Translate this page into:
Acetabular development after open reduction to treat developmental dysplasia of the hip after walking age
*Corresponding author: Zulqurnain Rafiq, Department of Orthopedics, College of Medicine, King Saud University, Riyadh, Saudi Arabia. drzulqurnain@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bakarman KA, Alsiddiky AM, Zamzam MM, Rafiq Z. Acetabular development after open reduction to treat developmental dysplasia of the hip after walking age. J Musculoskelet Surg Res, 2023;7:104-9.
Abstract
Objectives:
Treatment of developmental dysplasia of the hip (DDH) with high hip dislocation in children using a one-stage operation appears tedious and associated with complications. This study aimed to assess a less traumatic approach for the surgical treatment of irreducible hips among children with DDH after walking age. The treatment strategy involved open reduction (OR) alone and non-invasive monitoring of acetabular development.
Methods:
This was a retrospective analysis of 22 hips of 20 female patients with complete dislocation of the hip and a mean age of 25.09 ± 4.6 months, performed between February 2013 and February 2018. All DDH patients underwent OR alone and had an irreversible hip dislocation. After surgery, a spica cast was applied for 6 weeks and then reduced to a broomstick cast for a considerable period. Finally, night abduction brace was placed until a normal acetabular index (AI) was obtained. The mean follow-up was 44.60 ± 12.36 months.
Results:
Out of 20 patients with DDH, 18 (90%) were successfully treated by OR alone. The main pre-operative AI of 41.82° ± 5.54° decreased to 16.19° ± 7.09° at the final follow-up (P < 0.001). An initial negative center-edge angle at the pre-operative stage gradually increased to a mean of 26.86° ± 6.56° during the follow-up period.
Conclusion:
Relatively less invasive approach adopted in this study not only obviated the need for an additional procedure but also had a favorable effect on the acetabular and hip joint development.
Keywords
Acetabular development
Acetabular index
Avascular necrosis
Center-edge angle developmental dysplasia of the hip
Open reduction
INTRODUCTION
After walking age, treating developmental dysplasia of the hip (DDH) is much more challenging. Delayed therapeutic intervention is fraught with unfavorable outcomes due to secondary acetabular and femoral changes due to the prolonged dislocation of the hip.[1] The pediatric orthopedic surgeon faces a challenging situation when treating hip subluxation or dislocation in a child after walking age due to DDH. Soft-tissue release, accurate open reduction (OR), and capsulorrhaphy are required to treat this condition.[2] Anterior OR utilizing the iliofemoral, Smith-Peterson or their modifications approach are the most widely used treatment approach for these children. Treatment for persistent acetabular dysplasia may include pelvic osteotomy and femoral osteotomy to address decreased hip remodeling capacity and facilitate reduction. Avascular necrosis (AVN) of the femoral head is a possible surgical complication that could have a negative impact on the final clinical and radiological outcomes.[3] This risk can be mitigated by the proximal femoral shortening osteotomy or using traction. How and when to combine various approaches is not well-defined.
The current treatment practice strategy is to achieve acetabular development that is best promoted by OR and pelvic osteotomy that may or may not be accompanied by a concomitant femoral shortening.[4] This combined single-stage approach is not only a cumbersome procedure but is also associated with several complications.[5] Being an extensive and technically demanding procedure, the combined single-stage procedure is considered more suitable for “high” dislocation and “older” children that are more likely to benefit from a shortening of the femur.[6,7] On the contrary, these claims lack consensus. First, the height of dislocation justifying femoral shortening has not yet been quantified, and second, the treatment options for older children, including the patient’s age, remain controversial.
The literature has established that the acetabulum’s remodeling is possible for a long period in the case of the femur head remaining in a reduced position.[8-10] The development of the acetabulum is primarily affected by a concentric reduction and its maintenance throughout the growth period.[10-12] In the present study, the treatment approach comprised primary OR followed by applying a spica cast converted to a broomstick cast postoperatively. Finally, night abduction brace was placed until the normal AI was achieved. This study aimed to develop a less traumatic treatment strategy for DDH with complete dislocation in children after walking age.
