Translate this page into:
Incidence and predictors of surgical site infections following foot and ankle surgery
2 College of Medicine, Almaarefa Colleges for Science and Technology, Riyadh, Saudi Arabia
3 College of Medicine, King Faisal University, Al-Hasa, Saudi Arabia
4 College of Medicine, Jazan University, Jazan, Saudi Arabia
5 Department of Orthopedics, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
Corresponding Author:
Omar A Al-Mohrej
Department of Orthopedics, King Faisal Specialist Hospital and Research Center, Riyadh
Saudi Arabia
mohrejo@gmail.com
| How to cite this article: Al-Kenani NS, Alsultan AS, Alosfoor MA, Bahkali MI, Al-Mohrej OA. Incidence and predictors of surgical site infections following foot and ankle surgery. J Musculoskelet Surg Res 2017;1:6-9 |
Abstract
Objectives: Surgical site infections (SSIs) have a significant impact on morbidity, mortality, and health-care expenditures. Therefore, the aims of the current study were to examine the incidence of SSI among patients who had foot and ankle surgery at large hospital in Riyadh and to identify predictors of SSIs. Methods: This is a retrospective cohort study. This is a consecutive study of patients underwent foot and ankle surgery between 2010 and 2014. The association between variables and infection status was analyzed using a logistic regression model. Results: The study included 295 patients. The incidence of SSI was 3.42%. The age and the type of surgery were significant predictors of SSI. Conclusions: Proper postoperative monitoring for high-risk patients may facilitate reduction of SSIs following foot and ankle surgery and improves health outcomes.Introduction
Surgical site infection (SSI) is defined as a wound contamination by microorganisms within 30 days following a surgery, or within 1 year if implanted object is placed, or if it is deep infection or organ space infection such as osteomyelitis.[1],[2],[3],[4] Among other factors, surgical wounds are exposed to numerous complications. The most common of them is infection, comprising between 46% and 58.7% of all surgical complications.[5],[6] In the United States, it has been reported that SSIs are the most common type of hospital-acquired infections.[7],[8]
SSIs have a significant impact on morbidity, mortality, health-care cost, and even hospital length of stay.[8],[9] There are about a half million cases of SSIs in the United States every year, and the mortality is directly linked to SSI in 77%.[7],[10],[11] Moreover, SSIs were found to be associated with as much as $1.6 billion excess in costs and with an increase of hospitalizations by nearly 1 million additional days.[12] Moreover, SSIs are associated with greater physical limitations leading to reduced quality of life.[13]
Previous studies have identified several factors that increase the risk of SSI, including prolonged surgery time more than the 75th percentile, complicated diabetes, peripheral neuropathy, smoking status, Charcot neuropathy, and obesity.[1],[3],[4],[11],[14],[15] The urgency of the surgery may have an impact on postoperative SSI. Emergency surgeries were found to have a higher rate of SSI than elective surgeries, which could be due to the severity of the surgical injury and soft tissue damage or having a prolonged surgery time.[11] Certain surgical techniques were associated with an increased risk of SSIs, for example, using bone graft or no drainage use.[6]
Risk factors for SSIs in previous studies are mostly based on patient populations with diverse orthopedic conditions. Therefore, it is unknown whether the incidence and risk factors of foot and ankle SSIs are similar to those of other conditions. After all, the field of foot and ankle surgery has a higher rate of SSIs than other elective orthopedic procedures.[16] This area of research is still developing in Saudi Arabia, and there are no studies that examined the incidence and risk factors of SSIs following foot and ankle procedures. Therefore, the aims of the current study were to examine the incidence of SSI among patients who had foot and ankle surgery at large hospital in Riyadh and to identify predictors of SSIs. Examining predictors of SSI is important to improve the quality of wound care because early identification of these patients may facilitate a positive impact on patients' postoperative care and improve health outcomes.
Materials and Methods
This is a retrospective study, which included all patients who had foot and ankle surgery between 2010 and 2014 at King Abdulaziz Medical City (KAMC) in Riyadh, Saudi Arabia. This hospital is one of the largest hospitals in Riyadh with a bed capacity of 1501.
There were 295 patients included in the study using convenience sampling who had 353 surgeries.[17] In this sampling method, data were collected from medical charts of all surgeries performed by a single surgeon (principle investigator).
