Translate this page into:
Two-stage bone lengthening of the tibia through a normal bone and consolidated regenerate bone after trauma: A case report and literature review
Corresponding Author:
Akram D Al-Shoubaki
Department of Trauma and Orthopaedic Surgery, Al-Essra Hospital Outpatient Clinics (Level 3), Al-Essra Hospital, Queen Rania Street, Amman
Jordan
dr_shoubak@yahoo.com
| How to cite this article: Shobaki SD, Al-Shoubaki AD. Two-stage bone lengthening of the tibia through a normal bone and consolidated regenerate bone after trauma: A case report and literature review. J Musculoskelet Surg Res 2020;4:42-51 |
Abstract
We report a case of two-stage leg lengthening of the tibia through the normal tibial bone followed by a 2nd stage lengthening through the consolidated regenerate bone using Ilizarov external fixator. A 10-year-old boy presented with multiple fractures, including a Gustilo IIIC open tibial fracture with neurovascular injury and 11 cm bone defect. Surgical debridement and acute shortening using a triangular external fixator were performed. After wounds healing, this was replaced by an Ilizarov circular frame, with a proximal tibial osteotomy performed to start distraction osteogenesis. Leg lengthening of 5.9 cm was achieved after 10.5 months of total external fixator time. Fourteen months after first frame removal, a 2nd stage leg lengthening was performed with an Ilizarov circular frame through an osteotomy of the consolidated regenerate bone in the proximal tibia to achieve further 6.1 cm leg lengthening after 6.2 months of total external fixator time. The second leg lengthening stage united faster than the first stage with reduced external fixator time and index. The patient had a good functional outcome assessed by the Association for the Study and Application of the Methods of Ilizarov criteria at 6 months' follow-up. A literature review was performed for a proposed research question about the treatment of such cases shows that this method is an acceptable way of treatment. To the best of our knowledge, there are no cases reported in English literature that reports a 2nd stage leg lengthening of the tibia through the consolidated regenerate bone after a first stage leg-lengthening for treatment of open tibial fracture with bone loss.Introduction
Open tibial fractures are common fractures, and bone loss in comminuted fractures can produce a dilemma for orthopedic surgeons.[1] These fractures should be managed by a multidisciplinary team in a specialized tertiary center. The presence of senior orthopedic and plastic surgeons is of paramount importance for the management of these cases and for surgical planning.[2],[3] Surgical debridement and acute shortening of open tibial fractures can aid soft tissue coverage and bone healing and have been documented in the literature as a good option. After the initial treatment, bone lengthening through an osteotomy of the normal proximal tibia using a circular external fixator has been used to correct leg length and alignment.[4],[5],[6],[7]
To our knowledge, a 2nd stage of leg lengthening through a consolidated regenerate bone after a first stage leg lengthening for the treatment of open tibial fracture with bone loss has not been documented in the literature.
The aim of this article is to report a case of open tibial fracture with bone loss and extensive soft tissue injury; where we adopted a method of two-stage leg lengthening of the tibia through an osteotomy of normal proximal tibial bone followed by the lengthenisng through an osteotomy of the consolidated regenerate bone from the first stage using Ilizarov ring external fixator. We also aim to report a literature review of leg lengthening using a circular frame as a treatment of open tibial fractures with bone loss and soft tissue injury following the initial surgical debridement and acute shortening of the leg.
Case Report
A 10-year-old boy presented to our hospital after being hit by a car on his way to school. ATLS® protocol was initiated on arrival. His vital signs were stable. A rigid neck collar was applied and not removed for clinical assessment due to neck pain and suspicion of cervical spine injury. Bleeding from an obvious left leg open tibial fracture was packed with saline-soaked gauze, and compression bandage and both legs were splinted [Figure - 1] and [Figure - 2]. Neurological assessment was done with a Glasgow coma score of 15/15, with good sensation in all limbs except for the left foot. He was given IV antibiotics as per hospital protocol. Primary survey radiographs for chest and pelvis revealed normal lung shadow, right humeral neck fracture and normal pelvic bones. A focused trauma computed tomography scan was performed and revealed an unstable cervical (C7) fracture with posterior retropulsion and spinal cord compression, splenic laceration with contained splenic hematoma, and no chest or pelvic injuries [Figure - 3]a.
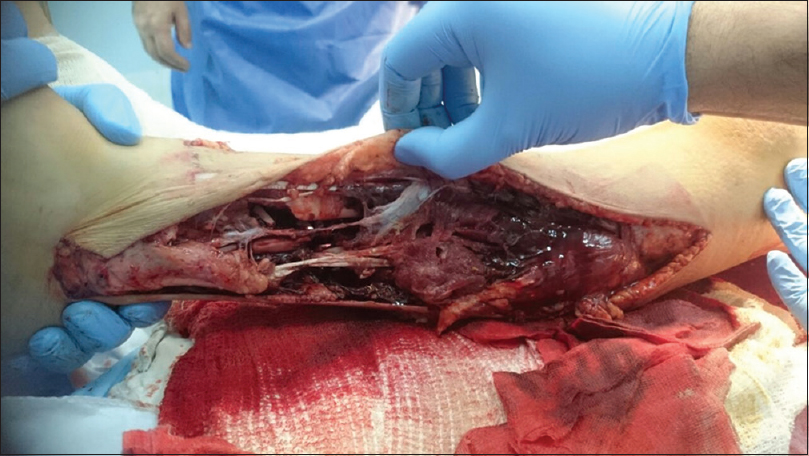 |
| Figure 1: Lateral aspect of the left leg |
 |
| Figure 2: Medial aspect of the left leg |
 |
| Figure 3: (a) C7 fracture with posterior retropulsion, (b) computed tomography reconstruction images showing both lower leg fractures around the knees, (c) right humeral neck fracture, (d) right leg floating knee injury |
The patient was taken immediately to operating theatre for the initial management of his left leg open tibial fracture in the presence of the plastic and vascular surgeons. He sustained a Gustilo IIIC open tibial fracture with neurovascular injury and extensive soft tissue loss of his left leg. He also had multiple fractures including: Supracondylar fracture of left femur with posterior displacement (AO classification: complete distal metaphyseal fracture 33-M/3.2),[8] supracondylar fracture of right femur with posterior displacement (Complete distal metaphyseal fracture 33-M/3.2),[8] right tibial plateau and proximal fibula fracture (Proximal epi/metaphyseal tibial fracture Salter-Harris Type IV (41t-E/4.2) and complete metaphyseal fibular fracture (41f-M/3.2)[8] and right proximal humerus fracture (Complete proximal metaphyseal fracture 11-M/3.2)[8] [Figure - 3]b, [Figure - 3]c, [Figure - 3]d.
