Translate this page into:
Diagnostic accuracy of phone messaging forwarded images for developmental dysplasia of the hip
*Corresponding author: Ahmad Almigdad, Department of Orthopedics, Royal Medical Services, King Hussein Medical Center, Amman, Jordan. akmigdad_just@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Almigdad A, Megdadi N, Banimelhem K, Al Omari B, Al Abdallat A, Almanasir G. Diagnostic accuracy of phone messaging forwarded images for developmental dysplasia of the hip. J Musculoskelet Surg Res 2022;6:260-6.
Abstract
Objectives:
The objectives of this study were to evaluate the accuracy of the diagnosis based on the phone forwarded pelvic radiographs for developmental dysplasia of the hip (DDH) and whether to accept decisions based on phone images.
Methods:
Two hundred and eight pelvic radiographs (416 hips) performed for DDH screening were evaluated by three orthopedic surgeons on picture archiving and communication system (PACS) and re-evaluated by the same surgeons after receiving them blindly on their phones through the WhatsApp application. Phone pictures were evaluated on both portrait and landscape viewing interfaces.
Results:
Nine ossification centers (2.9%) were detected on PACS but were not noticed when evaluated on the phone due to the lower phone image quality. All dislocated and dysplastic hips were correctly diagnosed by the phone. The phone overestimated the acetabular index by about two degrees, which explains why 4.8% and 7.5% of normal hips on PACS viewers were labeled dysplastic once evaluated on phone portrait and landscape viewers, respectively. However, landscape phone viewing and smaller phone screens were associated with a higher overestimation of the acetabular index.
Conclusion:
The phone is a valuable and safe tool for diagnosing DDH from pelvic radiographs. However, a precaution should be taken in borderline cases as the phone overestimated hip angles resulting in a misdiagnosis of normal hips as dysplastic. However, we do not recommend or encourage this practice because clinical evaluation is essential in any clinical decision-making.
Keywords
Acetabular index
Developmental dysplasia of the hip
Jordan
Pelvic radiograph
INTRODUCTION
Social media is a platform for interaction among individuals, allowing communication, sharing knowledge, and exchanging information. Social media messaging has evolved as an essential tool for communication among physicians and between patients and their physicians.[1-3] The revolution of smartphones and their wide availability and the ability to share images, media, and messages through social media messaging applications made communication easier and more effective.
Social media messaging usage in orthopedic consultation is widely adopted. It allows a rapid consultation between patients and physicians, and between junior and senior physicians. It also allows the sharing of radiographs and clinical pictures, and even CT and MRI videos. This allows straightforward and rapid decisions and is even utilized as a personal backup to review radiographs and patients’ histories for treatment planning.[4] However, there are ethical concerns about patients’ privacy.[5] Nevertheless, this has become a common practice, especially in the circumstances like COVID-19 pandemic restrictions, where patients could not reach health-care centers and, therefore, contacted their physicians for a new consultation and follow-up.
Screening for developmental dysplasia of the hip (DDH) is a controversial subject. The controversy includes whether to do a universal or selective screening as well as the screening modality.[6] Ultrasound is the preferred diagnostic modality before the ossification of the proximal femoral epiphysis. However, a pelvic radiograph is required when there is a significant ossification.[7,8] In Jordan, due to the inadequate availability of ultrasound machines in orthopedic clinics and the lack of professional training on its use, screening for DDH is done by early clinical examination followed by pelvic radiographs at the age of 3 months.
A pelvic radiograph for DDH might be shared for diagnosis or to seek another opinion. However, many social media applications, including WhatsApp, automatically compress photos and reduce their quality. Therefore, this study evaluates the accuracy of phone messaging forwarded pelvic radiographs for DDH diagnosis and whether to accept the decision based on them. In addition, to determine if the acetabular index angle can be estimated accurately based on phone images.
MATERIALS AND METHODS
In this prospective study, three orthopedic physicians radiologically evaluated infants who attended the orthopedic clinic for DDH screening and follow-up from April to November 2021. Sociodemographic history, risk factors, and associated conditions were obtained from infant families at the clinic. Hip radiograph parameters were measured by three orthopedic surgeons in picture archiving and communication system (PACS) and decision was documented.
