kinematics received standard physiotherapy treatment Criteria CG: Subjects having small shoulder kinematics received standard physiotherapy treatment Criteria IG: Subjects having small shoulder kinematics received standard physiotherapy treatment and end range mobilization and scapular mobilization |
CG: Hot pack, TENS, and passive stretching exercises IG: Hot pack, transcutaneous electrical nerve stimulation and Mulligan’s technique |
Group 1: Scapular mobilization Group 2: Post Capsule stretching. Cross over was done and then combined treatment was given. |
IG: Angular joint mobilization applied for flexion, internal rot, external rot, abduction over 6 session/2 weeks CG: Anterior, posterior and inferior stretching over 6 session/2 weeks |
IG: Mulligan mobilization with movement and Conventional treatment, including hot packs for 10 min and wand exercises, pulley rope, shoulder wheel exercises and wall climbing exercises CG: Muscle energy technique and conventional treatment as well |
IG: Neuromuscular control exercises with passive mobilization at glenohumeral joint for 6 months CG: Neuromuscular control exercises for six months |
|
| Outcome measure | ROM Disability score Shoulder kinematics |
VAS AROM PROM Shoulder disability questionnaire |
ROM and Goniometry | NPRS SST SPADI Goniometry |
NPRS Goniometry Shoulder pain and disability index |
ROM SPADI And symptoms of pain |
|
| Results | Criteria IG showed improvement in ROM and shoulder kinematics (P<0.05) | IG showed improvement in pain, ROM and SPADI as compared to CG | Joint ROM improved after scapular mobilization and capsular stretching. (P<0.05) No difference created in both groups in terms of effectiveness (P>0.05) | IG showed more improvement in pain, ROM and function (P<0.05) | NPRS and SPADI was better in IG (P<0.05) | No statistical significant group in both groups by 1, 3, and 6 months | |
PICOs: Patient, Intervention, Comparison, Outcomes, RCT: Randomized controlled trial, IG: Intervention group, DOS: Duration of symptoms, CG: Control/Comparator group, VAS: Visual analogue scale, AROM: Active range of motion, PROM: Passive range of motion, NPRS: Numeric pain rating scale, SST: Simple shoulder test, SPADI: Shoulder pain and disability index, ROM: Range of motion, TENS: Transcutaneous electric nerve stimulation
Study design
All the RCT studies included in this review underwent quantitative analysis. Ultimately, six studies that met the eligibility criteria were added to this review for further analysis.
PEDro scale for methods studies
The internal validity of each study was evaluated using the PEDro scale, with each study receiving a score out of 10. The total score for all the included studies is represented in Table 3. Notably, all the studies scored 5–7 on the PEDro scale, indicating that they fulfilled eligibility criteria, had random allocation, and demonstrated baseline comparability. However, only one study employed concealed allocation and blinding of subjects. None of the studies included blinding of therapists in their methods.
| Authors/Year | Doner et al., 2013[29] | Razzaq et al., 2022[28] | Noureen et al., 2021[30] | Yiasemides et al., 2022[31] | Yang et al., 2011[32] | Duzgun et al., 2019[33] |
|---|---|---|---|---|---|---|
| Eligibility criteria | Yes | Yes | Yes | Yes | Yes | Yes |
| Random allocation | Yes | Yes | Yes | Yes | Yes | Yes |
| Concealed allocation | No | No | No | Yes | No | No |
| Baseline comparability | Yes | Yes | Yes | Yes | Yes | Yes |
| Blind subject | No | No | No | No | No | Yes |
| Blind therapists | No | No | No | No | No | No |
| Blind assessors | No | Yes | No | No | Yes | No |
| Adequate follow-up | Yes | Yes | No | Yes | Yes | Yes |
| Intention-to-treat analysis | Yes | Yes | Yes | Yes | Yes | Yes |
| Between-group comparisons | Yes | Yes | Yes | Yes | Yes | Yes |
| Point estimates and variability | Yes | Yes | Yes | Yes | Yes | Yes |
| Score (out of 10) | 6 | 7 | 5 | 7 | 7 | 7 |
It is important to highlight some major concerns regarding the quality of these studies, particularly the lack of blinding and concealed allocation in their methods. These aspects are under consideration, as they can impact the overall validity of the results.