MATERIALS AND METHODS
This retrospective study was conducted between February 2013 and February 2018. It included 22 hips of 20 females with irreducible hip dislocation who were treated by OR alone. These patients were selected from a total of 430 hips (378 patients) who were treated at our institution [Figure 1]. Describes the selection criteria of the study population. OR and a pelvic osteotomy were performed in 240 hips, and femoral shortening was performed in 78 hips. Patients with teratological, paralytic, and pathological dislocations were excluded from the study. Similarly, patients who received surgical or nonsurgical treatment at an outside facility before presentation were not included in this research. Hips that were unreduced or reducible under tension requiring pelvic and femoral shortening were excluded from the study.

- Schematic description of selection of study population with developmental dysplasia of hip.
The criteria to proceed with OR were based on interoperative assessment without any cutoff age; these included the stable and reducible hips without tension on the femoral head. Parents of children were counseled and briefed before the surgery that the final decision regarding the need for a pelvic osteotomy would be made during the procedure. All patients had an anterolateral approach for the OR. The femoral head was manually distracted at 30° of hip flexion following reduction to measure joint tension before capsule closure. By inserting a McDonald of 3–4 millimeters size, tangential to the roof of the acetabulum, into the hip joint. Then, the acetabulofemoral distraction was assessed. The easy introduction of McDonald indicated a tension-free reduction, as illustrated in [Figure 2].

- Assessment method of the amount of distraction between femoral head and acetabulum by manual traction.
The spica cast application was made at 30–40° flexion, 30–40° abduction, and 10–15° of internal rotation. After the surgery, written spica care instructions were given to the parents. The post-operative hospital stay was for 24 h. After 6 weeks, the spica cast was converted to a broomstick cast, followed by a nighttime abduction brace that was gradually withdrawn when the normal acetabular index (AI) was obtained. In addition, data were extracted from the patient’s medical records for the patient’s age at index surgery, gender, Tönnis grades of hip dislocation, operation time in minutes, blood loss in milliliters, and duration of treatment.
The picture archiving and communication system was used for monitoring the hips radiographically during follow-up. Anteroposterior (AP) radiographs were recorded at pre-determined time points: right after the surgery; taken immediately following surgery; at 6 weeks or at the removal of the spica cast; then every 3 months for 1 year; and every 6 months until the last follow-up. The AI[13] and the center-edge angle (CEA)[14] were selected as the main outcome variables for determining the success of correcting the acetabular dysplasia and the resulting maintenance of that correction. An AI of <30° and a CEA of >10° were considered safe acetabular development.[15,16]
A radiographic evaluation was performed at each follow-up visit. Any lateralization of the femur head or disruption of the Shenton line on the standing AP radiograph was considered an indication of possible further intervention. The grading for the femur head’s AVN was done using the Kalamchi and MacEwen classification system criteria.[17] Multiple pediatric orthopedic consultant surgeons performed all pre- and postoperative procedures and assessments. The radiographic measurements were performed by a junior author (ZR) and reviewed by two senior authors (KB, KA).
Statistical analysis
The data were entered and analyzed using SPSS v 20.0. The repeated measures analysis of variance test was applied to compare the measurements taken preoperatively, postoperatively, and at the follow-up appointments. Multivariate linear regression analysis was used to model the relationship between the gender, side, and length of the broomstick cast on the terms “AI” and “CEA’.” An arbitrary P < 0.05 or less was considered to be significant.
RESULTS
Table 1 describes the characteristic features of 22 hips in 20 patients with DDH in this study. Two patients had bilateral dislocations, whereas 18 had unilateral dislocations. Ten hips were involved on the right, while 12 hips were involved on the left side. No intraoperative or immediate post-operative complications were encountered. In addition, the intraoperative blood loss was minimal.
| Characteristic | Number (%) |
|---|---|
| Gender (All females) | 20 (100) |
| Tönnis Grade 3 | 10 (45) |
| Tönnis Grade 4 | 12 (55) |
| Right-sided DDH | 10 (45) |
| Left-sided DDH | 12 (55) |
| Total number of hips | 22 |
| Mean age at surgery (months) | 25.09±4.6 |
| Mean Broomstick cast duration (months) | 4.86±1.3 |
| Mean abduction brace duration (months) | 2.1±1.2 |
| Mean follow-up duration (months) | 44.09±20.5 |
DDH: Developmental dysplasia of the hip
The management of 18 (90%) patients was completed with OR alone. The mean follow-up time was 44.95 ± 20.51 months. All the patients reported being pain-free at the last appointment and full physical activity with no limp. None of the patients complained of muscle weakness or Trendelenburg sign. The broomstick cast was kept for a mean duration of 4.8 ± 1.3 months to achieve hip stability by radiological parameters. With a mean duration of 2.1 ± 1.20 months, only seven (31.82%) patients were switched to nighttime hip abduction braces.