Radiographs ID numbers were collected and a fourth surgeon used his phone to take the pictures from the PACS and sent them through the WhatsApp application to the same orthopedic surgeon who assessed pelvic radiographs to reanalyze them in their phones. However, images were obtained in ideal conditions by a physician who sits comfortably in front of a PACS screen leading to good quality images. In addition, images were picked from the PACS while the phone was in a vertical position and using a 6.43 inch phone screen size. Orthopedic physicians then reassessed the photos received on their phones and documented their decisions. However, phone photos were assessed twice through portrait and landscape interfaces. Then, data were combined according to the ID number for later analysis.
Hip radiographs described the hips as (a) normal, (b) dysplastic, or (c) dislocated. The hip ossification center was assessed as apparent or not apparent. In addition, the picture quality was labeled as accepted or inadequate.
Two hundred and eight infants and their pelvic radiographs (416 hips) were assessed. To standardize the analysis on phones, the Angelus® program version 4, an android store available application for angle measurement, was used to measure the acetabular index [Figure 1]. In addition, we standardized the parameters on PACS and phones to minimize intraobserver and interobserver variations. Although the diagnosis of DDH based on pelvic radiographs depends on many parameters and the qualitative assessment of the hip as dysplastic or dislocated is subjective, we considered the acetabular index a numerically measured parameter. However, the acetabular index angle changes with age, but we considered an angle of 30° as the normal upper limit for statistical analytical purposes.

- (a) Pelvic radiograph for developmental dysplasia of the hip screening. (b) The right hip acetabular index calculation on picture archiving and communication system. (c) Acetabular index on the portrait view. (d) Acetabular index on landscape view.
Statistical data analysis
The mean and standard deviation were used to describe the continuously measured variables, and the frequencies and percentages for describing the categorically measured variables. The histogram and the statistical Kolmogorov–Smirnov test were used to assess the statistical normality assumption of metric-measured outcomes. The paired samples t-test was used to assess the statistical significance of the mean difference in hip angles when compared between the PACS viewer and the phone’s two different views (portrait and landscape).
The data were transposed to accommodate the repeated measures of the hip conditions, and the measured angles were analyzed with the generalized linear mixed model (GLMM) analysis to assess the statistical significance of the mean differences in the measured hip angles under various viewing conditions and accounting for other relevant predictors in the analysis as covariates. The association between predictor variables and the mean hip measurements variation was expressed as a beta coefficient with its associated confidence interval.
The SPSS IBM V21 was used to analyze the data, and the alpha significance level was considered at 0.050.
RESULTS
The study included 208 infants (416 hips) and their pelvic radiographs. [Table 1] displays the sociodemographic characteristics and the risk factors of DDH in the study sample. Females represented the majority (62.5%). The mean age of infants at the study time was 5.43 months (±2.64), while the mean age at their first presentation was 4.28 months (±2.16).
| Frequency | Percentage | |
|---|---|---|
| Gender | ||
| Female | 130 | 62.5 |
| Male | 78 | 37.5 |
| Age ( months) at first presentation, mean (SD) | 4.28 (2.16) | |
| Age ( months) at the time of the study, mean (SD) | 5.43 (2.64) | |
| Risk factors | ||
| Firstborn | 58 | 27.9 |
| Family history of DDH | 58 | 27.9 |
| Breech position | 3 | 1.4 |
| Swaddling | 80 | 38.5 |
| Mode of delivery | ||
| Normal vaginal delivery | 159 | 76.4 |
| Cesarean section | 49 | 23.6 |
| Treatment modality | ||
| No pathology (no treatment) | 114 | 54.8 |
| Pavlik harness | 71 | 34.1 |
| Abduction splints | 23 | 11.1 |
DDH: Developmental dysplasia of the hip
[Table 2] demonstrates the descriptive analysis of the hip radiographs with various viewing methods. Only 6 (2.9%) images out of 208 were of insufficient quality on the phone. Nine (2.16%) ossification centers were apparent on PACS and, once evaluated on phones, were not detected, which is explained by the lower quality of phone images than PACS.
