Translate this page into:
Post seizure bilateral simultaneous neck of femur fractures in a young adult
Corresponding Author:
Faisal S Alanazy
Department of Orthopaedic Surgery, King Saud Medical City, Ulaishah, 7790 Al Imam Abdul Aziz Ibn Muhammad Ibn Saud, Riyadh 12746 3617, Riyadh 12746
Saudi Arabia
dr.falanazy@gmail.com
| How to cite this article: Alenazi AA, Alanazy FS, Hashem AM, Alshugair IF, Alanazi AK, Alrashedan BS. Post seizure bilateral simultaneous neck of femur fractures in a young adult. J Musculoskelet Surg Res 2021;5:124-127 |
Abstract
The neck of femur fractures are common in the aging population. Young people typically sustain neck of femur fracture following a high-energy injury. Simultaneous bilateral neck of femur (BNOF) fractures in young patients are a rare entity. They might be sustained following a seizure episode. Timely diagnosis and treatment of these injuries are important and can affect the treatment modality and outcome. Internal fixation is desired in young, active, and healthy patients presenting with BNOF fractures. We report a case of a young adult presented with BNOF fractures following a single seizure episode. Bilateral open reduction and internal fixation using cannulated screws was chosen for this patient treatment. He was followed up for 2 years and showed a desirable outcome.
Introduction
Neck of femur fractures are common in the aging population and are estimated to be around 1.6 million annually worldwide.[1] In the young population, these fractures are typically due to high-energy mechanism of injury.[2],[3] They are almost always considered a surgical orthopedic entity that needs accurate reduction with stable fixation to decrease the risk of avascular necrosis (AVN) of the femoral head and nonunion.[4] Bilateral simultaneous hip fractures in young patients without a history of underlying diseases affecting bone mineralization are relatively rare and reported in the literature.[5],[6],[7] They can be sustained, as well as posterior shoulder dislocations or proximal humerus fractures, due to seizure episodes or following electrical shock injuries and can be initially missed causing a delay in treatment.[8],[9] In general, the neck of femur fractures can be treated with internal fixation; cannulated screws, sliding hip screws, or cephalomedullary nail fixation with or without the need for open reduction.[10],[11] Valgus intertrochanteric osteotomy or revision of internal fixation, is reserved for cases with nonunion.[12] Core decompression and hip replacement are reserved for cases complicated with nonunion or in patients who have poor clinical conditions as a result of age or a disease that is affecting bone quality to the degree that can affect healing potential negatively.[13],[14] In the hip joint, muscles' contractions during a tonic-clonic seizure or electric shock can lead to peritrochanteric muscle contractions, causing posterior hip dislocation and neck of femur fracture, especially in patients with conditions affecting bone density.[8],[15] A thorough and complete physical examination of the musculoskeletal system should be performed in patients presenting following seizure episodes or electrical injuries with a high suspicion index. The general condition of these patients on presentation can be distracting to unforgiving injuries if missed.[5],[9] Internal fixation in patients with renal osteodystrophy presenting with the seizure-induced bilateral neck of femur (BNOF) fractures has been used successfully.[5] Hip replacement surgery is reserved for cases who had their injuries missed, or their fractures were complicated with AVN or nonunion following internal fixation, due to the high likelihood of compromised blood supply, or due to the poor condition of the patient or his bone quality.[6] In the current paper, we present a patient who had a tonic-clonic seizure episode causing BNOF fractures and was successfully managed. The patient was followed up for 2 years and showed a good outcome. We believe that displaying this case in literature is important as such a case can be encountered by emergency medicine personals and the general condition of postictal patients can mask such an injury. Moreover, different treatment approaches have been reported in the literature for such patients.
Case Report
An 18-year-old male was brought to the emergency department (ED) following a single episode of a tonic-clonic seizure at home, followed by loss of consciousness. The exact duration of the seizure fit was unknown, as there was no witness to the event. He was drowsy and was complaining of bilateral hip pain on the presentation. He was investigated in the ED, and computed tomography (CT) of the brain and abdomen was ordered. CT abdomen showed bilateral hydroureteronephrosis that was likely related to atonic neurogenic bladder, and BNOF fractures and CT brain showed no acute brain injury. His laboratory investigations were unremarkable except for high urea, creatinine, low calcium, and Vitamin D levels.