All of the studies included in this evaluation stated that double-blinding was not used, and three of them used single-blinding for both participants and assessors.[25] It is critical to recognize that studies without blinding have the potential to introduce performance bias and overestimate results, especially when subjective outcomes are included as stated by Moher et al.[25] According to Savović et al.,[26] there might be a 13% exaggeration in outcomes when comparing unblinded research to double-blinded studies. However, the outcome difference between blinded and unblinded trials is not always substantial. When participant blinding is absent, the effectiveness of the intervention may be underestimated.
It is worth mentioning that different studies have come to different findings about the influence of blinding on effect magnitude. While some studies suggest that lack of blinding can affect the results, others argue that it may not significantly affect the overall effect size.[27]
Mobilization protocol
Razzaq et al.[28] compared Mulligan mobilization to standard treatment, which comprised 10 min of hot packs, wand exercises, pulley rope activities, shoulder wheel exercises, and wall climbing exercises.[28] Doner et al. conducted another trial in which the intervention group underwent Mulligan mobilization as well as passive stretching activities.[29] Noureen et al. compared active anterior and posterior stretching to angular joint mobilization.[30] Yiasemides et al. employed neuromuscular control exercises combined with passive mobilization at the glenohumeral joint in the intervention group.[31] Yang et al. used end-range and scapular mobilization strategies. Each of these studies used a distinct sort of mobilization and evaluated its efficacy by comparing it to other therapies.[32] The primary goal of this study is to evaluate if mobilization is an effective therapy for FSs. Importantly, all of the included studies found that mobilization is an effective treatment for FSs.
Control protocol
Many of the trials combined traditional therapy approaches with mobilization strategies. Conventional therapy includes hot packs for 10 min, pulley rope workouts, shoulder wheel exercises, and wall climbing activities, with follow-up sessions as shown in the study by Razzaq et al.[28] Hot packs, TENS, and passive stretching exercises were used by Noureen et al.[30] They also performed anterior, posterior, and inferior stretching across six two-week sessions. Yiasemides et al. incorporated neuromuscular control exercises over six months, and another study focused on posterior capsule stretching as part of the conventional treatment.[31] These studies combined mobilization with various conventional therapies to evaluate their effectiveness in treating FSs.
Outcome
Pain assessment techniques differed among studies. One study used the VAS to assess pain, whereas the other two used the NPRS. However, one study could not detect pain levels, while another recognized discomfort, especially during rest. In addition, one of the studies employed the SPADI pain score to assess pain levels.
The ROM was a common criterion measured in all of the investigations, and it included measures for flexion, extension, abduction, adduction, external rotation, and internal rotation. Furthermore, several of the studies used the SPADI to assess pain and disability related to the shoulder.
Effect of intervention
All the studies in this review measured the effect of mobilization on two main factors: Pain and ROM capacity. They reported P-values to indicate the statistical significance of the observed effects. In addition, effect sizes were calculated to provide insight into the magnitude of the intervention’s impact on these outcomes. This comprehensive approach allowed for a thorough assessment of the effectiveness of mobilization in addressing pain and improving the ROM in FS patients.