Yearly assessment of AI after surgery [Figure 3] revealed a significant improvement in AI at each visit from the preoperative AI (mean 42.05° ± 5.57°) until the latest follow-up (mean 16.19° ± 7.09°; P < 0.001). Although preoperatively, CEA was negative among all patients, a gradual yearly increase was observed at each follow-up appointment, reaching a maximum of 25.52° at the last appointment [Figure 4]. According to the Kalamchi and MacEwen classification, AVN was encountered in three hips. Two were classified as type I AVN and one as type II AVN. Patients with type I AVN had no residual deformity, while patients with type II deformity had varus de-rotation osteotomy to correct the valgus and excessive anteversion. [Figure 5] shows radiological improvement in AI and CEA.
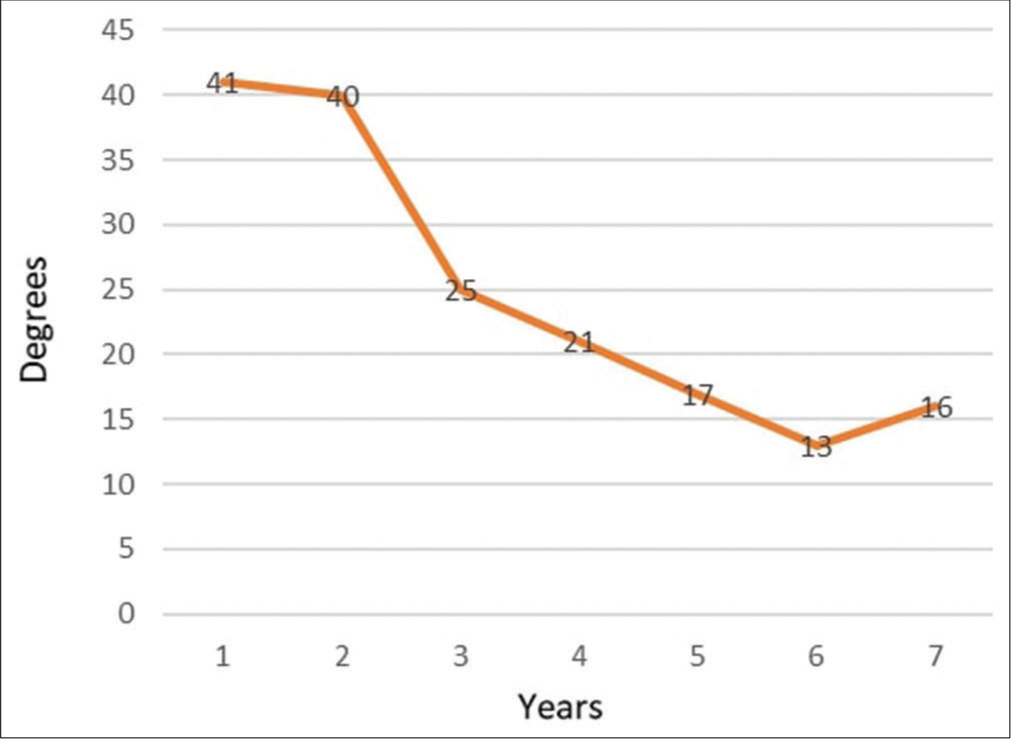
- Acetabular index values at different time intervals.
