Translate this page into:
Predictors of screw cutout in the surgical fixation of peritrochanteric hip fractures: A retrospective cohort study
*Corresponding author: Loay A. Salman, Department of Orthopedics, Hamad Medical Corporation, Doha, Qatar. loayasalman@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aboulebda M, Salman LA, Hammad M, Foodool MA, Kong G, Abunimer AM, et al. Predictors of screw cutout in the surgical fixation of peritrochanteric hip fractures: A retrospective cohort study. J Musculoskelet Surg Res, 2023;7:164-9.
Abstract
Objectives:
This study aimed to evaluate the impact of the tip-apex distance (TAD) and other reported risk factors on the screw cutout rate.
Methods:
This study retrospectively reviewed electronic medical records from January 2016 to December 2018 to analyze the relationship between TAD and implant cutout failure rate in patients with peritrochanteric (PT) fractures who underwent cephalomedullary nail (CMN) or dynamic hip screw (DHS) fixation. Secondary factors analyzed included age, body mass index (BMI), fracture stability, posterolateral fragment presence, post-operative radiographic reduction, implant type, and screw position.
Results:
A total of 68 patients (40 DHS, 28 CMN cases) were included in the study, with a mean age of 64 ± 20 years and a BMI of 25.5. Most of the included patients (65%; 44) were males. An overall cohort screw cutout rate of 7.3% (5 cases) was observed. The patient’s age, BMI, fracture classification (stability), implant type, and the level of the operating surgeon did not influence the screw cutout rate (P = NS). However, a TAD ≥25 mm (P = 0.02), lag screw position (P = 0.03), and fracture reduction in anteroposterior (P = 0.02) and lateral views (P = 0.024) showed statistically significant results.
Conclusion:
This study demonstrated that a TAD of ≥25 mm, lag screws malposition, and inappropriately reduced fracture in post-operative radiographs are significant risk factors for screw cutout in DHS and CMN fixation of PT fractures.
Keywords
Cephalomedullary nail
Dynamic Screw cutout
Hip fractures
Peritrochanteric
Tip apex distance
INTRODUCTION
Peritrochanteric (PT) femur fractures can be associated with debilitating outcomes and reduced disability-adjusted life years.[1,2] Thus, posing a substantial socioeconomic challenge,[1-3] PT fractures encompass a group of fractures between the femur neck and subtrochanteric region and contribute to up to 50% of adult hip fractures. These fractures are often a result of low energy (e.g., falls) in elderly patients or high-energy trauma like road traffic accidents in younger populations.
Surgical treatment is the gold standard in managing this kind of injury to restore baseline pre-injury mobility and functionality, pain control, and avoid immobilization morbidity. Various surgical fixation methods exist based on the fracture pattern and stability, including dynamic hip screw (DHS) and cephalomedullary nail (CMN). CMN, such as Gamma nails, are usually used to fix unstable PT hip fractures (AO classification A2 and A3) due to the biomechanical advantages over plate fixation. However, stable PT fractures (AO classification A1) can be fixed with either implant.
Screw cutout or failure is one of the most serious complications associated with internal fixation of PT fractures, with a prevalence of around 1.9–3.2%.[4-6] It is defined as varus collapse of the femoral neck-shaft angle (<130), which leads to screw extrusion or cutout from the femoral head.[4] This complication often requires to be addressed surgically. Thus, identifying the predisposing risk factors helps prevent screw cutouts and reoperation following internal fixation of PT fractures.