| Frequency | Percentage | |
|---|---|---|
| Ossification center on PACS | ||
| Not apparent | 206 | 49.5 |
| Apparent | 210 | 50.5 |
| Ossification center on phones | ||
| Not apparent | 215 | 51.7 |
| Apparent | 201 | 48.3 |
| Calculated acetabular index angle (degrees) on PACS, mean (SD) | 24.93 (5.22) | |
| Estimated acetabular index angle (degrees) on phone portrait view, mean (SD) | 26.51 (5.21) | |
| Estimated acetabular index angle (degrees) on phone landscape view, mean (SD) | 26.87 (5.01) | |
| Hip condition on PACS | ||
| Dislocated | 8 | 1.9 |
| Dysplastic | 90 | 21.6 |
| Normal | 318 | 76.4 |
| Hip condition on the phone portrait view | ||
| Dislocated | 8 | 1.9 |
| Dysplastic | 110 | 26.4 |
| Normal | 298 | 71.6 |
| Hip condition on phone landscape view | ||
| Dislocated | 8 | 1.9 |
| Dysplastic | 120 | 28.8 |
| Normal | 288 | 69.2 |
PACS: Picture archiving and communication system
When comparing the measured hip angles on the PACS and phones, it was noticed that the mean acetabular index on PACS was lower than the phone portrait and landscape measured angles [Figure 2]. The mean hips measured angle on PACS was 24.93° (±5.22) compared to 26.51° (±5.21) in the portrait view and 26.87° (±5.01) in the landscape view.
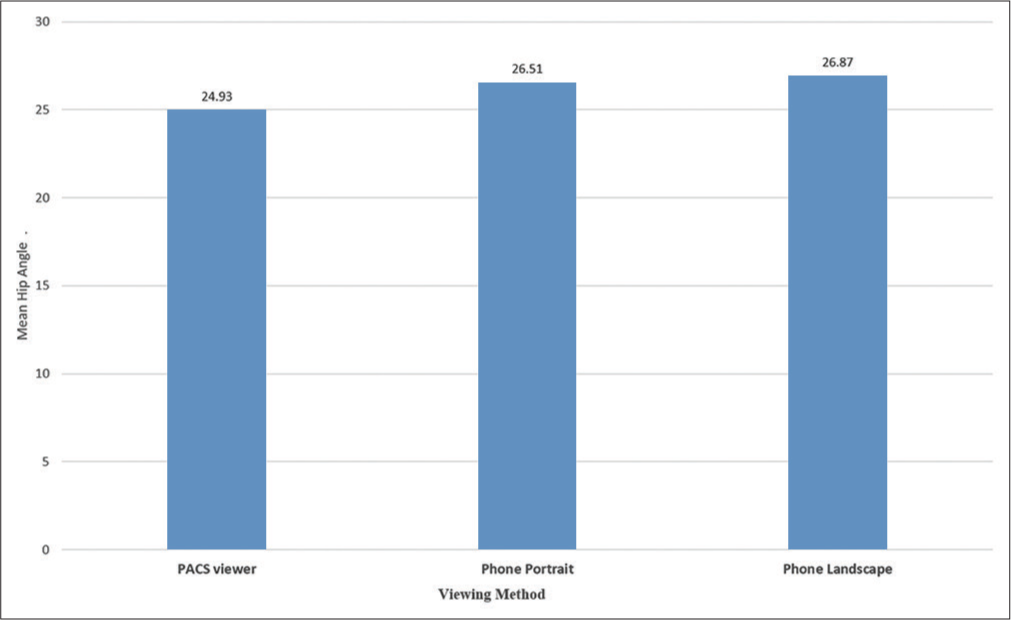
- The mean hip angles were evaluated with three different viewing methods.
[Table 3] demonstrates the contingency analysis, which compares the descriptive decision of hips between the PACS viewer and both phone interface viewing. Dislocated hip was constantly appearing on the phone regardless of the viewing method. Hip dislocations were identified in eight hips. Three patients were diagnosed with bilateral hip dislocation, one with an isolated right hip and another with isolated left hip dislocation. On the other hand, 20 hips were diagnosed as normal in PACS viewers and labeled as dysplastic in portrait phone viewing; the percentage of misdiagnosis in this category was 18.2%. Similarly, 30 hips (25%) were considered normal on PACS, labeled as dysplastic on landscape view.