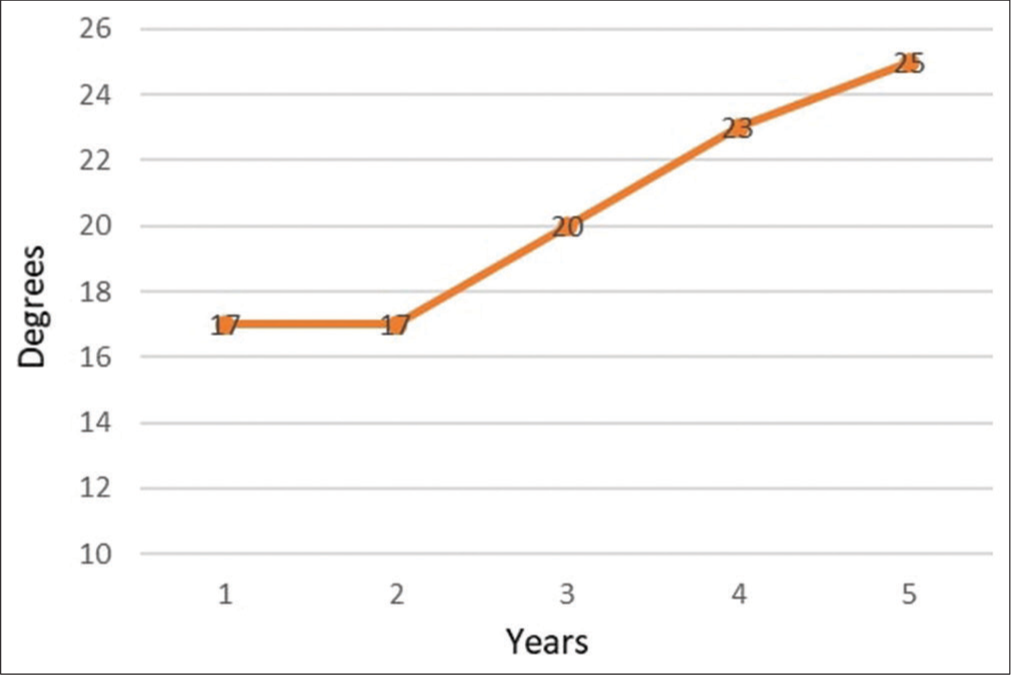
- Central-edge angle values at different time intervals.

- Serial radiographs of 36 months old girl with bilateral hip developmental dislocation: (a) Preoperative radiograph with dislocation Tönnis grade 4, (b) immediate postoperative (c) 6 weeks, (d) 6 months, (e), 28 months, and (f) 5 years postoperative radiograph showing excellent acetabular development.
The radiographically determined parameters for two patients (three hips, 10%), did not return to normal ranges. For one patient with bilateral DDH, removing the hip spica cast was followed by redislocation of the right hip. This patient was treated with OR, a Dega osteotomy plus femoral shortening. Subsequently, a subluxation with coxa valga occurred contralaterally. This had to be managed by repeat OR, Dega acetabuloplasty, and femoral shortening. The other patient developed lateralization of the femoral head with a limitation of range of motion, most likely due to the early removal of the broomstick cast. This patient was also treated with a repeat OR, comprising of Dega osteotomy and shortening of femur.
A regression model was calculated using age at surgery and side and broomstick cast duration as predictors for AI. Age was found to be the only significant predictor, with a beta value of 0.732 (P = 0.03), indicating that the AI increased by 0.7° for each year increase in age. Another regression model was calculated using age, side, and broomstick cast duration as predictors for the latest CEA. Age was found to be the only significant predictor, with a beta value of −0.689 (P = 0.008), indicating that the CEA increased by 0.6° for each year increment in age.
DISCUSSION
In this study, 18 (90%) DDH patients were treatment successfully with OR alone. All of these patients had crossed the walking age. The recent trend for older children with high dislocations is to perform pelvic osteotomy with femoral shortening in conjunction with OR.[3,4] The decision in the present study to perform OR alone was based solely on interoperative assessment disregarding the patient’s age. Several factors have been suggested in successful results after performing surgery. The patient’s age is particularly important.[12] In the present study, the mean age of the patients was 25.09 ± 4.6 months. Kagawa et al.[18] evaluated 43 hips of 38 children with Tönnis grade 3 and 4 hip displacements treated by an OR after walking age. In their study, it was observed that radiologically the hip joint development continued to improve until 6 years and, in some cases, up to 7–8 years.
Moreover, Brougham et al.[8] suggest that AI development ceases at 5 years of age. Their study included a serial analysis of 63 hips of 53 children. Closed reduction was performed for these children when they reached the age of 18 months. Albinana et al.,[16] in a 7-year follow-up study of 72 children (mean age 16 months) with DDH treated by open (n = 48) and closed reduction (n = 24), found that the acetabulum continued developing even after 4 years of surgery. The findings of the present study also revealed that the acetabulum kept developing for over 6 years of age following OR. Collectively these data point to the intrinsic potential of acetabulum after 18 months of age for treatment of DDH. In addition, this approach to treating DDH also avoided the need for secondary procedures.
