Translate this page into:
Utility outcomes score assessment of living with below-knee amputation
-
Received: ,
Accepted: ,
How to cite this article: Makhdom A, Cota A. Utility outcomes score assessment of living with below-knee amputation. J Musculoskelet Surg Res 2022;6:138-43.
Abstract
Objectives:
Lower limb trauma that involves severe soft-tissue injuries continues to pose treatment challenges when considering whether to perform an amputation or salvage the injured extremity. This study aimed to measure the perceived health burden of living with unilateral below-knee amputation (BKA). A secondary aim was to compare the health burden of living with BKA and single-eye blindness and/or double-eye blindness (SEB and DEB).
Methods:
A web-based survey was utilized to establish the effectiveness of outcome scores for three health states (unilateral BKA, SEB, and DEB) in a sample of 116 participants recruited from the general population. The outcome measures included the time trade-off (TTO), standard gamble (SG), and visual analog scale (VAS) tests.
Results:
The TTO, SG, and VAS scores for BKA were 0.75 ± 0.2, 0.78 ± 0.18, and 0.57 ± 0.16, respectively. These measures indicate that participants were willing to undergo a theoretical surgery that carries a 22% chance of mortality and trade 9 years of life to avoid a BKA. These were lower than the values of SEB VAS (P = 0.02) and TTO (P = 0.002) tests and the SG measure (0.8 ± 0.17, P = 0.09). Age, gender, race, income, and education were not statistically significant independent predictors of the utility scores for BKA.
Conclusion:
When faced with a BKA, individuals in our sample population would choose to undergo reconstructive surgery with a hypothetical 22% chance of mortality. They would be willing to sacrifice 9 years of their life for such a surgery to avoid a BKA. These data can be beneficial to understand better how patients perceive their disability and help in patients’ counseling.
Keywords
Below-knee amputation
Utility outcome scores
Quality of life
Prosthetic treatment
Outcome measures
INTRODUCTION
Significant lower extremity trauma is an entity frequently encountered by orthopedic trauma surgeons. While the incidence of open long bone fractures in some reports is 12 per 100,000 persons annually, 40% of all complex traumas occur in the lower limb and these tend to be more severe than open fractures in the upper extremities.[1,2] Complex open lower extremity trauma is often associated with extensive muscle and neurovascular damage. This injury pattern continues to pose a treatment challenge when deciding between a treatment course involving limb salvage or surgical amputation.[3,4] Over the past few decades, many studies have highlighted the clinical differences and consequences between these two options for patients. However, neither treatment option has proven superior with respect to long-term functional outcomes.[3-8] While there are some clearly defined indications where limb amputation is preferred over surgical reconstruction, the decision regarding the optimal treatment strategy is often a difficult one to make. The resulting loss of a limb can negatively affect a patient’s life as well as psychosocial well-being.[7] Objectively quantifying the perceived impact of the health burden of a lower extremity amputation offers help when counseling patients facing a decision between below-knee amputation (BKA) and limb-salvage surgery and is also important for insurance funding and health-care resource distribution. One means of objectively measuring a particular health state is through the use of validated utility outcome scores. Examples of such validated measures include the standard gamble (SG – that is, the mortality risk an individual would accept to obtain perfect health), the visual analog scale (VAS – scores range from 0 [death] to 1 [healthy]), and time trade-off (TTO – that determines the number of years of life an individual would relinquish to be perfectly healthy).[9-11] Outcome utility tools have helped provide a rationale for developing a standard of care models for many medical conditions.[12] Of these, preference-based measures are invaluable to allow for objective standardization of an individual’s health status. Utility scores are validated preference-based measures that were primarily established in the 1980s to determine health state preferences in health economics and epidemiological medicine.[9,13,14] This concept was then introduced in the plastic surgery literature and helped objectively measure the health burden of many disfiguring conditions.[12,15] Recently, utility assessments have been utilized in the orthopedic literature as well.[16-18]
Our primary aim in this study was to objectively measure the perceived health impact on an individual living with a unilateral BKA using utility outcome scores (TTO, SG, and VAS) in a sample from the general population. The secondary aims were to compare the perceived health state outcome scores for living with a BKA to those for single-eye and double-eye blindness (SEB and DEB) and to determine whether the utility scores for a unilateral BKA were influenced by age, gender, race, income, and education.