Mobilization for pain
The information on P-values and outcomes for various pain measurement methods, including the VAS, NPRS, SPADI pain score, and pain at rest are provided in Table 4. Overall, three out of six studies found that mobilization had a good impact, with Doner et al. finding a considerable improvement in pain levels. [29]
| Study | Outcome measure tool |
Group | Pre-treatment Mean±SD |
Post-treatment Mean±SD |
P-value | Between group P-value |
Posttreatment effect size | Outcome |
|---|---|---|---|---|---|---|---|---|
| Doner et al., 2013[29] | VAS | IG | 3.24 (2.19) | 0.20 (0.82) | 0.001 | 0.018 | 2.2 | Positive |
| CG | 3.43 (1.74) | 0.44 (0.63) | 0.001 | |||||
| Razzaq et al., 2022[28] | NPRS | IG | 0.56±0.56 | 1.15±1.05 | - | 0.00 | 3.2 | Positive |
| CG | 6.41±0.50 | 4.34±0.89 | ||||||
| Noureen et al., 2021[30] | NPRS | IG | - | 3.4±1.1 | - | <0.01 | 0.7 | Positive |
| CG | - | 4.4±1.7 | - | |||||
| Yiasemides et al., 2022[31] | SPADI Pain | IG | 38±22 | 29±22 | - | - | 0.02 | Neutral |
| score | CG | 18±20 | 18c20 | - | ||||
| Yang et al., 2011[32] | - | - | - | - | - | - | - | - |
| Duzgun et al., 2019[33] | Pain at rest | IG | - | 25±75 | - | 0.878 | - | Neutral |
| CG | - | 25±75 | - | |||||
| Combined | - | 25±75 | - |
SD: Standard deviation, VAS: Visual Analog Scale, NPRS: Numeric pain rating scale, SPADI: Shoulder pain and disability index, IG: Intervention group, CG: Control group
Mobilization for ROM
The results of all trials in terms of ROM, showing the particular benefits of Mulligan mobilization, angular joint mobilization, glenohumeral joint mobilization, and scapular mobilization are summarized in Table 5. Overall, the findings indicate that mobilization strategies successfully improved many elements of ROM in individuals with FSs.
| ROM | Study | Group | Pre-treatment Mean±SD |
Post-treatment Mean±SD |
P-value | Effect size post-treatment |
|---|---|---|---|---|---|---|
| Flexion | Doner et al, 2013[29] | IG | 121.25 (17.90) | 174.50 (8.41) | 0.001 | 1.2 |
| CG | 114.00 (19.30) | 157.75 (18.53) | ||||
| Razzaq et al., 2022[28] | IG | 75.56±8.02 | 166.31±17.01 | 0.00 | 3.1 | |
| CG | 75.37±13.64 | 107.17±20.93 | ||||
| Noureen et al., 2021[30] | IG | 165.0±7.5 | <0.01 | 3.3 | ||
| CG | 139.6±7.9 | |||||
| Yiasemides et al., 2022[31] | IG | 14±23 | 3±9 | 0.12 | ||
| CG | 19±19 | 3±6 | ||||
| Yang et al., 2011[32] | Cri I. | 31.7 (4.7) | 0.88 | - | ||
| CC | 30.8 (4.5) | - | ||||
| CI | 32.8 (4.4) | - | ||||
| Abduction | Duzgun et al., 2019[33] | IG | 132.6±13.4 | 140±11.3 | <0.001 | - |
| CG | 133±19.3 | 136.5±18.2 | - | |||
| Com G | 133±16.4 | 140±15.4 | - | |||
| Razzaq et al., 2022[28] | IG | 49.03±11.92 | 162.09±16.53 | 0.00 | - | |
| CG | 54.17±8.89 | 97.06±23.23 | - | |||
| Noureen et al., 2021[30] | IG | 149.0±12.7 | <0.01 | - | ||
| CG | 124.8±8.6 | - | ||||
| Yiasemides et al., 2022[31] | IG | 28±24 | 7±15 | 0.10 | ||
| CG | 36±25 | 6±11 | ||||
| Yang et al., 2011[32] | Cri I. | 99.5 (40.1) | 0.10 | - | ||
| CC | 88.8 (37.5) | - | ||||
| CI | 116.4 (27.3) | - | ||||
| Extension | Duzgun et al., 2019[33] | IG | 105±16.5 | 111±13.7 | <0.001 | - |
| CG | 102.5±20.3 | 110±17.3 | - | |||