There were two wounds; lateral and anteromedial sides of the left leg. The lateral side was extending from the level of the head of the fibula to the lateral malleolus measuring about 30 cm × 4 cm [Figure - 1]. Anteromedial side extending from upper third of the calf muscle to the anterior ankle joint line measuring about 20 cm × 5 cm, separated anteriorly by a 3 cm skin bridge and posteriorly by a 1 cm skin bridge that looked nonviable [Figure - 2]. After initial assessment in theatres, the foot had absent dorsalis pedis pulse, intact pulseless posterior tibial artery with intact tibial nerve, complete cut of the peroneal artery, and nerve at the fracture site. There was a proximal vascular injury at the level of the popliteal artery from the posterior displacement and angulation of the femoral supracondylar fracture; for which a bypass was performed followed by a repair of the peroneal artery by the vascular surgeon. Multiple cut tendons were encountered with intact Achilles tendon. Multiple bone fragments were lost from the tibia and fibula. A thorough washout and surgical debridement of the soft tissues and the bones were performed. A temporary joint-bridging triangular external fixator (as illustrated by the AO Foundation online Surgery Reference)[9] was applied to stabilize the left tibia and allow soft tissue management [Figure - 4]a and [Figure - 4]b. Acute shortening was performed due to a small defect of 5 cm at the initial operation, followed by further shortening within a week due to loss of viability of loose bone fragments and to aid soft tissue cover of the leg. The final bone defect was about 11 cm.
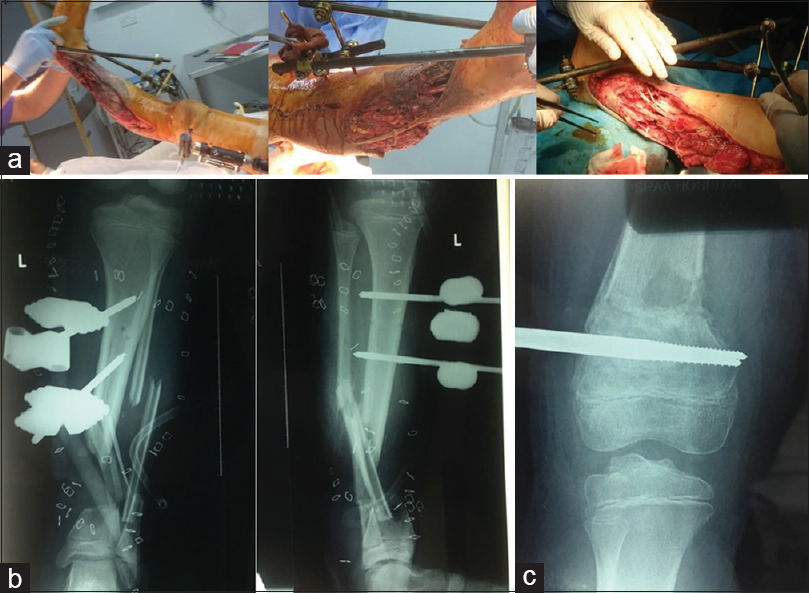 |
| Figure 4: (a) Joint-bridging triangular external fixator on left lower leg and a unilateral external fixator on the left femur, (b) radiographs of joint-bridging triangular external fixator on left lower leg showing the bone defect of the tibia, (c) radiograph showing the reduction of left femur supracondylar fracture with unilateral external fixator |
The left femur supracondylar fracture was closely reduced and fixed with a unilateral external fixator [Figure - 4]a and [Figure - 4]c. The right knee was managed by closed reduction and Kirschner-wires fixation of the femoral supracondylar fracture and an above-knee plaster [Figure - 3]d. The patient underwent anterior C7 corpectomy and cage insertion 1 day later [Figure - 5]. He underwent multiple wound debridement procedures by the plastic surgeon until all wounds were clean and ready for split skin grafts 2 weeks later.