| Hip diagnosis on PACS compared to phone portrait view. | |||
| PACS findings | Phone diagnosis on portrait view | ||
| Dislocated | Dysplastic | Normal | |
| Dislocated | 8 (100) | 0 | 0 |
| Dysplastic | 0 | 90 (81.8) | 0 |
| Normal | 0 | 20 (18.2) | 298 (100) |
| Hip diagnosis on PACS compared to phone landscape view. | |||
| PACS findings | Phone diagnosis on landscape view | ||
| Dislocated | Dysplastic | Normal | |
| Dislocated | 8 (100) | 0 | 0 |
| Dysplastic | 0 | 90 (75) | 0 |
| Normal | 0 | 30 (25) | 288 (100) |
Paired t-test was used to compare the measured hips angles on smartphones on both interfaces with the PACS as the standard reference [Table 4]. The findings demonstrated a higher angle on portrait view than PACS and an even higher on landscape viewing. On portrait view, the mean difference with the PACS was 1.57°(P < 0.001). Cohen’s D effect size statistic denoted that the amount of overestimation of the hips by the phone portrait view was medium suggestive of substantive overestimation of the hips angles when the portrait view was used to evaluate the radiographs images. Similarly, the paired samples t-test showed that the mean hips on the landscape viewing method had significantly exceeded that calculated with the PACS with 1.93° (P < 0.001). The effect size statistic denoted that the amount of overestimation of the hips angles with the smartphone landscape view was substantive. Cohen’s D = 0.758 approximated a large impact for the landscape views of the hip angles. Comparing the estimated hips mean angle with the phone portrait and landscape views, the paired t-test showed that the landscape estimated mean hips angle had also significantly exceeded that measured with the portrait layout by 0.359° (P < 0.001), with a small impact of the landscape over that estimated with the portrait on the hips angle, Cohen’s D = 0.299.
| Mean hips angle difference | Mean difference | 95% C. I. mean difference | Cohen’s D | P-value |
|---|---|---|---|---|
| PACS versus portrait | −1.57 | −1.917:−1.233 | 0.629 | <0.001 |
| PACS versus landscape | −1.93 | −2.279:−1.589 | 0.758 | <0.001 |
| Portrait versus landscape | −0.359 | −0.522:−0.195 | 0.299 | <0.001 |
PACS: Picture archiving and communication system
Phone images were assessed by the personal phones of three physicians; 44.7% of hip radiographs were assessed on a 6 inch screen phone, 23.6% of images were assessed on a 6.4 inch screen, and the remaining 31.7% on a 6.7 inch phone. To identify the difference of the screen size on angle analysis, the multivariate GLMM analysis was used with an identity link to regress the patients repeated hips angles measurements with the three methods (PACS, phone portrait, and phone landscape views). The data were first transposed from long to wide data using the data restructuring feature in the analysis program resulting in a data matrix equal to 416 hips * 3 repeated hip angle measures = 1248 data records [Table 5]. Measurement on phone portrait view resulted in a significant overestimation of the hip angles when compared with the PACS on average; the portrait phone view of the hip radiograph may be associated with 2.67° on average above that estimated by the PACS viewer (P < 0.001). Furthermore, measurement on the phone landscape interface resulted in an overestimation of the hips angle compared with the PACS estimate of the same image, beta coefficient = 2.50°, P < 0.001, by considering the other predictors and covariates in the analysis model as accounted.
| Model term | Beta coefficient | 95% confidence interval for beta | P-value | |
|---|---|---|---|---|
| Low bound | Upper bound | |||
| Intercept | 24.086 | 22.172 | 26 | <0.001 |
| Used viewing method=Phone portrait view | 2.673 | 2.271 | 3.256 | <0.001 |
| Used viewing method=Phone landscape view | 2.495 | 2.008 | 2.981 | <0.001 |
| Phone screen size=6.7 inch | 1.241 | −0.382 | 2.864 | 0.134 |
| Phone screen size=6.4 inch | −0.822 | −2.555 | 0.912 | 0.353 |
| Interaction (6.7 inch screen*portrait view) | −2.279 | −3.043 | −1.514 | <0.001 |
| Interaction (6.4 inch screen*portrait view) | −1.614 | −2.479 | −0.803 | <0.001 |
| Interaction (6.7 inch screen*landscape view) | −1.979 | −2.735 | −1.224 | <0.001 |
| Interaction (6.4 inch screen*landscape view) | 0.607 | −0.221 | 1.436 | 0.150 |
The interaction term between the screen size and the used layout of the screen (screen size * phone view), which was found to be statistically significantly correlated with the measured mean hips angle [Table 6]. The 6.7 inch screen smartphones when used with the landscape may result in significantly lower (−1.98° less) hips angle estimates compared to the 6 inch screen smartphones in landscape view (P < 0.001). The 6.4 inch smartphone screen resulted in no significantly different hip angle measures in landscape view compared to the 6.0 inch smartphone screen (P = 0.150). The 6.7 inch smartphone screen was associated with significantly lower (−2.28°) hips angle measurement when used in portrait view than the small 6.0 inch smartphone screen, also in portrait layout on average (P < 0.001). Not only so but also the 6.4 inch smartphone screen was associated with significantly lower (−1.61°) hips measurement in portrait view compared to the small 6.0 inch smartphone’s screen when used in portrait and paying attention that the same physician conducted all those measurements from PACS to smartphone two views for each patient.
| Smartphone screen size | Mean (SD) hips angle |
|---|---|
| 6.0 inch | 26.97 (±5.22) |
| 6.4 inch | 24.96 (±6.15) |
| 6.7 inch | 25.72 (±4.09) |
In summary, 20 (4.8%) normal hips were misclassified as dysplastic once evaluated on phone portrait view, and 30 (7.2%) normal hips were misdiagnosed as dysplastic when assessed on landscape view compared to the PACS view.