| Com G | 104.3±20 | 113±16.7 | - | |||
| Razzaq et al., 2022[28] | IG | 12.09±4.97 | 58.00±12.73 | 0.00 | - | |
| CG | 12.41±3.72 | 30.20±14.72 | - | |||
| Noureen et al., 2021[30] | IG | 58.6±3.1 | <0.01 | - | ||
| CG | 50.0±7.3 | - | ||||
| Adduction | Doner et al., 2013[29] | IG | 92.30 (26.71) | 167.50 (21.73) | 0.001 | - |
| CG | 89.25 (21.17 | 137.50 (28.26) | - | |||
| Razzaq et al., 2022[28] | IG | 11.92±3.35 | 57.18±18.01 | 0.00 | - | |
| CG | 11.51±3.90 | 28.68±11.89 | - | |||
| External rotation | Doner et al., 2013[29] | IG | IG | 25.50 (12.55) | 0.041 | - |
| CG | CG | 29.75 (17.20) | - | |||
| Noureen et al., 2021[30] | IG | - | 59.0±8.5 | <0.01 | - | |
| CG | - | 46.4±5.2 | - | |||
| CG | - | - | - | |||
| Yang et al., 2011[32] | Cri I. | - | 31.7 (12.9) | 0.04 | - | |
| CC | - | 34.7 (19.3) | - | |||
| CI | - | 44.3 (17.4) | - | |||
| Duzgun et al., 2019[33] | IG | 36±15 | 40.4±14.5 | <0.001 | - | |
| CG | 39.3±19 | 42.3±20.4 | - | |||
| Com G | 38±17.4 | 43.3±17.7 | - | |||
| Internal rotation | Doner et al., 2013[29] | IG | 32.50 (11.75) | 86.50 (7.45) | 0.001 | - |
| CG | 36.25 (20.70) | 32.50 (11.75) | - | |||
| Com G | - | - | ||||
| Yang et al., 2011[32] | Cri I. | 38.3 (19.5) | 0.24 | - | ||
| CC | 33.3 (18.1) | - | ||||
| CI | 49.0 (6.3) | - | ||||
| Duzgun et al., 2019[33] | IG | 48.8±16.5 | 46.7±15.7 | 0.106 | - | |
| CG | 51.4±18.2 | 55±18 | - | |||
| Com G | 49.7±16.4 | 55±18 | - |
SD: Standard deviation, IG: Intervention group, CG: Control group, Com G: Combined group, Cri I: Criteria control group, ROM: Range of motion
DISCUSSION
The impact of mobilization as a therapy for FS was investigated in all of the studies included in this review. Three of the six trials found that mobilization had a favorable effect on pain levels in individuals with FSs. However, two trials revealed that mobilization did not affect pain. Based on these findings, we can consider mobilization as a treatment option for FS. Nonetheless, it is crucial to carefully consider the methods and limitations of the studies included in the review when interpreting these results. The variability in study outcomes may be influenced by factors such as the specific mobilization techniques used, the duration of treatment, and the patient populations studied.
Doner et al.[29] found that Mulligan mobilization (n = 20) reduced pain more than conventional treatment (n = 20) in a short-term RCT, but the study quality was moderate, with a PEDro score of 6/10, Razzaq et al.[28] demonstrated that combining conventional treatment with mobilization (n = 32) was more effective in reducing pain than muscle energy techniques (n = 32) alone (P < 0.001). However, the study quality was moderate with a PEDro score of 7/10 and lacked concealed allocation.[29]
Noureen et al.[30] found that angular mobilization (n = 25) was significantly effective in reducing pain compared to stretching (n = 25), as per NPRS (P < 0.001). However, like Doner et al.[29] and Razzaq et al.,[28] the study had quality limitations due to missing concealed allocation and blinding, scoring only 5/10 on the PEDro scale. The absence of adequate follow-up further compromises the reliability of its outcomes.