 |
| Figure 5: Anterior cervical C7 corpectomy and cage insertion |
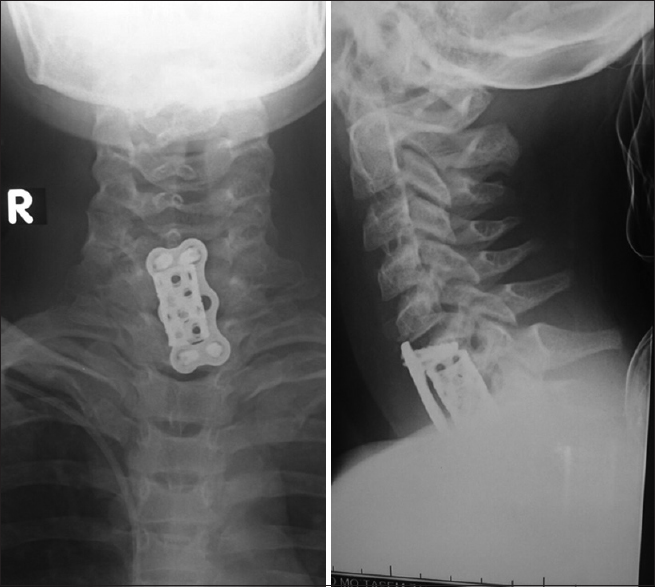
One month after the primary injury, all wounds have healed. The temporary external fixator was replaced by an Ilizarov circular frame on day 35 after the injury, with a proximal tibial osteotomy performed to start the first stage of distraction osteogenesis [Figure - 6]a. The frame was used in compression mode at the fracture site. The distraction commenced at a rate of 1 mm/day for 2 weeks then increased to 1.5 mm/day for 30 days due to pain at the osteotomy site, which indicated premature union. The distraction time was 44 days; achieving leg lengthening of 5.9 cm [Figure - 6]b. Bone union was achieved after 9 months following the distraction period with a total external fixator time of 10.5 months [Figure - 6]c. The healing index expressed by distraction–consolidation time (time to bony union) per centimeters of lengthening was 1.5 months/cm (9 months/5.9 cm = 1.5). The external fixator index expressed by the time the fixator was on the bone in days per centimeter of length gained was 53 days/cm (315 days/5.9 cm = 53). The Ilizarov frame was removed, leaving the patient with a Limb Length Discrepancy (LLD) of approximately 5.1 cm. The patient was left without any metalwork, fully weight-bearing, and extensive physical therapy was initiated. The LLD was compensated with a shoe raise [Figure - 6]d. A convalescence period of 14 months allowed for full consolidation of the regenerate bone of the tibia, increase the range of movements of the joints and muscles and tendons rehabilitation.
 |
| Figure 6: (a) Proximal Tibial osteotomy through normal tibial bone, (b) distraction osteogenesis of the proximal tibia, (c) consolidated regenerate bone of the proximal tibia, (d) full consolidation of the regenerate bone of the tibia |
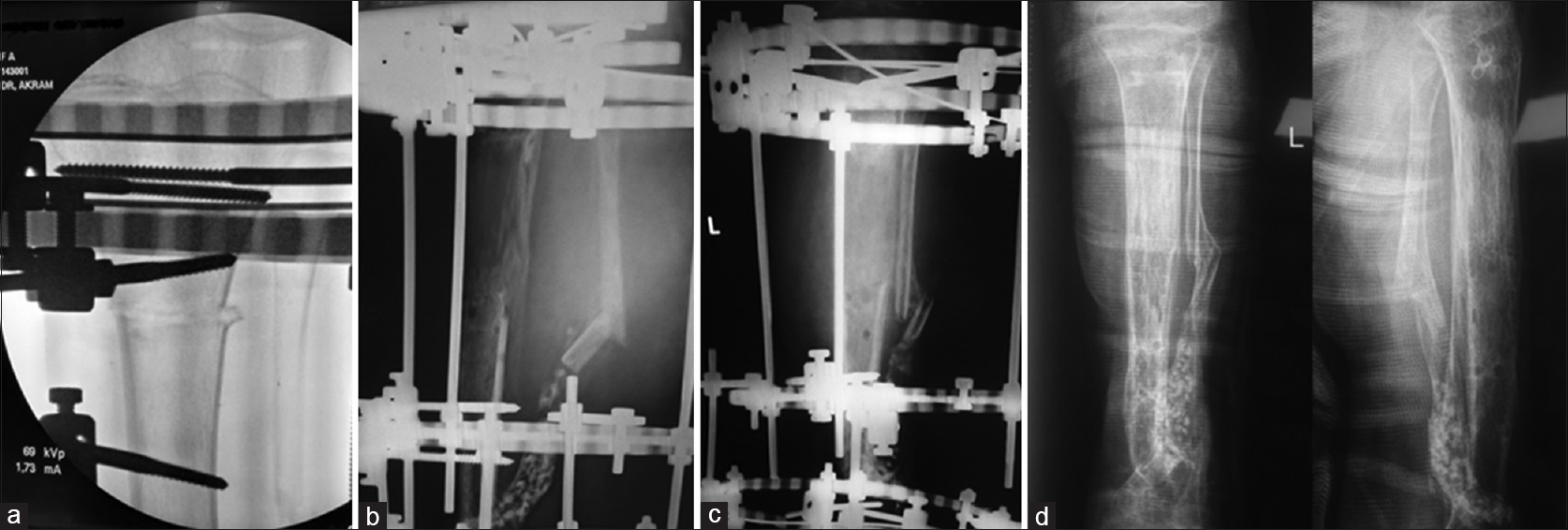
A 2nd stage of leg lengthening was planned after full consolidation of the regenerated bone of the proximal tibia. The LLD was 6.2 cm after 14 months of the removal of the first Ilizarov frame due to growth around the knee. The left tibia was 5.5 cm shorter than the right one. This 2nd stage was performed by an Ilizarov frame and distraction osteogenesis through an osteotomy of the consolidated regenerate bone of the proximal tibia. The distraction commenced at a rate of 1 mm/day for 2 weeks, then increased to 1.5 mm/day for 32 days. The distraction time was 46 days; achieving leg lengthening of 6.1 cm. Bone union was achieved after 4.7 months following the distraction period with a total external fixator time of 6.2 months. The healing index was 0.77 months/cm. The external fixator index was 30 days/cm. Further 6.1 cm leg length was gained by this 2nd stage bringing the LLD to 0.1 cm. Consecutive radiographs of this 2nd stage leg lengthening through the consolidated regenerate bone of the proximal tibia are shown in [Figure - 7]. The second Ilizarov frame was removed, and the patient was left without any metalwork. He started fully weight-bearing with extensive physical therapy. [Figure - 8]a and [Figure - 8]b show the last radiographs after the 2nd stage leg lengthening through the consolidated regenerate bone of the proximal tibia, with good consolidation and congruent ankle joint.