DISCUSSION
Because smartphones are commonly used as a consultation method for DDH by forwarding pelvic radiographs through social media applications, we conducted this study to verify the accuracy and safety of diagnosis based on phone images. However, good picture quality in the phone is mandatory to make a decision. However, in real conditions, some picked-up pictures from the screen have a light reflection or may be taken from printed radiographs or at an angle. Those factors diminish the picked-up picture quality, and the inadequate picture quality is expected to be higher in images shared in real conditions. In our study, images were obtained in ideal conditions by a physician who sits comfortably in front of a PACS screen, leading to good quality images. Nevertheless, 2.9% of the images were of low quality. The lower quality phone picked images obscured the ossification center in 9 hips (2.16%), which were detected on PACS viewer. The femur head ossification center appears between the age of 3 and 9 months.[9] Therefore, the high frequency of delayed ossification centers appearance is not necessarily pathological; it is secondary to the early presentation of the study sample from the age of 3 months. Nevertheless, nine ossification centers were apparent on PACS and not detected on phones, which is expected due to the lower quality of phone images than PACS.
The acetabular index is a valuable parameter used in the diagnosis of DDH. It represents the angle formed by the junction of Hilgenreiner’s and a line drawn along the acetabular surface. However, using the acetabular index is controversial, and the normal values are debatable. In 1938, Tchijine believed that a cup angle greater than 40° indicated the need for treatment. However, in 1958, Hass recommended that the angle should be <30°. There is still controversy over the angle in many recent studies. However, in normal newborns, the acetabular index averages 27.5°, 23.5° at 6 months, and 20° at 2 years. However, 30° is considered the upper limit of the normal range.[10-12]
In our study, we used the acetabular index as an objective measure for analysis purposes, and the use of the 30° angle is for ease of measurement only. Therefore, we believe that using this cutoff point does not affect the analysis, and the result we got from calculating the index on the phone and PACS is that the phone overestimates the angle compared to PACS, and this finding is reproduced independently of the cutoff point.
The images on PACS are calibrated; therefore, the acetabular index measurements on PACS are the standard. Phone pictures’ dimensions changed secondary to stretching or compression of the pictures; moreover, the dimension in portrait viewing is not identical to landscape viewing.
Therefore, this affects the measured acetabular index angles. However, mean acetabular indices of the hips measured in phone portrait mode were higher than those in PACS and further higher in landscape viewing measurements; this difference in both interface measurements might arise from the fact that the pictures were picked while a phone was in portrait view. The overestimation in phones ranged up to two degrees. It should be noted that phone overestimation led to the misdiagnosis of normal hips with borderline acetabular index angles as dysplastic, which resulted in 4.8% and 7.5% of false positives in portrait and landscape interface, respectively. Nevertheless, all dysplastic and dislocated hips were diagnosed correctly on the phone assessment.
In our analysis, the smaller phone screen size was generally associated with a more considerable overestimation of the hip angles than larger screen sizes; although this association is a non-linear correlation, it is an important factor to consider. However, this study did not rule out the sources of error from observing physicians themselves because the physicians were using their phones to assess the hips’ angles. Nevertheless, this is an important finding to highlight and consider when using the phone for decision-making.
Regardless of the fact that clinical history and examination are essential in diagnosing any pathology, including DDH. Nevertheless, pelvic radiographs can diagnose DDH precisely, especially in older infants. However, it is a common practice, at least in Jordan, to share pelvic radiographs through phone seeking consultation between patients and their physicians and between junior physicians and their seniors. Therefore, we conducted this study to determine the accuracy and safety of this method.
Limitations of the study
Although the images shared on the smartphones were taken by the person sitting in front of the PACS viewer, assuring a good quality of such images on phones. However, this is not the case for the pictures that are forwarded in reality, as they might be taken from variable distances and angles. In addition, some phone pictures are picked up from printed radiographs, which may be hazy or blurred; this adds to the difficulty of picture interpretation in real life. Therefore, we expect a higher frequency of unaccepted phone pictures, precluding proper picture assessment.