Femoral shortening was not performed in the present study for complete dislocations based on the intraoperative assessment yielding highly favorable results. Avoidance of femoral shortening was based on the criteria of interoperative assessment of the stability of the hip joint, subjective assessment of soft-tissue tension, and ease of reduction without any pressure on the femoral head.[6] Previously, it was recommended that femoral shortening should always be performed for complete dislocation of the hip as a single-stage procedure to avoid future intervention.[19,20] This one-stage approach has been criticized for being too aggressive and avoidance of femoral shortening by the adoption of an individualized approach will not only decrease the operating time, blood loss, and hospital stay[5,6] but also circumvents the need for a follow-up surgery for removing the hardware.[6,7]
Moreover, if such a femur shortening procedure is performed, which was not warranted in the first place, in that case, this could inadvertently reduce the soft-tissue tension in the area surrounding the joint, thereby increasing the risk of re-dislocation. The other major pitfall of the combined procedure is that excessive de-rotation of the femur to rectify the ante-version may lead to posterior instability, particularly if combined with the Salter innominate osteotomy.[21] By adopting similar criteria, Ibrahim et al.[22] successfully treated 39 hips with a mean age of 27.6 months; 95% were Tönnis grades 3 and 4, and femoral shortening was performed for only 14 patients. These data suggest that applying an individualized approach for avoiding femoral shortening yielded not only favorable results for the treatment of DDH but also prevented the requirement for any additional surgery.
It has been claimed that acetabular dysplasia in DDH is not an actual defect. On the contrary, it has been described as resulting when the acetabular apparatus fails to ossify.[23] Magnetic resonance imaging evaluation of the morphology of the acetabulum has revealed that in cases, where bony coverage is inadequate on radiographs, the growth of the acetabulum may progress normally, which provided that the cartilage cover is intact.[24,25] Several studies have also reported that concentric reduction and maintenance of reduction are the primary factors influencing acetabular growth.[11,12,26]
After 6 weeks, the spica cast was converted to a broomstick cast, which maintained the reduction and allowed for a sufficient range of motion movements in all directions, particularly hip flexion and extension. This dynamic mechanical loading may have regulated endochondral ossification resulting in rapid improvement in the acetabular depth and width caused by ossification that occurs both appositionally and interstitially.[27,28]
Radiologically, the acetabulum’s development is strongly predicted by the AI,[29] whereas CEA suggests a relationship between the acetabular development and that of the femur head.[14] To validate the CEA, an age of at least 4 years has been suggested. However, a high interobserver reliability has been found in studies assessing the CEA in patients younger than four.[30] In the present study, the development of acetabulum in DDH patients was evaluated by AI and CEA during follow-up after OR. On each follow-up appointment, a significant decrease in AI was observed in [Figure 3]. For CEA, a significant increase was reported at each follow-up appointment in [Figure 3], with a mean CEA of 26.86° ± 6.56° reported at the last appointment. The changes in AI and CEA at the latest follow-up had negative and positive slopes, respectively. The present study suggests that AI and CEA improved if a concentric reduction was made and maintained during the growth period. This is consistent with studies that acetabular ossification occurs most rapidly during the first 4 years of life.[28,31]
This study was, however, limited by small number of patients and relatively shorter follow-up. Large scale studies are recommended for validation of the findings of this study.
CONCLUSION
For treatment of DDH with easily reducible, complete dislocation of hips after walking age with OR and keeping the patients on prolonged broomsticks casts was found to be a less invasive approach and obviated the need for secondary procedures. Moreover, this individualized approach imparted a favorable influence on the development of the entire hip joint.
ACKNOWLEDGMENT
The authors are grateful to Professor Zahid Shakoor of the immunology department for his constant support and insightful comments on our study.
AUTHORS’ CONTRIBUTIONS
KAB, AMA, MMZ and ZR developed the idea for the study, oversaw its execution, and contributed to the data set. Data were organized, processed, and evaluated by MMZ and ZR. KAB and AMA finished the draft and helped with logistics. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This research was approved by the Institutional Review Board of King Saud University’s College of Medicine on March 14, 2022 with reference No. 22/0242/IRB.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am. 1978;60:575-85.