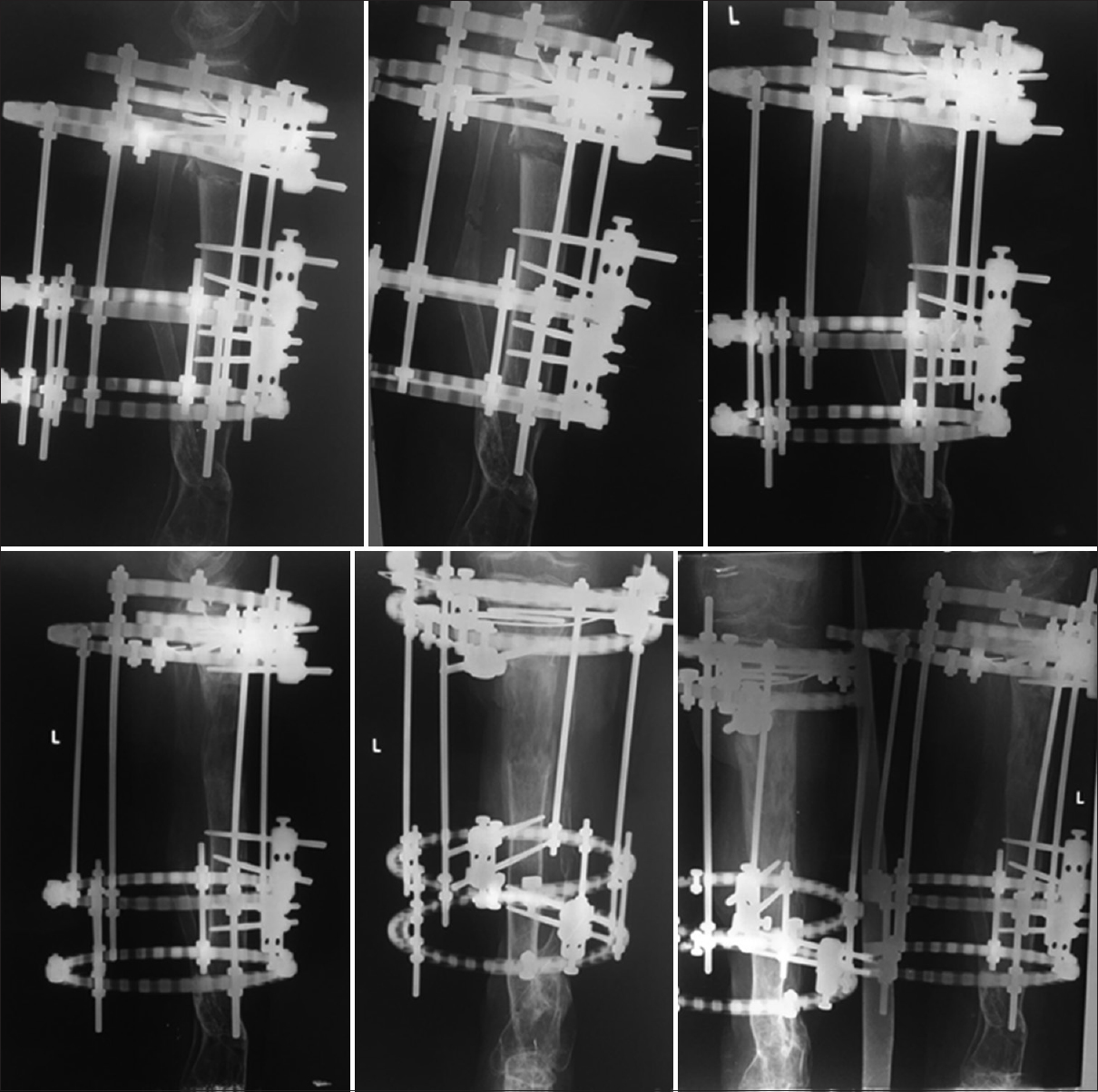 |
| Figure 7: Consecutive radiographs of the 2nd stage leg lengthening through the consolidated regenerate bone of the proximal tibia, with good consolidation in the last radiograph |
 |
| Figure 8: (a) Final radiograph after the 2nd stage leg lengthening through the consolidated regenerate bone of the proximal tibia, with good consolidation, (b) final radiographs of the ankle joint shows joint congruity maintained, (c) final clinical pictures of the lower leg (showing passive dorsiflexion of the ankle joint) |
There have been minor complications of pin site infection and limitation of ankle movement due to the presence of peroneal nerve cut at the fracture site with drop foot and contracture of the Achilles tendon [Figure - 8]c. Although the first Ilizarov frame included an ankle frame to keep the foot in plantigrade position, poor compliance with the use of the dynamic ankle-foot orthosis (AFO) after the frame removal may have led to the contracture of the Gastrocnemius-Soleus muscles and shortening of the Achilles tendon. The patient has regained some length with stretching exercises. Bone grafting was needed to augment healing of delayed union of primary tibial fracture site after 4 months from the injury. This has united after 3 months of bone grafting and was helped by compression at the fracture site using the distal part of the Ilizarov frame.
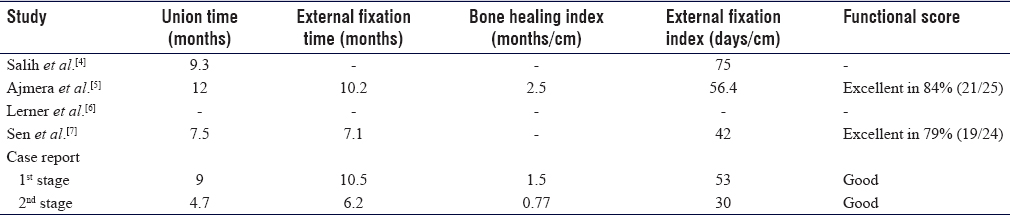
In comparison between the two stages of leg lengthening, we noticed that the second leg lengthening stage through the consolidated regenerate bone in the proximal tibia had a much shorter bone union and external fixator times and a lesser bone healing and external fixator indices than the first stage through the normal tibial bone.