Nephrology, neurology, and orthopedic surgery were involved in the management of the patient. Upon assessment by orthopedic surgery, the patient was conscious and oriented, and his vital signs were within normal limits. The patient had a history of a neurogenic bladder from the age of 5 years, for which he never sought medical opinion since the diagnosis did not cause him any complications before presentation to our hospital. His family, social, and surgical history were unremarkable, and there was no history of seizure episodes in the past. On examination, he had bilateral groin tenderness, and there were no distal neurovascular deficits. Plain radiographs of the pelvis showed BNOF fractures, and the patient was cleared for surgical intervention [Figure - 1].
 |
| Figure 1: Anteroposterior radiographs of the pelvis showing a displaced bilateral subcapital neck of femur fractures |
Surgical technique and outcome
The patient was placed on a supine position on a traction table under general anesthesia. Intraoperative fluoroscopy was used for a trial of closed reduction for each hip, which failed. The traction was loosened, and an open reduction and fixation using cannulated screws was initiated through an anterolateral approach to each hip sequentially, which was successful. On the 1st day postoperatively, clinical examination was unremarkable, and physiotherapy with a passive range of motion exercises as tolerated was started, and his postoperative radiographs were satisfactory. The patient was discharged on the 4th postoperative day with follow-up with nephrology and neurology and instruction for nonweight-bearing mobilization in a wheelchair. He was given calcium and cholecalciferol by nephrology, and levetiracetam by neurology. He was seen in the clinic 2 weeks postoperatively, and the wound was found to be clean, clips were removed, and the hip radiograph was satisfactory. Weight-bearing was initiated at 8 weeks postoperatively, and he regained his normal functional status by 10 weeks. He was followed for 2 years, and there were no complications related to the fracture, and the patient did not sustain any other seizure episodes to his knowledge [Figure - 2]. The patient was scheduled for a DEXA scan multiple times, but he did not show up for his appointments. He is on a frequent follow-up with nephrology, and his condition was well and did not necessitate any medical intervention.
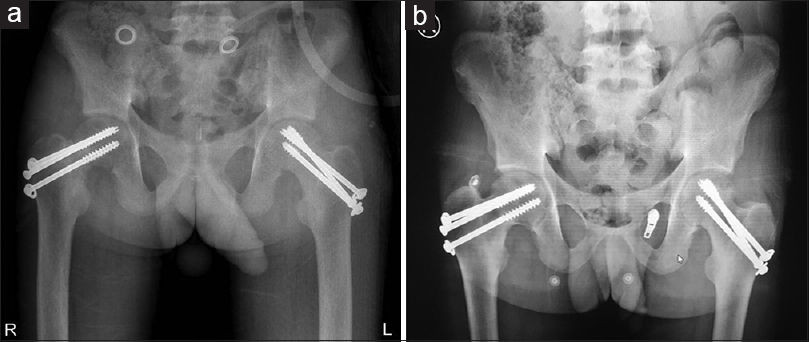 |
| Figure 2: Anteroposterior radiographs of pelvis taken on 8 weeks (a) and 2 years (b) postoperatively, which show good healing progression |
Discussion
During an electric shock, vigorous muscle contractions can lead to a neck of femur fracture, posterior shoulder dislocation, or proximal humerus fracture in patients with no history of chronic kidney disease.[9],[15] This can explain our case's presentation as his general condition was well and did not need any medical treatment directed to his neurogenic bladder after presentation or dialysis until the last follow-up. BNOF fractures in young patients induced by muscular spasm following either a seizure episode or electric injury are rare and reported in the literature.[5],[6],[7],[8],[9],[10],[11],[12],[13],[14],[15] They typically occur as a result of high-energy trauma in a young, healthy population.[2] The underlying renal disease can affect bone mineral density, quality, tensile stiffness, and remolding potential.[5],[6],[16],[17] An increased rate of nonunion has been found in a displaced neck of femur fractures in general.[4] A higher rate has also been found in patients with chronic kidney disease even in acutely and adequately treated cases due to the underlying secondary metabolic bone changes.[18] The risk of AVN following the neck of femur fractures is about 14.3%.