In this study, several variables were collected including: patients' demographics (i.e., age, gender, body mass index and smoking status), laboratory investigations (i.e., per-operative glucose level and white blood cell count), and surgery related data (i.e., surgery technique, duration of surgery, length of hospital stay, and complications). According to previous literature, SSIs were associated with other comorbidities, such as diabetes mellitus, hypertension, peripheral neuropathy, peripheral vascular disease, and rheumatoid arthritis. Medications used preoperatively were also investigated (i.e., tumor necrosis factor alpha, steroids, and nonsteroidal anti-inflammatory drugs). Hence, these variables were studied. Furthermore, the National Nosocomial Infection Surveillance (NNIS) score was examined as a potential risk factor.[18] The NNIS was calculated based on the following components:
- The American Society of Anesthesiologists score (3, 4, or 5)[18]
- Operative wound classification (contaminated or dirty)
- Duration of surgery (≥75% percentile).
SSI was the dependent variable and was diagnosed based on physical examination, signs, and symptoms of infection at the surgical site also positive swab wound cultures and tissue cultures, which were obtained from the patients' charts. This variable was used as a binary variable with no SSI as the reference category.
Data were analyzed using Statistical Analysis System (SAS® version 9.2, SAS Institute Inc. 2008, Cary, NC USA). The proportion of SSI was calculated with 95% confidence interval (CI). Chi-square test used to compare categorical variables with the outcome whereas continuous variables used Student's t-test. The association of independent variables with the infection was analyzed using logistic regression model. Model fit was checked using the Hosmer–Lemeshow (HL) goodness of fit test. An HL statistic <15.5 (8° of freedom; P > 0.05) indicates no evidence of lack of fit. The strength of association was estimated using odds ratio (OR) with 95% CI and P < 0.05.
The study was reviewed and approved by the Institutional Review Board at King Abdullah International Medical Research Centre.
Results
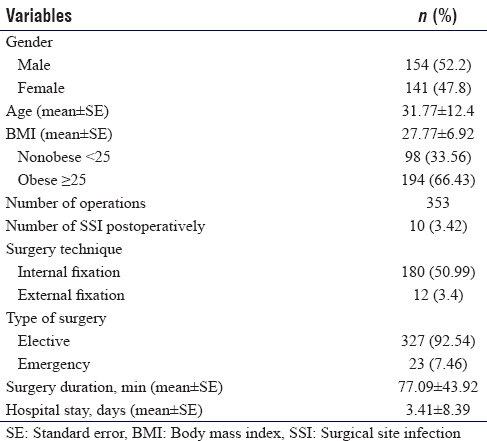
Out of 295 patients who were operated on, only 10 had documented postoperative SSI. The incidence of SSI was 3.42%. Males were the majority (70%) of SSI patients. The demographic characteristics of the study are summarized in [Table - 1].
Of the infectious organisms, methicillin-resistant Staphylococcus aureus was the most prevalent as it affected three patients. Staphylococcus coagulase-negative was the second prevalent organism affecting two patients. The other organisms include Pseudomonas stutzeri, Enterococcus faecalis, Enterobacter sp, Citrobacter freundii, and Escherichia coli, all of which were found once.
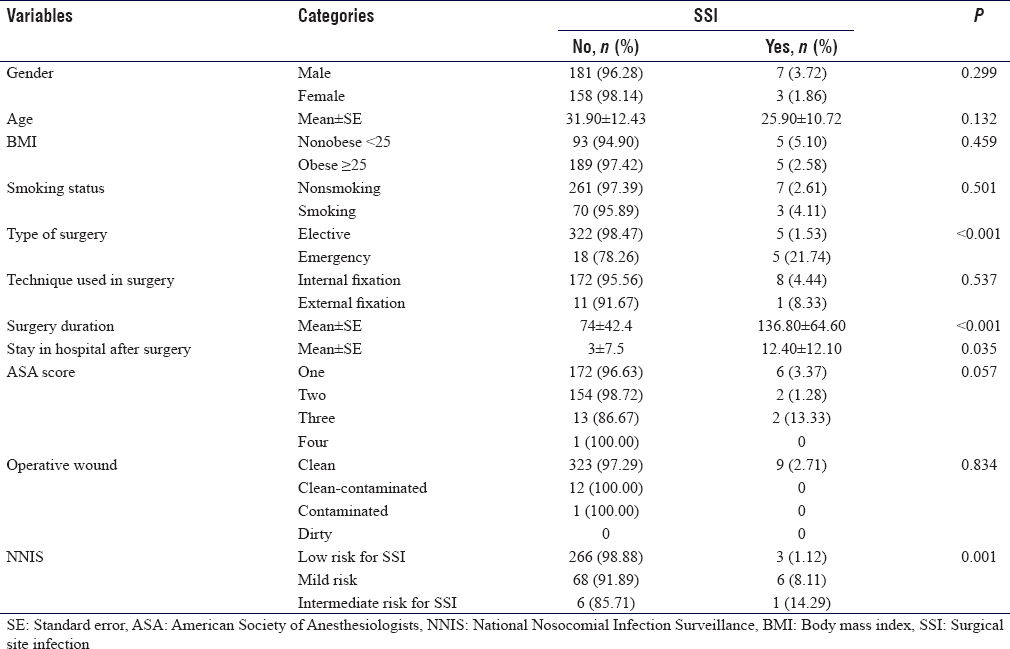
The univariate analysis showed a significant association between the type of surgery performed and the postoperative SSI, as SSI was diagnosed in 21.74% of the emergency surgeries (P < 0.001). The NNIS score was higher in patients who contracted an SSI (P = 0.001). [Table - 2] demonstrates the univariate analysis.