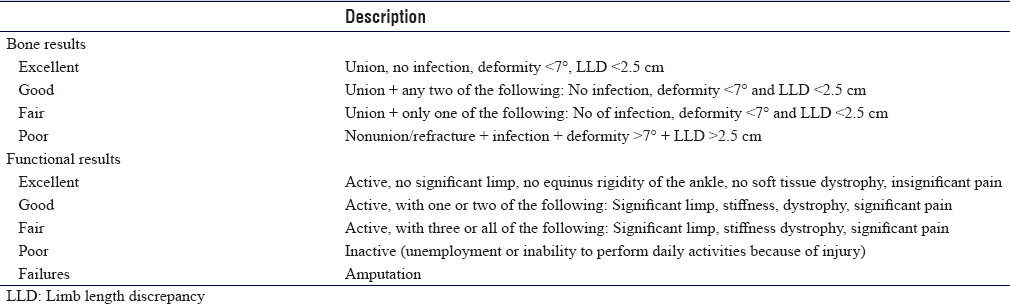
At 6 months follow up after the removal of all metalwork, the patient walks fully weight-bearing on a plantigrade foot with some compliance of dynamic AFO use. The passive range of movements of the knee joint was 5°–12° but actively was 10°–110°. The passive and active range of movements of the ankle joint was 0°–30° plantar flexion and no dorsiflexion [Figure - 8]a, [Figure - 8]b, [Figure - 8]c. A new leg length scanogram, obtained at this visit, showed a discrepancy in the growth of the legs and an LLD of 0.9 cm (Left tibia 0.4 cm shorter than right one). This is probably due to the unequal growth around the knees as the growth plates were affected by the original trauma. This is treated with a shoe raise. The bone and functional assessment were done according to the Association for the Study and Application of the Methods of Ilizarov (ASAMI) criteria reported by Paley et al.[10] and illustrated in [Table - 1]. The patient had an excellent bone result and a good functional result as he suffered from ankle stiffness and soft tissue dystrophy (impaired sensation of the foot, which could be due to the nerve injury at the time of the original trauma).
To our knowledge, there is no case reported in English literature that reports a 2nd stage leg lengthening of the tibia through the consolidated regenerate bone after a first-stage leg lengthening for the treatment of open tibial fracture with bone loss.
Literature Review
The aim of this systematic review is to find the answer to a proposed research question: what are the functional and bone healing outcomes after 1 year of treating open tibial fractures with bone loss by the method of acute shortening followed by leg lengthening using circular external fixator and distraction osteogenesis principles.
Methods and Results of the Review
PubMed search engine was used in our search as citations in PubMed come from MEDLINE indexed journals, journals/manuscripts deposited in PubMed Central, and National Center for Biotechnology Information Bookshelf. In addition, it's a free search engine that includes many journals and publications with occasional access to free articles that can make the search easy.
The literature search was performed on the 5th of September 2019 using the keywords “leg lengthening” and “circular frame” and “circular fixator” and “tibial fracture” and “Distraction Osteogenesis” in different combinations. This search revealed 60 articles after the exclusion of repeated articles in different combinations of the keywords. Another keyword, “multiple leg lengthening” was used alone and revealed 93 articles.
Inclusion criteria for the review
English studies on humans where the authors report the results of leg lengthening using a circular frame for early post traumatic treatment of lower leg after open tibial fractures were included.
Exclusion criteria
Studies that report leg lengthening using intramedullary nail or plates, the use of circular frame for nonunion, congenital deformities, cosmetic lengthening, reports complications, lengthening of bones other than the tibia.
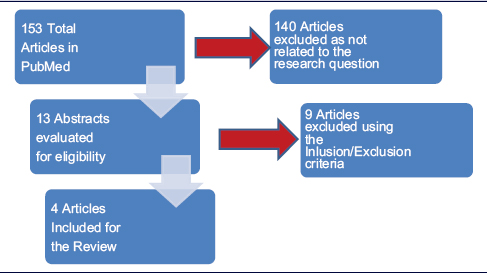
Going through the abstracts of these articles using the inclusion and exclusion criteria, only 13 articles were found related to the review subject.[[4],[5],[6],[7],[11],[12],[13],[14],[15],[16],[17],[18],[19]
On further reading and review of the abstracts, nine articles were excluded.[11],[12],[13],[14],[15],[16],[17],[18],[19] One article illustrating the complication of external fixator and comparing the use of the Ilizarov frame with and without intramedullary alignment was excluded. One article reported a case with a review of the literature, and two case report articles were excluded. One article comparing the different struts used in the Taylor Spatial Frame was excluded. Four articles reported limb lengthening for different reasons, including deformity correction, nonunion, postinfective, and different bones lengthening, were also excluded. The remaining four articles describing the results of acute shortening and leg lengthening of open tibial fracture were reviewed [Table - 2]: shows the flow chart of the inclusion and exclusion of the articles].
None of the studies found has reported multiple-stage leg lengthening of the tibial bone for the treatment of open tibial fracture with bone loss.