[19] It can be caused by an increase in intracapsular pressure in minimally displaced fractures through a tamponade effect, or from a direct trauma to the femoral head blood supply.[20] John et al. reported three cases with end-stage renal disease on hemodialysis, who sustained BNOF fractures following uremic or hypercalcemic-induced seizures who were 15, 44, and 64 years old.[21] Two of their cases were presented late, one was not a candidate for internal fixation because of age, and the other patients' fractures were treated with internal fixations but were complicated with nonunion.[21] Alkaramani et al. reported a 31-year-old male with a history of anabolic steroid and growth hormone abuse for bodybuilding who sustained BNOF fracture following an episode of a tonic-clonic seizure as a result of hormonal imbalance.[7] They chose to treat him with a sliding hip screw on the left side due to comminution and cannulated screws on the right side. Sathyanarayana et al. reported a 23-year-old male with an end-stage renal disease on dialysis who was diagnosed on the 3rd day with BNOF fractures following a seizure episode.[6] They chose to treat the patient with bilateral uncemented hemiarthroplasty considering his age and time of the treatment as it was considered late, general condition, bone quality, and prognosis as he was planned for renal transplant.[6] Our patient has a chronic kidney disease secondary to a neurogenic bladder and was not mandating dialysis and his only significant finding on presentation was an elevated urea and creatinine levels. Internal fixation of these fractures is desired in young, healthy, and active patients when possible to restore the native hip biomechanics.[18],[22] Other than increased blood loss with sliding hip screw fixation compared to cannulated screw fixation, no significant difference was found in the outcome regarding the nonunion rate, function, and AVN of the femoral head when these two modalities were compared.[22] We believe that the good outcome in our case was a result of rapid recognition and treatment of the injury and the patient's general health. Considering that simultaneous BNOF fractures following a seizure episode is a rare entity with different treatment approaches in literature driven by the condition of the patient, and timing of the diagnosis, made us consider reporting this case in literature.
Conclusion
Further investigations are important for patients presenting following a generalized seizure episode because they might have a concomitant neck of femur fractures, which are critical to identify and manage. Rapid recognition and treatment of these injuries, along with the general health of patients, are important factors in deciding the treatment type of neck of femur fractures. Internal fixation of the bilateral neck of femur fractures following a seizure episode in a young patient with mild chronic kidney disease can be considered a good treatment option.
Ethical consideration
The authors certify that they have obtained all appropriate written patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AAA, BSA, and FSA conceived the study. AMH, IFA, and AKA collected, provided, and organized materials and data of the patient. AAA, BSA, and FSA wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-33. [Google Scholar] |
| 2. | Ye Y, Hao J, Mauffrey C, Hammerberg EM, Stahel PF, Hak DJ. Optimizing stability in femoral neck fracture fixation. Orthopedics 2015;38:625-30. [Google Scholar] |
| 3. | Thomas CD, Mayhew PM, Power J, Poole KE, Loveridge N, Clement JG, et al. Femoral neck trabecular bone: Loss with aging and role in preventing fracture. J Bone Miner Res 2009;24:1808-18. [Google Scholar] |