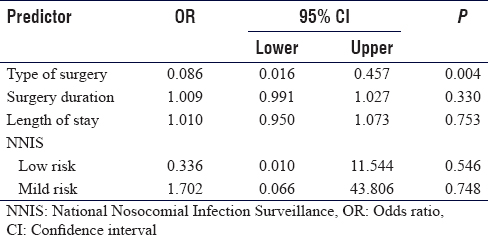
Stepwise multivariate logistic regression model [Table - 3] demonstrated that the type of surgery (OR 0.086 [95% CI 0.016–0.457]; P = 0.004) was a significant predictor of acquiring SSI after the surgery. The HL statistic showed no evidence of model lack of fit (P = 0.358).
Discussion
Our study found the incidence of SSI following foot and ankle surgery to be 3.42%. This estimate is slightly higher than the 2.55% reported previously following orthopedic surgeries in our country [11] and lower than the 6.8%, which has been reported by Khairy et al.[19] In the area of foot and ankle surgeries, the prevalence of postoperative infections varied from 1.0% to 6.5%, which is consistent with our study.[20],[21]
This study found the surgery type (emergency vs. elective) to be a significant predictor of SSI. Nevertheless, other variables, such as gender, were identified by previous studies as independent predictors of SSI as males were found to be more susceptible to SSI, which was not the case in our study.[22]
Although the duration of surgery was significant in the univariate analysis, it was not significant in the regression analysis despite being found as an independent predictor in prior studies.[1],[23] In theory, increasing surgery duration may lead to the increase of the wound exposure to microorganisms and more tissue damage.[24] In univariate analysis, we also found that increase in the length of hospital stay is a significant factor for the development of SSI while in multivariate analysis, it was not, and in another study, the length of the hospital stay was a significant factor, which could be because of the exposure to hospital environment and bacteria.[24]
Similar to the literature, SSI rates in our study were much higher in emergency surgeries than elective ones.[19] Although the total number of emergency surgeries included in the study was small, half of SSI patients had an emergency surgery. The severity of the surgical injury, greater difficulty of the surgical technique, and lack of preoperative patient preparation may contribute to SSI development among patients undergoing emergency surgeries.[13],[25] Another potential explanation for these findings has to do with the standard practice for treatment, which requires a prolonged hospital stay. This, in turn, may expose patients to a higher risk of iatrogenic diseases.
There are several limitations that need to be taken into account in light of these findings. One potential factor may be a referral bias because KAMC has a good reputation across Saudi Arabia. The study is also limited by the small sample size. Due to our small sample and young population in the study, there was no patient with SSI that had diabetes mellitus. It was expected, however, to find an association between encountering SSI and having diabetes mellitus.[14] Therefore, diabetes could not be studied as independent risk factors for SSI after foot and ankle surgery. Despite these limitations, this is the first study that informs clinicians, researchers, and policy makers about the incidence and predictors of SSI among foot and ankle patients in Saudi Arabia.
Conclusions
This study found age and surgery type to be significant predictors of SSI. Proper postoperative monitoring for high-risk patients may facilitate reduction of SSIs following foot and ankle surgery and improves health outcomes.