Discussion and Critical Appraisal of the Studies
The four studies were retrospective case series reports of the results of management of open tibial fractures with circular frames; level IV evidence on the hierarchy of evidence.[4],[5],[6],[7] These reports are useful in reporting the results of small samples size treated with an unusual method that requires special expertise, which is not available on a routine basis; i.e., the circular frame. Also, it is easier and takes less time to perform, as most of the data are available and only needs to be collected and analyzed. This type of studies is helpful in our practice as they might initiate a research question for future studies and can help in generating guidelines for the treatment of these cases, e.g., to treat all these cases in tertiary hospitals where all parts of a multidisciplinary team with special expertise are available.[2] It is a very useful study design in this cohort of patients where it is very difficult to find a comparator group and might be unethical to randomize patients with open tibial fractures and mangled legs to a different type of treatment. The limitation of retrospective case series is that it is a retrospective review of a group of patients, the absence of control group, missing data, the confounding factors, treatment and recall bias, and the generalizability of the results.[20]
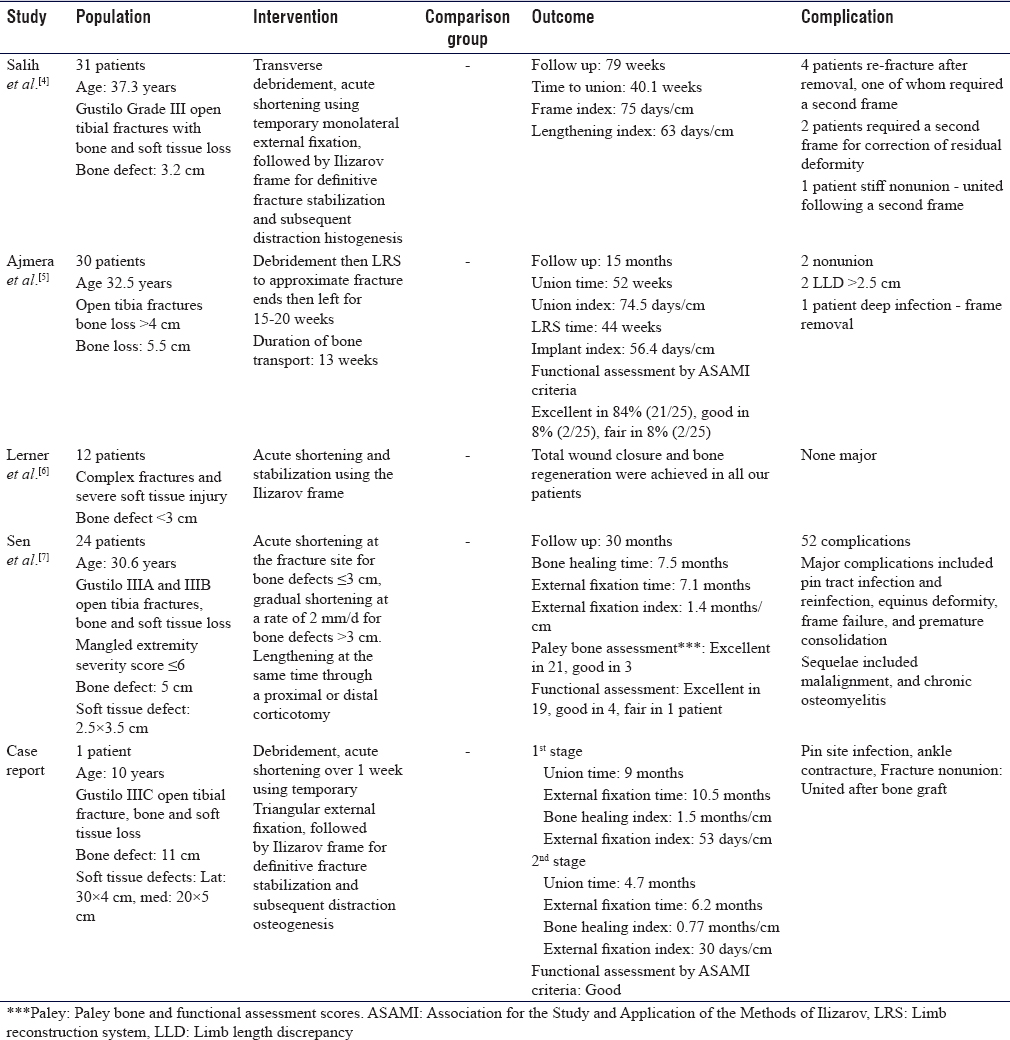
Authors of the four articles reported similar patients' populations; patients who sustained open tibial fractures with bone loss and extensive soft tissue damage. These patients in the four articles were all treated in a similar way; with surgical debridement of devitalized tissue and bone, followed by acute shortening and treatment with circular frame for lengthening of the short limb adopting the principle of distraction osteogenesis through normal tibial bone osteotomy.[4],[5],[6],[7] Although the mean bone defect was variable between the studies, authors performed acute shortening at the fractured sites after thorough debridement. Salih et al.[4] performed surgical debridement using a transverse elliptical incision across the tibial crest. They reported that the transverse incision could often be primarily closed or gives access to surrounding muscles to cover the bone with a muscle flap. Ajmera et al.[5] reported his patients that were treated by the limb reconstruction system (LRS), which is a type of dynamic external fixator and adopted the distraction osteogenesis principles of normal bone. Sen et al.[7] reported performing simultaneous gradual shortening for bone defect more than 3 cm and lengthening through the osteotomy site. [Table - 3] shows the summary of the four articles included in this review; the population, intervention, comparator, and outcome measure in addition to the results of our case report.
In our case, after thorough debridement, acute shortening was performed in two stages according to the soft tissue demand to allow the soft tissue management. A temporary joint-bridging triangular external fixator[9] was used to stabilize the fractured tibia and allows soft tissue management. The bone defect was approximately 11 cm. The temporary external fixator was replaced by an Ilizarov circular frame on day 35 after the injury after soft tissue healing was achieved by a split skin graft over the anteromedial and posterior aspect of the lower leg to cover the area of skin loss left after shortening of the leg and consecutive debridement of devitalized tissue.