Mobilization techniques, including scapular and glenohumeral interventions, appear promising in alleviating FS pain.[31,33] However, study quality and design inconsistencies, such as blinding and concealed allocation, influence interpretations.[28-30] The underlying mechanism might be attributed to the neurophysiological effects where mobilization activates mechanoreceptors and inhibits nociceptors, providing pain relief.[34] A thorough systematic review on this subject is notably missing, emphasizing a research opportunity.
Most reviewed studies indicate that mobilization techniques, especially Mulligan mobilizations, effectively improve the flexion ROM in patients with FSs. Out of the six studies assessing flexion ROM, five noted improvements. Mulligan mobilizations consistently demonstrated efficacy in both studies where they were implemented.[29,28] While one study evidenced a positive outcome with scapular mobilizations,[33] another indicated neutral effects.[32] Furthermore, Duzgun et al.[33] showed an 8-degree improvement in flexion after scapular mobilization, a finding mirrored by Surenkok et al.[35] Meanwhile, studies utilizing passive mobilizations and glenohumeral joint mobilizations showed mixed results: one presented positive results,[30] and the other depicted neutral outcomes.[31] These findings, even with some methods limitations in certain studies, accentuate the potential therapeutic significance of mobilization methods for FS treatment.
Most studies reviewed have indicated that different mobilization techniques can improve abduction ROM in FS patients. Specifically, Mulligan mobilizations effectively improved abduction ROM.[28] Angular joint mobilizations also showed positive results for abduction ROM despite the study’s lower quality.[30] Scapular mobilizations yielded mixed outcomes: one study found a 6-degree improvement in abduction,[33] echoing findings from Surenkok et al.[35] Conversely, Yang et al.[32] did not observe a significant increase in abduction ROM. Notably, Yiasemides et al.[31] (n = 98) showed neutral effects for glenohumeral joint mobilizations. Overall, while various mobilizations positively impacted abduction ROM, results were not uniformly consistent across all studies.
The limited research available indicates that specific mobilization techniques, such as Mulligan mobilization, are effective in improving the extension ROM in patients with frozen shoulders. Razzaq et al.[28] and Noureen et al.[30] both found significant improvements in extension ROM following their respective interventions, with P < 0.05. It is noteworthy that the quality of Noureen et al.[30] was lower and that blinding was not consistently followed in studies employing Mulligan mobilizations. Overall, the evidence suggests a positive effect of mobilization techniques on extension ROM in FSs, but more comprehensive research is required to solidify these findings.
The limited research available underscores Mulligan mobilization’s effectiveness in improving adduction ROM in FSs. Both Doner et al.[29] and Razzaq et al.[28] studies demonstrated significant improvements in adduction ROM after employing this technique, with P < 0.05. Both studies endorse the positive impact of Mulligan mobilization, and it emerges as a promising intervention for enhancing adduction ROM in FSs, even though further expansive research is warranted to solidify these outcomes.
When evaluating the external rotation ROM in patients with FSs, there is a consistent indication of improvement across the reviewed studies. Specifically, Mulligan mobilization, employed in the studies by Doner et al.[29] and Noureen et al.[30] demonstrated positive results, although with some method concerns, such as the absence of blinding. Similarly, Yang et al.[32] and Duzgun et al.[33] found improvements in external rotation, with their findings reinforced by respective PEDro scores of 7/10. The effectiveness of both scapular and passive mobilizations in enhancing external rotation was also consistent across studies. These findings collectively highlight the efficacy of various mobilization techniques in ameliorating external rotation in a FS. However, further research with rigorous methods is essential for a more comprehensive understanding.
Mixed results have been noted when reviewing the effectiveness of various mobilization techniques on the internal rotation ROM in patients with FSs. Doner et al.[29] presented a significant improvement in internal rotation when Mulligan mobilization was employed, as evidenced by P = 0.001. Conversely, in the latter study, Yang et al.[32] and Dugzun et al.[33] reported no significant improvements in internal rotation despite slight increases in degrees of rotation.