- [CrossRef] [Google Scholar]
- A comparative study of nonoperative versus operative treatment of developmental dysplasia of the hip in patients of walking age. J Pediatr Orthop. 1997;17:181-8.
- [CrossRef] [Google Scholar]
- Single stage open reduction through a medial approach and innominate osteotomy in developmental dysplasia of the hip. J Bone Joint Surg Br. 2005;87:380-3.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral overgrowth following surgical treatment of long-established dysplasia of the hip. Acta Ortop Bras. 2009;17:139-43.
- [CrossRef] [Google Scholar]
- Predictors of the need for femoral shortening osteotomy during open treatment of developmental dislocation of the hip. J Pediatr Orthop. 2009;29:868-71.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of femoral shortening in the treatment of developmental dysplasia of the hip after walking age. J Child Orthop. 2019;13:371-6.
- [CrossRef] [PubMed] [Google Scholar]
- The predictability of acetabular development after closed reduction for congenital dislocations of the hip. J Bone Joint Surg Br. 1988;70:733-6.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging in acetabular residual dysplasia. Clin Orthop Relat Res. 1991;265:207-17.
- [CrossRef] [Google Scholar]
- Acetabular growth potential in congenital dislocation of the hip and some factors upon which it may depend. Clin Orthop Relat Res. 1976;119:99-106.
- [CrossRef] [Google Scholar]
- Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop. 1994;14:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular development after open reduction for developmental dislocation of the hip. 15-year follow-up of 22 hips without additional surgery. Acta Orthop Scand. 1998;69:17-20.
- [CrossRef] [PubMed] [Google Scholar]
- Translation: Hilgenreiner on congenital hip dislocation. J Pediatr Orthop. 1986;6:202-14.
- [CrossRef] [Google Scholar]
- Studies on dysplastic acetabula and congenital subluxation of the hip joint: With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:58.
- [Google Scholar]
- The frequency of congenital hip dislocation and congenital equinovarus in Sweden. Nord Med. 1956;55:221-3.
- [Google Scholar]
- Acetabular dysplasia after treatment for developmental dysplasia of the hip. J Bone Joint Surg Br. 2004;86:876-86.
- [CrossRef] [PubMed] [Google Scholar]
- Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62:876-88.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular development after open reduction to treat dislocation of the hip after walking age. J Orthop Sci. 2016;21:815-20.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results after open reduction of developmental hip dislocation by an anterior approach lateral and medial of the iliopsoas muscle. J Pediatr Orthop B. 2005;14:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am. 1989;71:734-41.
- [CrossRef] [PubMed] [Google Scholar]
- Combined open reduction and Dega transiliac osteotomy for developmental dysplasia of the hip in walking children. Acta Orthop Belg. 2019;85:545-53.
- [Google Scholar]
- Developmental hip dysplasia and dislocation: Part I. Instr Course Lect. 2004;53:523-30.
- [Google Scholar]
- Magnetic resonance evaluation of acetabular residual dysplasia in developmental dysplasia of the hip: A preliminary study of 27 patients. J Pediatr Orthop. 2010;30:37-43.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of cartilage coverage with magnetic resonance imaging in residual dysplasia and its impact on surgical timing. Acta Orthop Traumatol Turc. 2019;53:351-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61:112-8.
- [CrossRef] [PubMed] [Google Scholar]
- Development and injury of the triradiate cartilage with its effects on acetabular development: Review of the literature. J Trauma. 2003;54:1245-9.
- [CrossRef] [PubMed] [Google Scholar]
- Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39-47.
- [CrossRef] [Google Scholar]
- Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. Int Orthop. 2018;42:631-40.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement of center-edge angle in developmental dysplasia of the hip: A comparison of two methods in patients under 20 years of age. Skeletal Radiol. 2002;31:25-9.
- [CrossRef] [PubMed] [Google Scholar]
- Development of the osseous and cartilaginous acetabular index in normal children and those with developmental dysplasia of the hip: A cross-sectional study using MRI. J Bone Joint Surg Br. 2012;94:1625-31.
- [CrossRef] [PubMed] [Google Scholar]