A two-stage lengthening was adopted in our case. The first stage was performed through an osteotomy of a healthy bone of proximal tibia, then the frame was removed, and physical therapy started. The 2nd stage was performed through an osteotomy of the regenerated bone of proximal tibia, which, to our knowledge, was not described in English literature. This two-stage lengthening method has allowed the patient a convalescence period of physical therapy to improve the joints function and range of motion of the knee and ankle joints. In addition, this method was adopted as a precaution to keep the lengthening to the minimum that can be achieved at the first stage to avoid further neurovascular compromise. Also, it was difficult to predict the amount of leg growth and LLD as the child was growing and approaching the age of growth spurt and taking into consideration that the growth plates around the knee were affected by the original trauma. Also, this approach had a psychological effect on the patient as he was enthusiastic about starting the 2nd stage after seeing the result of the first lengthening.
The outcome measures reported in the four studies were variable. There were different times and indices reported, which looks like synonyms to the same measurements. Distraction time is the time of the distraction at the osteotomy site to achieve the required length. The distraction at the osteotomy site is usually started at a rate of 1 mm/day. The consolidation time is the time form the end of distraction to the bony union, which allows the frame to be removed and is usually more than double the distraction time. The consolidation index is the consolidation time per distraction gap in centimeters.[21],[22] These parameters have been explained in some of the four studies but in different nomenclatures. The healing index is a widely used parameter for the lengthening of bones and expressed as the distraction–consolidation time (time to bony union) per centimeters of lengthening. It is usually 1 month/cm in children and 2–3 months/cm in adults.[21],[22] The external fixator index is the time of the external fixator on the bone in days per centimeter of length gained, which is reported as an average of 57 days/cm.[21]
The distraction of bone has a detrimental effect on the adjacent structures. Muscular stretching can lead to plastic deformation and contracture around the joints with a limitation of range of movement. Nerves and vessels can suffer from degenerative changes, and excessive distraction can lead to partial or complete nerve potentials loss.[21] These effects have been mentioned as complications or sequels of the leg lengthening in the four studies, and it also happened in our case.
Results of the Studies
The outcome measures reported in the four studies were variable. There were different times and indices reported, which looks like synonyms to the same measurement as explained earlier in our critical appraisal of the studies. [Table - 3] illustrates the results of these studies as reported by the authors and the case report two stages. [Table - 4] shows the results with adjustment of units of measurement for comparison purposes.
Salih et al.[4] reported the median of time to union, frame index, and lengthening index. The frame index was defined as days in frame per bone loss, whereas the lengthening index was days in the frame after corticotomy per bone loss. These indices were identified as times per the amount of bone loss in centimeters, whereas the external fixator index and the healing index were identified as times per the amount of length gained in centimeters.[21],[22] These two parameters; bone loss and the length gained; should be equal at the end of the treatment, which make these indices synonyms.
Ajmera et al.[5] reported the mean of union time, the union index, and the implant index. These indices were not identified by the authors, but they reported time in days per centimeters. They also reported a functional assessment score by the ASAMI criteria. Reporting the results with a known score is one of the strengths of this study although that does not mean the score has been validated.[10],[23]
Lerner et al.[6] reported the achievement of total wound closure and bone regeneration. Sen et al.[7] reported the mean bone healing time, the mean external fixator time, and the index. In addition, they reported the Paley bone and functional assessment scores, a score reported by Paley et al.[23] to assess the bone alignment and union in addition to the functional assessment criteria.
In our case, we reported the bone union time, external fixator time, bone healing index, and eternal fixator index for the two stages of distraction osteogenesis. We also reported the functional assessment score by ASAMI criteria [Table - 4]. We noticed that the second leg lengthening stage through the consolidated regenerate bone in proximal tibia had a much shorter bone union and external fixator times and a lesser bone healing and external fixator indices than the first stage through the normal tibial bone. A possible explanation for this observation could be probably due to the fact that the patient underwent a vascular bypass around the knee due to vascular injury of the popliteal artery, which could have caused a slower healing process in the proximal tibia due to reduced blood supply to the area. Moreover, the hypervascularity state of the regenerate proximal tibial bone could have contributed to the faster healing of the second osteotomy period.[21]
To our knowledge, there are no cases reported in English literature that reports a 2nd stage leg lengthening of the tibia through the consolidated regenerate bone after a first-stage leg lengthening of normal bone for the treatment of open tibial fracture with bone loss.
Conclusions of the Studies
The four studies reviewed concluded that surgical debridement; acute shortening followed by distraction osteogenesis is a safe and acceptable method of treatment of open tibial fractures with extensive soft tissue damage and bone loss. The acute shortening of the tibia can help fracture site union aided by compression using the circular frame and helps the soft tissue coverage and healing with simple split-skin grafts rather than the need for complex transfer flaps.[4],[5],[6],[7] Salih et al.[4] recommended transverse wound debridement in selected cases to allow early soft tissue coverage. Ajmera et al.[5] had a similar conclusion using their LRS fixator but recommended further studies to prove its efficiency. Sen et al.[7] recommended the use of bifocal compression-distraction osteogenesis for the treatment of these cases.
We adopted the method of surgical debridement, acute shortening followed by distraction osteogenesis for the treatment of our reported case, and surely have provided the patient with a good result and final outcome.
Conclusion
Surgical debridement, acute shortening followed by leg lengthening through an osteotomy using a circular frame, is an acceptable treatment method of extensive open tibia fractures with bone loss. The evidence in the literature is level IV. A 2nd stage leg lengthening can be performed in the consolidated regenerate bone of the tibia, as reported in our case.