Although Mulligan mobilization showed a positive outcome in one study, scapular mobilizations and other techniques did not yield universally consistent results. Thus, it appears that while some mobilization techniques can enhance internal rotation in FS cases, further rigorous and extensive research is required to establish a consistent and effective therapeutic approach.
This systematic review emphasizes the critical role of clinical research in transforming knowledge into practical applications for clinical practitioners, which is consistent with the ideas outlined in recent literature.[36] Practically, therapists can incorporate mobilization techniques to alleviate pain and enhance shoulder mobility in patients with FSs. Personalized application of these evidence-based interventions ensures a tailored and effective physiotherapeutic approach in clinical practice.
Limitations
Due to the short timeframe of the study, gray literature or non-English literature was not investigated. Furthermore, the effect of Cyriax, Maitland, and Kaltenborn mobilizations was not measured because no literature was provided. The study also has a limitation in terms of contacting authors. In studies, using the VAS for pain assessment introduces potential subjectivity and variability inherent in self-reported measures, influencing the interpretation of pain outcomes. Despite RCT design consistency, variability in intervention protocols and outcome measures hindered meta-analysis. Inconsistent reporting and outcome measure heterogeneity posed challenges for data synthesis and meta-analysis.
CONCLUSION
It is evident that mobilization techniques, including Mulligan, scapular, and angular joint mobilizations, yield promising results for FS patients. Notably, these treatments have demonstrated a marked reduction in pain spanning from six weeks to six months, alongside notable enhancements in the ROM across various axes: flexion, extension, abduction, adduction, external rotation, and internal rotation. In essence, mobilization stands out as a beneficial and effective approach to addressing both pain and mobility challenges associated with a FS.
It is reassuring to note the absence of reported adverse effects, underscoring the safety of the treatment. However, while these findings are promising, there is still room for exploration, especially regarding the potential impacts of other mobilization techniques, such as Cyriax, Maitland, and Kaltenborn, on FS management.
Recommendations
This systematic study suggests that mobilization, alone or in combination with other treatments, has the potential to improve function, reduce discomfort, and increase ROM capability in patients with FSs. Furthermore, more studies, such as RCTs, on Cyriax, Maitland, and Kaltenborn mobilizations and their effects on FSs should be conducted. The PEDro should increase the quality of future studies. Future studies should prioritize standardized intervention protocols and outcome measures to facilitate meta-analysis.
ACKNOWLEDGMENT
The authors would like to sincerely thank the research supervisor for his continuous support and guidance.
AUTHORS’ CONTRIBUTIONS
AS contributed to the conception and study design; MA, HZ, and MAK contributed to the literature search and data extraction; SS contributed to data extraction and quality assessment of articles. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study has received ethical approval from Coventry University, with reference number P127725 (29 October 2021).
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Treatment strategy for frozen shoulder. Clin Orthop Surg. 2019;11:249-57.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1:180-9.
- [CrossRef] [PubMed] [Google Scholar]
- Frozen shoulder: A systematic review of therapeutic options. World J Orthop. 2015;6:263.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: A systematic review. J Back Musculoskelet Rehabil. 2021;34:195-205.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of Maitland techniques in idiopathic shoulder adhesive capsulitis. Int Sch Res Notices. 2012;2012:710235.
- [CrossRef] [Google Scholar]
- Comparison of Maitland and Kaltenborn mobilization techniques for improving shoulder pain and range of motion in frozen shoulders. J Phys Ther Sci. 2015;27:1391-5.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of Mulligan mobilization on pain and life quality of patients with Rotator cuff syndrome: A randomized controlled trial. J Back Musculoskelet Rehabil. 2019;32:171-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of friction massage versus capsular stretching in adhesive capsulitis-a randomized active controlled study among coastal patients. J Coast Life Med. 2023;11:2409-19.