| 4. | Papakostidis C, Panagiotopoulos A, Piccioli A, Giannoudis PV. Timing of internal fixation of femoral neck fractures. A systematic review and meta-analysis of the final outcome. Injury 2015;46:459-66. [Google Scholar] |
| 5. | Mataliotakis G, Lykissas MG, Mavrodontidis AN, Kontogeorgakos VA, Beris AE. Femoral neck fractures secondary to renal osteodystrophy. Literature review and treatment algorithm. J Musculoskelet Neuronal Interact 2009;9:130-7. [Google Scholar] |
| 6. | Sathyanarayana V, Patel MT, Raghavan S, and Naresh D. Simultaneous bilateral femur neck fracture in a young adult with chronic renal failure- A case report and review of literature. J Orthop Case Rep 2015;5:24-6. [Google Scholar] |
| 7. | Alkaramani E, Salameh M, Adam M, George B, Alser Y, Ahmed G. Simultaneous bilateral neck of femur fracture in a young adult with underlying metabolic disturbances. Hindawi Case Reports in Orthopedics 2020:3. Article ID 8972542, https://doi.org/10.1155/2020/8972542. [Google Scholar] |
| 8. | Nekkanti S, Vijay C, Sujana Theja JS, RaviShankar, Raj S. An unusual case of simultaneous bilateral neck of femur fracture following electrocution injury-A case report and review of literature. J Orthop Case Rep 2016;6:70-2. [Google Scholar] |
| 9. | Sohal HS, Goyal D. Simultaneous bilateral femoral neck fractures after electrical shock injury: A case report. Chin J Traumatol 2013;16:126-8. [Google Scholar] |
| 10. | Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: Current management. J Orthop Trauma 2015;29:121-9. [Google Scholar] |
| 11. | Guo J, Dong W, Jin L, Yin Y, Zhang R, Hou Z, et al. Treatment of basicervical femoral neck fractures with proximal femoral nail antirotation. J Int Med Res 2019;47:4333-43. [Google Scholar] |
| 12. | Banaszek D, Spence D, O'Brien P, Lefaivre K. Principles of valgus intertrochanteric osteotomy (VITO) after femoral neck nonunion. Adv Orthop 2018;2018:5214273. [Google Scholar] |
| 13. | Dooley BJ, Hooper J. Fibular bone grafting for non union of fracture of the neck of the femur. Aust N Z J Surg 1982;52:134-40. [Google Scholar] |
| 14. | Jackson M, Learmonth ID. The treatment of nonunion after intracapsular fracture of the proximal femur. Clin Orthop Relat Res 2002;119-28. [Google Scholar] |
| 15. | Powell HD. Simultaneous bilateral fractures of the neck of the femur. J Bone Joint Surg Br 1960;42-B: 236-52. [Google Scholar] |
| 16. | Goto NA, Weststrate AC, Oosterlaan FM, Verhaar MC, Willems HC, Emmelot-Vonk MH, et al. The association between chronic kidney disease, falls, and fractures: A systematic review and meta-analysis. Osteoporos Int 2020;31:13-29. [Google Scholar] |
| 17. | Jamal SA, Hayden JA, Beyene J. Low bone mineral density and fractures in long-term hemodialysis patients: A meta-analysis. Am J Kidney Dis 2007;49:674-81. [Google Scholar] |
| 18. | Kalra S, McBryde CW, Lawrence T. Intracapsular hip fractures in end-stage renal failure. Injury 2006;37:175-84. [Google Scholar] |
| 19. | Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury 2015;46:484-91. [Google Scholar] |
| 20. | Han S, Oh M, Yoon S, Kim J, Kim JW, Chang JS, et al. Risk stratification for avascular necrosis of the femoral head after internal fixation of femoral neck fractures by post-operative bone SPECT/CT. Nucl Med Mol Imaging 2017;51:49-57. [Google Scholar] |
| 21. | John R, Kumar P, Aggarwal S, Rajnish RK, Agarwal S, Vatsyan K. Simultaneous, non-traumatic, bilateral neck femur fractures in uremic renal osteodystrophy: A report of three cases and literature review. J Orthop Case Rep 2018;8:90-4. [Google Scholar] |
| 22. | Shehata MS, Aboelnas MM, Abdulkarim AN, Abdallah AR, Ahmed H, Holton J, et al. Sliding hip screws versus cancellous screws for femoral neck fractures: A systematic review and meta-analysis. Eur J Orthop Surg Traumatol 2019;29:1383-93. [Google Scholar] |
Fulltext Views
1,893
PDF downloads
972