Acknowledgment
We appreciatively recognize Ms. Shaden B. Al-Subaih without who this study would not have been possible. We would like to express our gratitude for her assistance and cooperation in data collection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
OAA-M conceived and designed the study. ASA and MAO conducted research, provided research materials, and collected and organized data. MIB analyzed and interpreted data. NSA-K wrote initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery: A comparison of patients with and without diabetes. Diabetes Care 2011;34:2211-3. [Google Scholar] |
| 2. | Maragakis LL, Cosgrove SE, Martinez EA, Tucker MG, Cohen DB, Perl TM. Intraoperative fraction of inspired oxygen is a modifiable risk factor for surgical site infection after spinal surgery. Anesthesiology 2009;110:556-62. [Google Scholar] |
| 3. | Bolon MK, Hooper D, Stevenson KB, Greenbaum M, Olsen MA, Herwaldt L, et al. Improved surveillance for surgical site infections after orthopedic implantation procedures: Extending applications for automated data. Clin Infect Dis 2009;48:1223-9. [Google Scholar] |
| 4. | Kaabachi O, Letaief I, Nessib MN, Jelel C, Ben Abdelaziz A, Ben Ghachem M. Prevalence and risk factors for postoperative infection in pediatric orthopedic surgery: A study of 458 children. Rev Chir Orthop Reparatrice Appar Mot 2005;91:103-8. [Google Scholar] |
| 5. | Wiewiorski M, Barg A, Hoerterer H, Voellmy T, Henninger HB, Valderrabano V. Risk factors for wound complications in patients after elective orthopedic foot and ankle surgery. Foot Ankle Int 2015;36:479-87. [Google Scholar] |
| 6. | Zhang W, Chen E, Xue D, Yin H, Pan Z. Risk factors for wound complications of closed calcaneal fractures after surgery: A systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 2015;23:18. [Google Scholar] |
| 7. | Hranjec T, Swenson BR, Sawyer RG. Surgical site infection prevention: How we do it. Surg Infect (Larchmt) 2010;11:289-94. [Google Scholar] |
| 8. | Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:605-27. [Google Scholar] |
| 9. | Prasanna SS, Korner-Bitensky N, Ahmed S. Why do people delay accessing health care for knee osteoarthritis? Exploring beliefs of health professionals and lay people. Physiother Can 2013;65:56-63. [Google Scholar] |
| 10. | Scott RD. The Direct Medical Costs of Healthcare-Associated Infection in U.S. Hospitals and the Benefits of Prevention. Atlanta: CDC; 2009. Available from: http://www.cdc.gov/HAI/pdfs/hai/Scott_Costpaper.pdf. [Last accessed on 2016 Apr 18]. [Google Scholar] |
| 11. | Al-Mulhim FA, Baragbah MA, Sadat-Ali M, Alomran AS, Azam MQ. Prevalence of surgical site infection in orthopedic surgery: A 5-year analysis. Int Surg 2014;99:264-8. [Google Scholar] |
| 12. | de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: Incidence and impact on hospital utilization and treatment costs. Am J Infect Control 2009;37:387-97. [Google Scholar] |
| 13. | Kamat US, Fereirra AM, Kulkarni MS, Motghare DD. A prospective study of surgical site infections in a teaching hospital in Goa. Indian J Surg 2008;70:120-4. [Google Scholar] |
| 14. | Wukich DK, Crim BE, Frykberg RG, Rosario BL. Neuropathy and poorly controlled diabetes increase the rate of surgical site infection after foot and ankle surgery. J Bone Joint Surg Am 2014;96:832-9. [Google Scholar] |
| 15. | Harbarth S, Huttner B, Gervaz P, Fankhauser C, Chraiti MN, Schrenzel J, et al. Risk factors for methicillin-resistant Staphylococcus aureus surgical site infection. Infect Control Hosp Epidemiol 2008;29:890-3. [Google Scholar] |
| 16. | Ralte P, Molloy A, Simmons D, Butcher C. The effect of strict infection control policies on the rate of infection after elective foot and ankle surgery: A review of 1737 cases. Bone Joint J 2015;97-B:516-9. [Google Scholar] |
| 17. | Suen LJ, Huang HM, Lee HH. A comparison of convenience sampling and purposive sampling. Hu Li Za Zhi 2014;61:105-11. [Google Scholar] |
| 18. | Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 1991;91:152S-7S. [Google Scholar] |
| 19. | Khairy GA, Kambal AM, Al-Dohayan AA, Al-Shehri MY, Zubaidi AM, Al-Naami MY, et al. Surgical site infection in a teaching hospital: A prospective study. J Taibah Univ Med Sci 2011;6:114-20. [Google Scholar] |
| 20. | Butterworth P, Gilheany MF, Tinley P. Postoperative infection rates in foot and ankle surgery: A clinical audit of Australian podiatric surgeons, January to December 2007. Aust Health Rev 2010;34:180-5. [Google Scholar] |
| 21. | Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198-208. [Google Scholar] |
| 22. | Cohen B, Choi YJ, Hyman S, Furuya EY, Neidell M, Larson E. Gender differences in risk of bloodstream and surgical site infections. J Gen Intern Med 2013;28:1318-25. [Google Scholar] |
| 23. | Korol E, Johnston K, Waser N, Sifakis F, Jafri HS, Lo M, et al. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One 2013;8:e83743. [Google Scholar] |
| 24. | Mawalla B, Mshana SE, Chalya PL, Imirzalioglu C, Mahalu W. Predictors of surgical site infections among patients undergoing major surgery at Bugando Medical Centre in Northwestern Tanzania. BMC Surg 2011;11:21. [Google Scholar] |
| 25. | Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999;20:250-78. [Google Scholar] |
Fulltext Views
3,326
PDF downloads
1,391