- [Google Scholar]
- Comparison of the early response to two methods of rehabilitation in adhesive capsulitis. Swiss Med Wkly. 2004;134:353-8.
- [Google Scholar]
- Functional improvement of bilateral frozen shoulder by unilateral intraarticular corticosteroid injection: A retrospective study. J Int Med Res. 2021;49:3000605211050535.
- [CrossRef] [PubMed] [Google Scholar]
- Review of diabetic frozen shoulder. Eur J Orthop Surg Traumatol. 2018;28:363-71.
- [CrossRef] [PubMed] [Google Scholar]
- The management of shoulder impingement and related disorders: A systematic review on diagnostic accuracy of physical tests and manual therapy efficacy. J Bodyw Mov Ther. 2019;23:604-18.
- [CrossRef] [PubMed] [Google Scholar]
- Gong's mobilization versus cyriax manipulation on range of motion and function recovery in subject with frozen shoulder"-a comparative study. Int J Dev Res. 2017;7:13260-8.
- [Google Scholar]
- The initial effects of a Mulligan's mobilization with movement technique on range of movement and pressure pain threshold in pain-limited shoulders. Man Ther. 2008;13:37-42.
- [CrossRef] [PubMed] [Google Scholar]
- Manual therapy and exercise for adhesive capsulitis (frozen shoulder) Cochrane Database Syst Rev. 2014;2014:CD011275.
- [CrossRef] [Google Scholar]
- The visual analogue scale: Its use in pain measurement. Rheumatol Int. 1985;5:145-8.
- [CrossRef] [PubMed] [Google Scholar]
- Shoulder pain and disability index (SPADI) J Physiother. 2011;57:197.
- [CrossRef] [PubMed] [Google Scholar]
- Responsiveness of the numeric pain rating scale in patients with shoulder pain and the effect of surgical status. J Sport Rehabil. 2011;20:115-28.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of obsessions: A randomized controlled trial. Behav Res Ther. 2010;48:295-303.
- [CrossRef] [PubMed] [Google Scholar]
- Using research to guide practice: The physiotherapy evidence database (PEDro) Braz J Phys Ther. 2020;24:384-91.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Ann Intern Med. 2012;157:429-38.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of blinding on estimated treatment effects in randomised clinical trials: Meta-epidemiological study. BMJ. 2020;368:l6802.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing the effects of muscle energy technique and mulligan mobilization with movements on pain, range of motion, and disability in adhesive capsulitis. J Pak Med Assoc. 2022;72:13-6.
- [CrossRef] [PubMed] [Google Scholar]
- Evalution of Mulligan's technique for adhesive capsulitis of the shoulder. J Rehabil Med. 2013;45:87-91.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of three directional capsular stretching versus angular joint mobilization in patients with frozen shoulder: A randomized controlled trial. Edit Adv Board. 2021;15:212.
- [CrossRef] [Google Scholar]
- Does passive mobilization of shoulder region joints provide additional benefit over advice and exercise alone for people who have shoulder pain and minimal movement restriction? A randomized controlled trial. Phys Ther. 2011;91:178-89.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of the end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: A randomized control trial. Man Ther. 2012;17:47-52.
- [CrossRef] [PubMed] [Google Scholar]
- Which method for frozen shoulder mobilization: Manual posterior capsule stretching or scapular mobilization? J Musculoskelet Neuronal Interact. 2019;19:311-6.
- [Google Scholar]
- Basic principles of extremity joint mobilization using a Kaltenborn approach. J Sport Rehabil. 2002;11:235-50.
- [CrossRef] [Google Scholar]
- Acute effects of scapular mobilization in shoulder dysfunction: A double-blind randomized placebo-controlled trial. J Sport Rehabil. 2009;18:493-501.
- [CrossRef] [PubMed] [Google Scholar]
- Is clinical research as helpful to clinicians as it could be? Phys Ther. 2023;103:pzad060.
- [CrossRef] [PubMed] [Google Scholar]