MATERIALS AND METHODS
Open enrollment online classified ads were posted and hosted by McGill University in Canada to recruit a sample of volunteers from the general population over 6 months. All subjects signed an electronic consent form before commencing a web-based survey, which collected anonymous demographic information in addition to providing questionnaires designed to determine the TTO, SG, and VAS utility scores for unilateral BKA, SEB, and DEB. Our survey used three different utility tools (the TTO, SG, and VAS) to account for any potential weaknesses associated with a single tool.
Based on expert opinion, descriptive health state scenarios describing the potential limitations for an individual living with one of the three health states (SEB, DEB, or a unilateral BKA) were created. The amputation scenario included a clinical photograph of a patient with a unilateral BKA [Figure 1]. Subjects’ comprehension of the study objectives was initially assessed by asking participants to rate the perceived health impact of SEB and DEB using the TTO, SG, and VAS utility outcome measures. Individuals who gave DEB a higher utility score (indicating a health state closer to perfect health) than SEB were excluded from the study. A schematic of the website survey is illustrated in Figure 2. To decrease the occurrence of multiple entries, our inclusion for participation required a valid e-mail address. All three of the utility outcome tools were used for each of the three health states in the same fashion. The following is an example of how the assessments were structured for the unilateral BKA scenario.

- Photo of a patient with below-knee amputation that was shared with our clinical scenario.
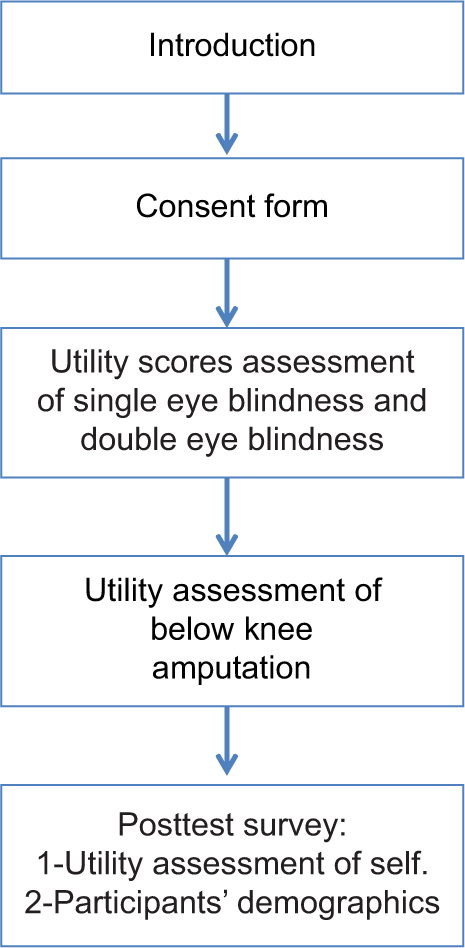
- The scheme of the online survey. The volunteers were first presented with a general description of the study and then presented with an online consent form to read and sign electronically. The survey was continued only if the participants agreed to the terms and conditions found in the consent form and signed it electronically. The study then continued with the online clinical scenarios to determine the utility scores. The study was completed with a post-test survey.
The VAS assessment asked surveyors to imagine themselves as the person with a unilateral BKA in the provided scenario and then provides a value ranging from 0 (death) to 100 (perfect health), rating the perceived health impact of this outcome. The utility health state score for unilateral BKA was determined by taking each participant’s rating (from 0 to 100) and dividing it by 100.
The TTO was assessed by asking the study participants to imagine themselves as the person with the unilateral BKA in the scenario. Participants were then asked to decide between living for the next 36 years of their life like the patient in the scenario and receiving a theoretical treatment that would guarantee them perfect health for 35 years but would require them to sacrifice 1 year of their life. If patients were unwilling to trade any years of life for perfect health, they scored 0 for this test. However, if an individual was willing to accept the loss of 1 year of life, up to six iterations of a sequentially alternating bisecting algorithm were used to determine an indifference point, which would represent the maximum amount of life years an individual would trade-off to have perfect health and avoid a BKA. For example, if a participant was willing to accept a loss of 1 year of life, they would then be asked if they would accept of loss of 17.5 (i.e., 35/2) life years for perfect health. If they dropped this option, they would be presented with an offer to lose 8.75 years of life (i.e., 17.5/2) for perfect health. This would continue for six iterations until the individual reached an acceptable trade-off in terms of life-years sacrificed for perfect health (no BKA) or declined all further increases in life lost and was left with the initial 1-year sacrifice that they agreed to. The utility score was determined using the following formula: TTO = (number of years living with a BKA – number of years traded off at the indifference point)/number of years living with a BKA.
