Translate this page into:
Pulled elbow: Diagnosis and management, the Paraguay experience
*Corresponding author: Alberto Daniel Navarro Vergara, Servicio de Ortopedia y Traumatologia, Hospital de Trauma Manuel Giagni, General Santos Casi Teodoro S Mongelos, Asuncion, Paraguay. djocote@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vergara AD. Pulled elbow: Diagnosis and management, the Paraguay experience. J Musculoskelet Surg Res 2022;6:144-7.
Abstract
Objectives:
The objectives of the study were to show the Paraguay experience in the diagnosis and handling of pulled elbows in recent years.
Methods:
A retrospective study of patients who presented to the emergency service was carried out from July 2019 to December 2021. Patients under 6 years with typical symptoms and signs of pulled elbow were included in the study. The data collected were demographics, affected side, mechanism of injury, and number of times pulled elbow occurred. The maneuver performed for the treatment and its success was also recorded.
Results:
There were 30 pulled elbow cases in 26 patients. Age ranged from 1 to 5 years, with a median of 3 years. The left side was more frequently affected (53%). There were more females affected (77%). The main mechanism of injury was upper limb traction, which occurred in 26 elbows (86.6%), followed by falling from a standing height in four cases. We found that imaging studies are requested when the reason for consultation is referred to as a possible fall from one’s own height. The hyperpronation method of reduction was effective in all cases. The treating physician felt the “click” in 93.3% of the times.
Conclusion:
The pulled elbow is a frequent injury in pediatric emergencies. It requires a high index of suspicion to make the diagnosis and a training to perform the hyperpronation reduction maneuver. Physicians subjected to the diagnosis and reduction maneuver training, can treat these injuries successfully without consultation of pediatric orthopedics.
Keywords
Nursemaid elbow
Pulled elbow
Children
Trauma
Hyperpronation
INTRODUCTION
Pulled elbow, commonly known as nursemaid’s elbow, is one of the common musculoskeletal injuries in children under 4 years of age and is rarely found in patients over 5 years of age. Its maximum incidence is between the age of 1 and 3 years.[1] There is a predominant involvement of females and the left side.[2] At present, around 20% of the upper extremity injuries, involving the elbow, are pulled elbows in the age group of under 4 years,[3] with a decrease in the percentage in the past decades in trauma emergencies, as many of them go to primary care centers.
The trauma mechanism responsible for the injury is a sudden longitudinal traction of the hand while the forearm is in pronation and the elbow is in extension with permision of Gundel et al. [Figure 1].[4,5]

- The mechanism of pulled elbow. The arrow shows the direction of the pull.
This type of injury is possible due to the nature of the anatomy of the affected area.[5] The head of the radius is oval, not circular as one might think. When the forearm is supinated, the anterior aspect of the head rises sharply from the neck, so when traction is applied in this position, the annular ligament is impacted against this prominence. However, this does not happen when the forearm is in pronation. In pronation, the bone elevation is gradual, therefore, when traction occurs in that position, the annular ligament slips behind the lower part of head of the radius, interposing between the humeral capitulum and radial dome when the pulling force is released. In patients older than 5 years are less susceptible to pulled elbow, due to anatomic changes at the insertion of the annular ligament, where it thickens and strengthens.[4-6]
The recurrence rate of pulled elbow is 5–39% depending on the reference population studied and it can affect the same or the contralateral arm.[6]
Unfortunately, there are no available epidemiological reports available on the Paraguayan population and very few in the region, which is why we describe here our experience in the past 2 ½ years, in terms of diagnosis and treatment.
MATERIALS AND METHODS
A retrospective study of patients who presented to the emergency service was carried out, from July 2019 to December 2021. Patients under 6 years of age who presented with a clinical picture compatible with pulled elbow were included in the study. The typical pulled elbow presentation includes a history of a child’s caregiver pulling the elbow or a fall from height, upper limb acute pain, the upper limb is close to the child’s body who is refusing to move it, no elbow swelling, and with possible previous positive history of a pulled elbow. Presentations related to severe trauma or with signs of fractures (swelling, ecchymosis, and deformities) were excluded from the study.