Three physicians assessed pelvic radiographs on their phones. Therefore, the finding related to phone screen size might be from interobserver variation rather than screen viewing size. To confirm the effect of phone size on measurement variation, it was better to include different phones sizes and tablets or even make the same physicians do the measurement on different phone sizes to eliminate the interobserver effect on acetabular index measurements, and it is still an important finding to be considered for future research. The images picked by phones from the PACS were obtained by a fourth person who used his phone, and the images were taken while his phone was in a portrait position; this raises the quires whether picking images while a phone was in a portrait position is different from picking it while it in landscape position. Moreover, even viewing the picture in a landscape is different if picked in a portrait or landscape phone position. The other query was whether picking images with one type of phone and sharing them with another type of phone differs from assessing pictures picked by the same type of phone.
Although the DDH decision based on pelvic radiographs depends on many parameters, this includes the qualitative assessment of the hip as normal, dysplastic, or dislocated. Moreover, the decision might sometimes be subjective. However, we usually consider all the parameters in assessing pelvic radiographs, and the acetabular index is just a numerically measured parameter for analytical purposes.
CONCLUSION
The phone is a valuable and safe tool for diagnosing DDH from pelvic radiographs. All dislocated and dysplastic hips were diagnosed correctly on the phone. However, when analyzed on the phone portrait and landscape, 4.8% and 7.5% of normal hips on PACS viewers were labeled dysplastic. The phone overestimated the acetabular index by around two degrees, so borderline normal hips on PACS were misdiagnosed as dysplastic on the phone. Overestimation is more marked on the landscape rather than portrait phone viewing. Therefore, a precaution should be considered at the borderline acetabular index cases. In addition, smaller screen sizes are associated with greater overestimating hip angles.
RECOMMENDATIONS
Although the phone is a safe and accurate tool in DDH diagnosis, we do not recommend or encourage this practice because clinical evaluation is essential in any clinical decision-making. Sharing radiographs if needed are better through emails to keep the picture quality and dimensions.
AUTHORS’ CONTRIBUTIONS
AA conceived and designed the study, conducted research, analyzed and interpreted data, and wrote the article’s initial and final drafts. NM, KB, and AAA provided research materials, collected and organized data, analyzed and interpreted data, and performed all statistical analyses. GA did all data entry and cleaning of the final data. Finally, all authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This study was approved by the Royal Medical Services Human Research Ethics Committee, number (13/2021) on December 27, 2021.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
References
- Social media for networking, professional development, and patient engagement. Am Soc Clin Oncol Educ Book. 2017;37:782-7.
- [CrossRef] [PubMed] [Google Scholar]
- Use of social network sites for communication among health professionals: Systematic review. J Med Internet Res. 2018;20:e117.
- [CrossRef] [PubMed] [Google Scholar]
- Remote patient monitoring in spine surgery. J Musculoskelet Surg Res. 2022;6:160-6.
- [CrossRef] [Google Scholar]
- Telemedicine in hand and upper-extremity surgery. J Hand Surg Am. 2020;45:239-42.
- [CrossRef] [PubMed] [Google Scholar]
- Ethical implications of digital images for teaching and learning purposes: An integrative review. J Multidiscip Healthc. 2015;8:299-305.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and referral for developmental dysplasia of the hip in infants. Pediatrics. 2016;138:e20163107.
- [CrossRef] [PubMed] [Google Scholar]
- Cochrane review: Screening programmes for developmental dysplasia of the hip in newborn infants. Evid Based Child Health. 2013;8:11-54.
- [CrossRef] [PubMed] [Google Scholar]
- Preventive health care, 2001 update: Screening and management of developmental dysplasia of the hip in newborns. CMAJ. 2001;164:1669-77.
- [Google Scholar]
- New radiographic standards for age at appearance of the ossification center of the femoral head in Japanese: Appearance at =12 months of age is normal in Japanese infants. J Orthop Sci. 2019;24:166-9.
- [CrossRef] [PubMed] [Google Scholar]
- The acetabular index: A critical review. J Bone Joint Surg Br. 1959;41:702-10.
- [CrossRef] [Google Scholar]
- Acetabular index values in healthy Turkish children between 6 months and 8 years of age: A cross-sectional radiological study. Acta Orthop Traumatol Turc. 2013;47:38-42.
- [CrossRef] [PubMed] [Google Scholar]