Regarding the SG utility score, surveyors were asked to select one of two options – to either remain in a current given health state (unilateral BKA) or take a chance on therapeutic management with some probability of success (perfect health) and some probability of failure (death). This gamble was initially presented to the participants, offering them a 99% chance of perfect health with a 1% chance of death. Patients that declined this option ended the gamble test. However, if individuals were willing to accept these risk/benefit parameters, they were offered treatments with increasing percent chances of death. Once a participant reached a level of risk whereby, they would not consider the treatment to avoid a BKA, the bisecting algorithm was again used to provide a decreasing chance of death associated with the treatment until an indifference point was reached whereby the participant was willing to accept the gamble (chance of death) to avoid the BKA health state. The SG utility score was determined using the following formula: Utility score = (1.00 –the risk of death at the point of indifference)/100. The online survey was concluded by asking the volunteers to rate their current health state using the TTO measure. The goal of performing a self TTO is to evaluate the current health state of the surveyors. Again, they were presented with the option of living in their current health state for 36 years or receiving a treatment, which would guarantee them perfect health but at the cost of 1 year of life. The algorithm was then executed in the same manner as previously described. Finally, we have utilized the STROCCS guidelines to help strengthen reporting this study.[19]
Statistical analysis
Paired t-test was used to compare the mean values for the utility scores. In addition, linear regression analysis was utilized to assess whether age, gender, race, income, and education were independent predictors for the utility scores. Statistical significance was set at P < 0.05. SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) was used to perform these calculations.
RESULTS
The survey was completed by 132 prospective subjects. Sixteen were excluded, either because they rated the SEB test with a lower utility score than the DEB test or they did not complete the survey. The remaining 116 volunteers were included in the statistical analysis. The basic demographic information is demonstrated in Table 1.
| Mean age (years) | 24±5 |
| Gender | |
| Females | 62 |
| Males | 51 |
| Not reported | 3 |
| Race | |
| African-American | 3 |
| Asian | 24 |
| Caucasian | 54 |
| Hispanic | 1 |
| Other | 12 |
| Prefer not to answer | 22 |
| Education | |
| Some college | 9 |
| College graduate | 41 |
| Graduate or professional degree | 37 |
| Medical education | 6 |
| High school | 7 |
| Prefer not to answer | 16 |
| Income | |
| <$10,000 | 47 |
| $10,000–25,000 | 26 |
| $25,000–50,000 | 4 |
| $50,000–100,000 | 1 |
| >$100,000 | 1 |
| Prefer not to answer | 37 |
The TTO, SG, and VAS scores for a unilateral BKA were 0.75 ± 0.2, 0.78 ± 0.18, and 0.57 ± 0.16, respectively. These were significantly higher (P < 0.0001) than the corresponding scores for DEB (TTO = 0.57 ± 0.26, SG = 0.58 ± 0.24, and VAS = 0.31 ± 0.17). In addition, the utility measures for a unilateral BKA were significantly lower than the SEB TTO (0.79 ± 0.19, P = 0.002) and VAS (0.61 ± 0.16, P = 0.02) tests, but not for the SG measure (0.8 ± 0.17, P = 0.09). The self-rated TTO (0.92 ± 0.16) was significantly higher (P < 0.0001) when compared with the BKA TTO utility score (0.75 ± 0.2). The results of utility scores are summarized in Table 2.