The data evaluated were demographics, affected side, mechanism of injury, and number of times pulled elbow occurred. The maneuver performed for the treatment, its success (click sensation and active motion at 5 min), and the use or not of immobilization at discharge were also recorded. All maneuvers were performed by a specialist in pediatric orthopedics, with the hyperpronation technique being the only maneuver performed.[6,7]
RESULTS
Twenty-six patients were included in this study with 30 pulled elbow incidences. Four patients had a similar event before, but with widely spaced interval (at least 6 months apart) between the events to consider them recurrences. [Table 1] shows the main results, grouped by gender, affected side, and mechanism of trauma.
| Age | Gender | Side | Mechanism |
|---|---|---|---|
| 4 | Female | Left | Traction |
| 4 | Female | Left | Traction |
| 3 | Female | Left | Traction |
| 2 | Female | Left | Fall |
| 3 | Male | Right | Traction |
| 2 | Female | Left | Traction |
| 3 | Male | Right | Traction |
| 3 | Male | Right | Traction |
| 1 | Female | Left | Traction |
| 3 | Male | Right | Traction |
| 2 | Male | Right | Traction |
| 2 | Female | Right | Traction |
| 3 | Male | Left | Fall |
| 3 | Female | Right | Traction |
| 3 | Female | Right | Fall |
| 3 | Female | Right | Traction |
| 3 | Female | Left | Traction |
| 2 | Female | Left | Traction |
| 1 | Female | Left | Traction |
| 3 | Female | Left | Traction |
| 4 | Female | Left | Fall |
| 3 | Female | Left | Traction |
| 3 | Female | Right | Traction |
| 3 | Female | Left | Traction |
| 4 | Female | Right | Traction |
| 2 | Female | Right | Traction |
| 4 | Female | Left | Traction |
| 2 | Female | Right | Traction |
| 2 | Female | Left | Traction |
| 5 | Male | Right | Traction |
Age ranged from 1 to 5 years, with a median of 3 years. The left elbows were affected in 14 patients (53.8%), while the right side was affected in 12 patients (46.1%). Females were affected more (77%) than males. The main mechanism of trauma was traction of the upper limb, which occurred in 26 cases (86.6%) followed by falling from a standing height in four cases. All patients presented in <14 h after the trauma and none of them reported any manipulation before presentation.
It was the 1st time for 26 (86.6%) patients, and on four occasions, the parents reported a previous similar event in the same elbow. However, the time interval between the first and the second events was at least 6 months.
It was found that, out of the 30 cases, the pediatrician requested radiographs on 20 occasions (66.6%). None of them found bone lesions, when they were evaluated by the specialist. In the remaining events, a consultation of a pediatric orthopedic specialist was requested before requesting supplementary studies. On evaluation of the patient, imaging studies were not considered necessary to reach the diagnosis. It was found that there were more imaging requests when the history of falling from height was the reason for the presentation. The hyperpronation method was effective in all cases, with the maneuver being repeated in 2 cases (6.66%) as no click or clinical improvement was observed after 5 min. The treating physician felt the click in 93.3% of the times.
DISCUSSION
At present, the treatment of pulled elbows has been widely effective.[8-10] Our series had a peak incidence similar to that described in the literature, but it should be noted that Takashi et al.[2] described a high number of cases in children under 1 year of age, with 6 months of age being the maximum frequency of elbow subluxation events in their group. They attributed that to the fact that the infants begin to turn actively on their bellies at that age. We did not have any cases younger than 1 year in our series. Regarding the common side affected; we did not have a statistically significant difference between the two sides. However, females were affected more than males, which is in agreement with available literature.[4,9-11]
We found a controversy in the literature for the indication for or against cast immobilization after reduction of the pulled elbow. Assad advocated the use of plaster in all patients with pulled elbow, since in their opinion, it has a significant impact on the number of recurrences.[10] We, as a general rule, never immobilize an elbow that was treated for pulled elbow with a cast, which is supported by many studies.[9-11] Knowing that recurrence is possible, we explain the injury mechanism to the parents, guiding them to avoid repeating the triggering maneuver, especially in the first 15 days after the event. Successful reduction (presence of the click and absence of pain) significantly reduces the possibility of a new spontaneous recurrence in the first few days. We believe that immobilizing the affected joint goes against the suspected diagnosis and that if we place the plaster, our management should be closer to that of a fracture at the elbow level rather than subluxation.
Our study did not have a recurrence rate in the short term (<6 months). We only had four patients with repeated episodes but separated by more than 6 months in each case.
The reduction maneuver that we used and gave us successful results is elbow hyperpronation with Permision of Gundel et al.[5] [Figure 2] in a 90° neutral position. A few times, the lack of the “click,” forced us to repeat the maneuver to obtain a successful reduction. There are two known reduction maneuvers for the reduction of pulled elbows, the supination-flexion maneuver and the hyperpronation (or forced pronation) maneuver. In both, the treating physician should feel the characteristic “click” that helps confirming the diagnosis.