Recommendations
RCT is very difficult to perform on such complex fractures, as these cases are very difficult to randomize to different groups of treatment, and it might be unethical to perform such a study. Further level III retrospective comparative study can be recommended to perform as a multicenter study where enough number of cases are found and can be compared to patients who were treated with different methods.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient's parents have given their consent for his images and other clinical information to be reported in the journal. The patient's parents understand that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
ADAS conceived and designed the study, collected and organized data and wrote the case report. SDS conducted the literature search, analyzed and interpreted data and wrote the initial and final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br 2005;87:142-50. [Google Scholar] |
| 2. | Nanchahal J, Nayagam D, Khan U, Moran C, Barrett S, Sanderson F, et al. The Standards for the Management of Open Fractures of the Lower Limb. 1st ed. London: Royal Society of Medicine Press Ltd.; 2009. Available from: http://www.bapras.org.uk/docs/default-source/commissioning-and-policy/standards-for-lower-limb.pdf. [Last accessed on 2019 Oct 02]. [Google Scholar] |
| 3. | Trickett RW, Rahman S, Page P, Pallister I. From guidelines to standards of care for open tibial fractures. Ann R Coll Surg Engl 2015;97:469-75. [Google Scholar] |
| 4. | Salih S, Mills E, McGregor-Riley J, Dennison M, Royston S. Transverse debridement and acute shortening followed by distraction histogenesis in the treatment of open tibial fractures with bone and soft tissue loss. Strategies Trauma Limb Reconstr 2018;13:129-35. [Google Scholar] |
| 5. | Ajmera A, Verma A, Agrawal M, Jain S, Mukherjee A. Outcome of limb reconstruction system in open tibial diaphyseal fractures. Indian J Orthop 2015;49:429-35. [Google Scholar] |
| 6. | Lerner A, Fodor L, Soudry M, Peled IJ, Herer D, Ullmann Y. Acute shortening: Modular treatment modality for severe combined bone and soft tissue loss of the extremities. J Trauma 2004;57:603-8. [Google Scholar] |
| 7. | Sen C, Kocaoglu M, Eralp L, Gulsen M, Cinar M. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss: A report of 24 cases. J Orthop Trauma 2004;18:150-7. [Google Scholar] |
| 8. | Fracture and dislocation classification compendium – 2018. AO Pediatric Comprehensive Classification of Long Bone Fractures (PCCF). Orthop Trauma 2018; 32 Suppl 1:S117-40. Available from: https://www2.aofoundation.org/AOFileServerSurgery/MyPortalFiles?FilePath=/Surgery/en/_docs/AOOTA%20Classification%20Compendium%202018.pdf. [Last accessed on 2020 Jan 08]. [Google Scholar] |
| 9. | Hessmann M, Nork S, Sommer C, Twaddle B. Reduction and Fixation of Distal Tibia Extraarticular Multifragmentary Fracture – Triangular External Fixator. AO foundation Surgery Reference (Online reference in clinical life). V2.0; 2018. Available from: https://www2.aofoundation.org/wps/portal/surgery?bone=Tibia &segment=Distal&classification=43-Extraarticular,%20multifragmentary&showPage=indication. [Last accessed on 2019 Oct 17]. [Google Scholar] |
| 10. | Paley D, Catagni MA, Argnani F, Villa A, Benedetti GB, Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res 1989;241:146-65. [Google Scholar] |
| 11. | Bukva B, Vrgoč G, Rakovac I, Dučić S, Sindik J, Čoklo M, et al. Complications in leg lengthening using an Ilizarov external fixator and intramedullary alignment in children: Comparative study during a fourteen-year period. Injury 2015;46 Suppl 6:S48-51. [Google Scholar] |
| 12. | Fletcher MD, Solomin LN. Definitive management of significant soft tissue loss associated with open diaphyseal fractures utilising circular external fixation without free tissue transfer, a comprehensive review of the literature and illustrative case. Eur J Orthop Surg Traumatol 2015;25:65-75. [Google Scholar] |
| 13. | Gulabi D, Erdem M, Cecen GS, Avci CC, Saglam N, Saglam F. Ilizarov fixator combined with an intramedullary nail for tibial nonunions with bone loss: Is it effective? Clin Orthop Relat Res 2014;472:3892-901. [Google Scholar] |
| 14. | Sala F, Talamonti T, Agus MA. Tetrafocal leg reconstruction using combined Ilizarov/TSF technique. Musculoskelet Surg 2011;95:151-5. [Google Scholar] |
| 15. | Iobst C. Limb lengthening combined with deformity correction in children with the Taylor Spatial Frame. J Pediatr Orthop B 2010;19:529-34. [Google Scholar] |
| 16. | Blondel B, Launay F, Glard Y, Jacopin S, Jouve J, Bollini G. Limb lengthening and deformity correction in children using hexapodal external fixation: Preliminary results for 36 cases. Orthop Traumatol Surg Res 2009;95:425-30. [Google Scholar] |
| 17. | Lerner A, Fodor L, Stein H, Soudry M, Peled IJ, Ullmann Y. Extreme bone lengthening using distraction osteogenesis after trauma: A case report. J Orthop Trauma 2005;19:420-4. [Google Scholar] |
| 18. | Märtson A, Haviko T. Posttraumatic limb shortening: Treatment with the Ilizarov distraction device. Ann Chir Gynaecol 2000;89:303-7. [Google Scholar] |
| 19. | Maffulli N, Lombari C, Matarazzo L, Nele U, Pagnotta G, Fixsen JA. A review of 240 patients undergoing distraction osteogenesis for congenital post-traumatic or postinfective lower limb length discrepancy. J Am Coll Surg 1996;182:394-402. [Google Scholar] |
| 20. | Petrisor B, Bhandari M. The hierarchy of evidence: Levels and grades of recommendation. Indian J Orthop 2007;41:11-5. [Google Scholar] |
| 21. | Hasler CC, Krieg AH. Current concepts of leg lengthening. J Child Orthop 2012;6:89-104. [Google Scholar] |
| 22. | Emara KM, Ghafar KA, Al Kersh MA. Methods to shorten the duration of an external fixator in the management of tibial infections. World J Orthop 2011;2:85-92. [Google Scholar] |
| 23. | Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-65. [Google Scholar] |
Fulltext Views
4,510
PDF downloads
1,750