| Utility scores | ||||||
|---|---|---|---|---|---|---|
| Test | SEB | DEB | Below-knee amputation | P-value (SEB vs. BKA) | P-value (DEB vs. BKA) | Self |
| VAS | 0.61±0.16 | 0.31±0.17 | 0.57±0.16 | 0.02 | <0.0001 | |
| TTO | 0.79±0.19 | 0.57±0.26 | 0.75±0.2 | 0.002 | <0.0001 | 0.92±0.16 |
| SG | 0.8±0.17 | 0.58±0.24 | 0.78±0.18 | 0.09 | <0.0001 | |
VAS: Visual analog scale, TTO: Time trade-off, SG: Standard gamble, SEB: Single-eye blindness, DEB: Double-eye blindness, BKA: Below-knee amputation
The unilateral BKA scores for the TTO (0.75 ± 0.2) and SG (0.78 ± 0.18) utility measures indicate that patients were willing to undergo a theoretical procedure with a 22% chance of mortality and trade 9 years of life to avoid a BKA. Regression analysis revealed that age, gender, race, income, and education were not statistically significant independent predictors of the utility scores for unilateral BKA.
DISCUSSION
Our results objectively measure the perceived impact that a unilateral BKA can have on an individual (TTO 0.75 ± 0.2, SG 0.78 ± 0.18, and VAS 0.57 ± 0.16). These BKA scores were significantly higher than scores for DEB (TTO 0.57 ± 0.26, SG 0.58 ± 0.24, and VAS 0.31 ± 0.17), indicating that participants in the study felt that complete blindness had a more significant impact on an individual’s health-related quality of life than a unilateral BKA. Conversely, the TTO scores (0.79 ± 0.19) and VAS (0.61 ± 0.16) for SEB were significantly higher than the BKA scores indicating that the participants in the study perceived a unilateral BKA to have a more detrimental impact on a person’s health status than being blind in one eye.
In addition, the previous studies that have examined the health burden of various disease states indicate that living with a unilateral BKA (TTO 0.75) is comparable with living with bilateral mastectomy defects (TTO 0.70),[20] living with severe facial disfigurement (TTO 0.68),[21] Type 1 diabetes mellitus (TTO 0.67),[22] and patients with Stage-4 renal disease after renal transplantation (TTO 0.78).[23] Moreover, these types of interdisciplinary comparisons have the potential to influence healthcare resource allocation by allowing for a measurement of the perceived health burden of a particular disease state.
Traumatic injuries are the second most common cause of amputations after dysvascular etiologies. Although patients prefer limb reconstruction at the time of injury, studies have suggested that the majority of failed limb reconstruction patients would pursue early amputation if they were able to repeat their decision.[8,24] Although limb reconstruction is often an alternative to amputation, it is not without its own set of drawbacks. A recent review reported that the length and cost of rehabilitation are higher for limb-salvage procedures and require more frequent reoperations and rehospitalizations.[8] Moreover, there appears to be no long-term functional benefit to limb reconstruction with high rates of disability and pain reported for both limb-salvage and amputation patients.[8] Given that participants in our study would be willing to undergo a procedure with a 22% chance of mortality and sacrifice 9 years of life to avoid a BKA, it is possible that patients have unrealistic expectations regarding the outcomes of limb salvage and may choose this route because of the perceived health impact of a BKA. Our results highlight the importance of counseling patients regarding the risks, expected functional outcomes, discussing realistic expectations, and offering psychosocial support when choosing between amputation and limb-salvage surgery.
Limitations of this study include using a sample of relatively healthy participants as evidenced by the high self-rated TTO (0.92 ± 0.16). Although there are advantages to extracting utility scores from patients themselves to reflect the actual health burden, previous research has suggested that most patients become habituated to their health condition and experience a decreased health burden over time.[25]
Moreover, it is difficult to design a study that can effectively obtain utility scores from a representative number of patients afflicted with uncommon health conditions at a specific time point. Consequently, extracting the utility scores from a general population sample is optimal and cost-effective in such cases.[26,27] In addition, despite our large sample size, selection bias may exist in the study participants as they were predominantly younger (mean age 24 ± 5) with higher education levels.
CONCLUSION
We have demonstrated that the utility outcome scores for living with a unilateral BKA are lower than for SEB but higher than DEB. In addition, the objective TTO (0.75 ± 0.2), SG (0.78 ± 0.18), and VAS (0.57 ± 0.16) scores for a unilateral BKA will allow future comparisons to be made between other orthopedic conditions. These types of analyses provide a better understanding of how patients perceive their potential disability and can provide insight when making decisions regarding healthcare allocation and funding resources.