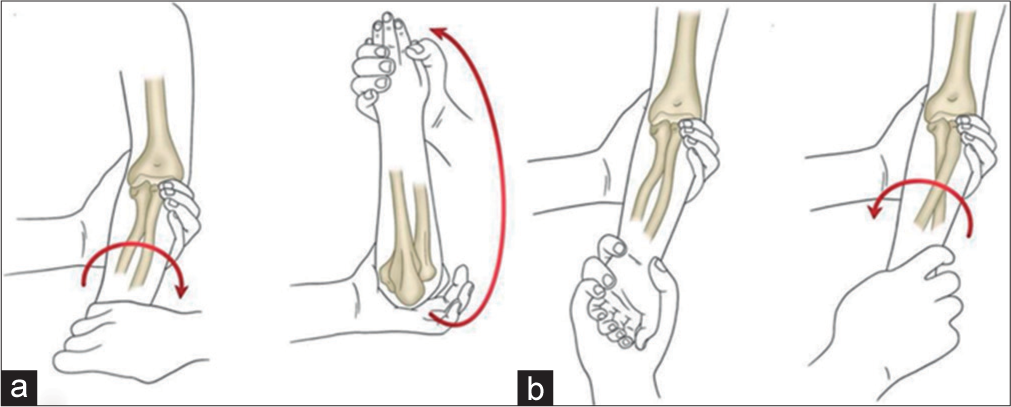
- Maneuvers methods. (a) Supination-flexion maneuver. (b) Hyperpronation maneuver. The arrow shows the direction of force to attain reduction.
CONCLUSION
The “nursemaid’s elbow” is a frequent injury in pediatric emergencies, it requires a high index of suspicion to make the diagnosis. It is not necessary to request radiological studies for diagnosis. The training of emergency physicians to diagnose and perform the hyperpronation maneuver is needed. With this training, the evaluation by a pediatric orthopedics is not necessary to obtain a successful treatment for pulled elbows.
AUTHOR’S CONTRIBUTION
The author has critically reviewed and approved the final draft and is responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The research protocol was approved by the Institutional Review Board on January 3, 2022. Grupo Premedic Circular #03012022.
DECLARATION OF PATIENT CONSENT
The author certifies that they have obtained all appropriate patient consent forms. In the form, the patient’s parent has given his consent for the patient’s images and other clinical information to be reported in the journal. The parent understands that the patient’s name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicts of interest.
References
- Upper extremity injuries In: John A. Herring, ed. Tachdjian's Pediatric Orthopaedics from the Texas Scottish Rite Hospital for Children (6th ed). Amsterdam, Netherlands: Elsevier; 2014. Ch. 29
- [Google Scholar]
- Investigation on 2331 cases of pulled elbow over the last 10 years. Pediatr Rep. 2014;6:5090.
- [CrossRef] [PubMed] [Google Scholar]
- Nursemaid's elbow-Supination-flexion technique versus hyperpronation/ forced pronation: Randomized clinical study. Indian J Orthop. 2019;53:117-21.
- [CrossRef] [PubMed] [Google Scholar]
- Suspected radial head subluxation. Pediatr Emerg Care. 2021;37:e58-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pronación dolorosa: Diagnóstico y manejo de urgencia [Nursemaid's elbow: Diagnosis and treatment in emergency department] Andes Pediatr. 2021;92:718-23.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic investigations of the mechanism of injury and pathologic anatomy of pulled elbow in young children. Clin Orthop. 1971;77:134-43.
- [Google Scholar]
- Effectiveness of reduction maneuvers in the treatment of nursemaid's elbow: A systematic review and meta-analysis. Am J Emerg Med. 2017;35:159-63.
- [CrossRef] [Google Scholar]
- Randomized comparison of pain perception during radial head subluxation reduction using supination-flexion or forced pronation. Pediatr Emerg Care. 2006;22:235-8.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of reduction maneuvers for “pulled elbow” in children: A prospective study of 115 cases. J Pediatr Orthop. 2014;34:432-6.
- [CrossRef] [PubMed] [Google Scholar]
- The treatment of pulled elbow: A prospective randomized study. Arch Orthop Trauma Surg. 2000;120:336-7.
- [CrossRef] [PubMed] [Google Scholar]
- “pulled elbow”: Report of two cases and review of the literature. J Pediatr Orthop B. 2010;19:304-6.
- [CrossRef] [PubMed] [Google Scholar]