AUTHORS CONTRIBUTIONS
Both authors have contributed in study design, concept, critical anaylsis, writing the 1st draft and reveiwing the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study received Institutional Research Board ethics approval. Number: 15881 on 02-21-2013, from the Research ethics board at McGill university health center, Montreal, Canada.
ACKNOWLEDGMENT
This study was presented as a podium presentation and in part as a conference proceeding in “Proceedings of ILLRS congress Miami 2015 combined meeting of ILLRS LLRS and ASAMI-BR”.
We would like to thank Dr. Hani Sinno for his contribution to this study’s concept and design.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate participants consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicts of interest.
References
- Epidemiology and management of open fractures of the lower limb. Br J Hosp Med. 1997;57:582-7.
- [Google Scholar]
- Factors influencing outcome following limb-threatening lower limb trauma: Lessons learned from the lower extremity assessment project (LEAP) J Am Acad Orthop Surg. 2006;14:S205-10.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of outcomes and complications of reconstruction and amputation for Type IIIB and IIIC fractures of the tibia. Plast Reconstr Surg. 2008;122:1796-805.
- [CrossRef] [PubMed] [Google Scholar]
- An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347:1924-31.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg Am. 2004;86:1636-45.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg Amys. 2005;87:1801-9.
- [CrossRef] [PubMed] [Google Scholar]
- Complex limb salvage or early amputation for severe lower-limb injury: A meta-analysis of observational studies. J Orthop Trauma. 2007;21:70-6.
- [CrossRef] [PubMed] [Google Scholar]
- Preferences for health outcomes. Comparison of assessment methods. Med Decis Making. 1984;4:315-29.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring health state preferences in women with breast hypertrophy. Plast Reconstr Surg. 2000;106:280-8.
- [CrossRef] [PubMed] [Google Scholar]
- Utility outcome assessment of the aging neck following massive weight loss. Otolaryngol Head Neck Surg. 2012;147:26-32.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of outcome studies in plastic surgery. Plast Reconstr Surg Glob Open. 2014;2:e189.
- [CrossRef] [PubMed] [Google Scholar]
- Methodology for measuring health-state preferences-II: Scaling methods. J Clin Epidemiol. 1989;42:459-71.
- [CrossRef] [Google Scholar]
- Describing health states. Methodologic issues in obtaining values for health states. Med Care. 1984;22:543-52.
- [CrossRef] [PubMed] [Google Scholar]
- The health burden of breast hypertrophy. Plast Reconstr Surg. 2001;108:1591-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral hallux valgus: A utility outcome score assessment. J Foot Ankle Surg. 2016;55:944-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of living with scoliosis: A utility outcome score assessment. Spine (Phila Pa 1976). 2017;42:E93-7.
- [CrossRef] [PubMed] [Google Scholar]
- Utility outcome assessment of pes planus deformity. Foot Ankle Surg. 2018;24:119-23.
- [CrossRef] [PubMed] [Google Scholar]
- STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg. 2021;96:106165.
- [CrossRef] [PubMed] [Google Scholar]
- An objective assessment of the perceived quality of life of living with bilateral mastectomy defect. Breast. 2013;22:168-72.
- [CrossRef] [PubMed] [Google Scholar]
- Utility scores for facial disfigurement requiring facial transplantation. Plast Reconstr Surg. 2010;126:443-9.
- [CrossRef] [PubMed] [Google Scholar]
- Valuing health-related quality of life in diabetes. Diabetes Care. 2002;25:2238-43.
- [CrossRef] [PubMed] [Google Scholar]
- Preference-based quality of life of patients on renal replacement therapy: A systematic review and meta-analysis. Value Health. 2008;11:733-41.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of limb loss. Phys Med Rehabil Clin N Am. 2014;25:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of risk acceptance in facial transplantation. Plast Reconstr Surg2006;. ;118:663-70.
- [CrossRef] [PubMed] [Google Scholar]
- Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296:716-21.
- [CrossRef] [PubMed] [Google Scholar]
- Recommendations for reporting cost-effectiveness analyses. Panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1339-41.
- [CrossRef] [PubMed] [Google Scholar]