Numerous variables have been described in the literature as predictors of screw cutout following fixation of such fractures.[7,8] These include (1) a tip apex distance (TAD) ≥T5 mm,[4,9] (2) unstable fracture patterns as per Orthopaedic Trauma Association (OTA)/AO classification (A2.2 or A2.3),[10] (3) the presence of a posterolateral fragment (Jensen 3 or 4),[11] (4) types of reduction pattern on anteroposterior (AP) (medial) and lateral (LAT) (intramedullary) radiographic images, and[12] (5) unstable screw position (other than central-central or central-inferior).[9,13]
The TAD is the total distance from the tip of the screw to the apex of the femoral head on both AP and LAT radiographs measured in millimeters after adjusting for magnification [Figure 1].[6]
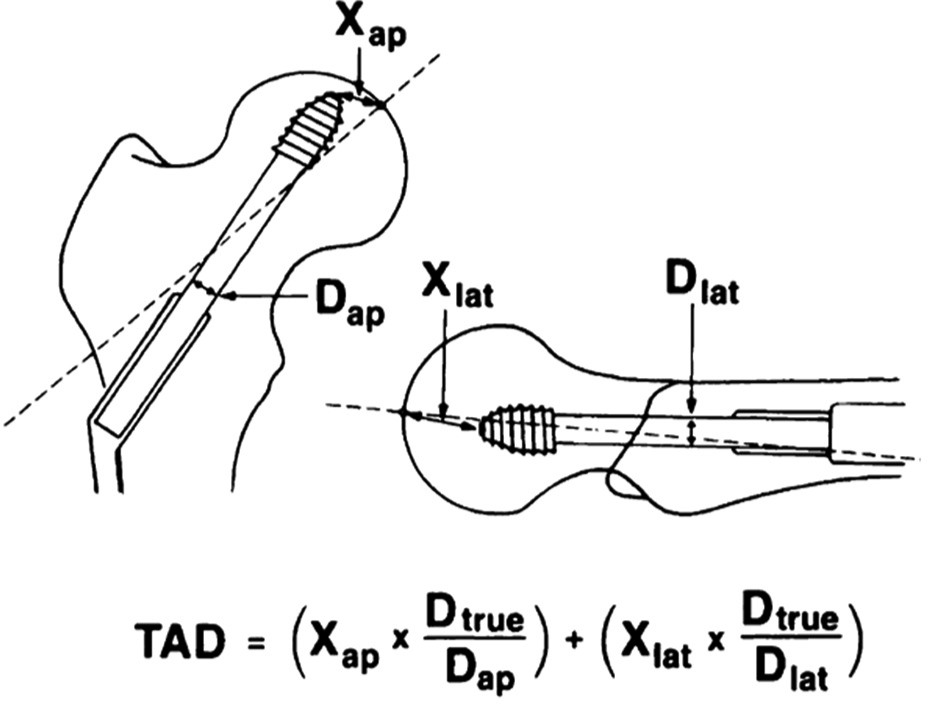
- The measurement of tip apex distance (TAD) is illustrated in a line drawing, with the use of Dtrue to control for magnification. Dtrue is the known diameter of the lag screw, while Dap and Dlat represent the measured diameter of the screw on anteroposterior and lateral radiographs, respectively. Xap and Xlat are the distances from the screw tip to the center of the femoral head on the corresponding radiographs. This illustration is adapted from a study by Baumgaertner et al. (1995) on the predictive value of TAD in the failure of fixation of peri-trochanteric fractures of the hip.
To the best of our knowledge, this is the first national study to investigate the value of these risk factors as predictors of screw cutout in both DHS and CMN implant fixation of PT fractures. Therefore, this study aimed to evaluate the impact of the TAD and other reported factors as predictors of the screw cutout after internal fixation of PT fractures.
MATERIALS AND METHODS
Study design and setting
This retrospective and cohort study was conducted at a Level I trauma center accredited by the Joint Commission International and Accreditation Council of Graduate Medical Education-International. The Institutional Medical Research Centre approved this study, which adhered to the STROCSS guidelines.[14]
Data source and collection
We searched our institution’s electronic medical records database from January 2016 to December 2018 using keywords such as “Peritrochanteric hip fractures,” “Cephalomedullary nail ” “DHS,” and their variations to identify all potential cases. Two authors independently performed the search and data collection. In addition, baseline variables, including age, gender, body mass index (BMI), comorbidities, fracture classification, implant type, TAD measurement, lag screw position, post-operative radiographic reduction on AP and LAT views, operating surgeon level, follow-up duration, and screw cutout rate, were collected.
The primary predictor variable for this cohort was the measurement of TAD in the early post-operative radiographs by which patients were grouped into two groups TAD <25 or ≥25 mm. Other predictor variables included the OTA/ AO classification, types of reduction patterns on AP and LAT radiographic images, lag screw position, age, and implant type.
The primary outcome was to assess any relationship between the TAD and the implant cutout failure rate in PT fractures treated by CMN or DHS. Secondary outcomes were to evaluate the impact of other risk factors on implant failure (i.e., fracture classification, quality of reduction, lag screw position, or age).
The post-operative quality of fracture reduction was described as a good, medial, or intramedullary pattern, according to the definitions proposed by Baumgaertner et al.[4] and Ito et al.[12] A good reduction was classified as normal or slight valgus alignment on the AP radiograph, <20° of angulation on the LAT radiograph, and 4 mm of displacement of any fragment. A medial reduction pattern in which the proximal fragment lay inward from the anatomical position in the post-operative AP radiograph. In contrast, an intramedullary reduction pattern was defined when the anterior cortex of the proximal part of the femur was located at the rear of the anterior cortex of the distal fragment in the LAT radiograph.
Eligibility criteria
All adult patients (≥18 years) with acute PT fracture who underwent DHS or CMN fixation between 2016 and 2018 with at least 3 months of follow-up were included in the study. Patients with inadequate post-operative radiographs and ipsilateral femur shaft fractures were excluded from the study. [Figure 2] shows the complete inclusion and exclusion process.
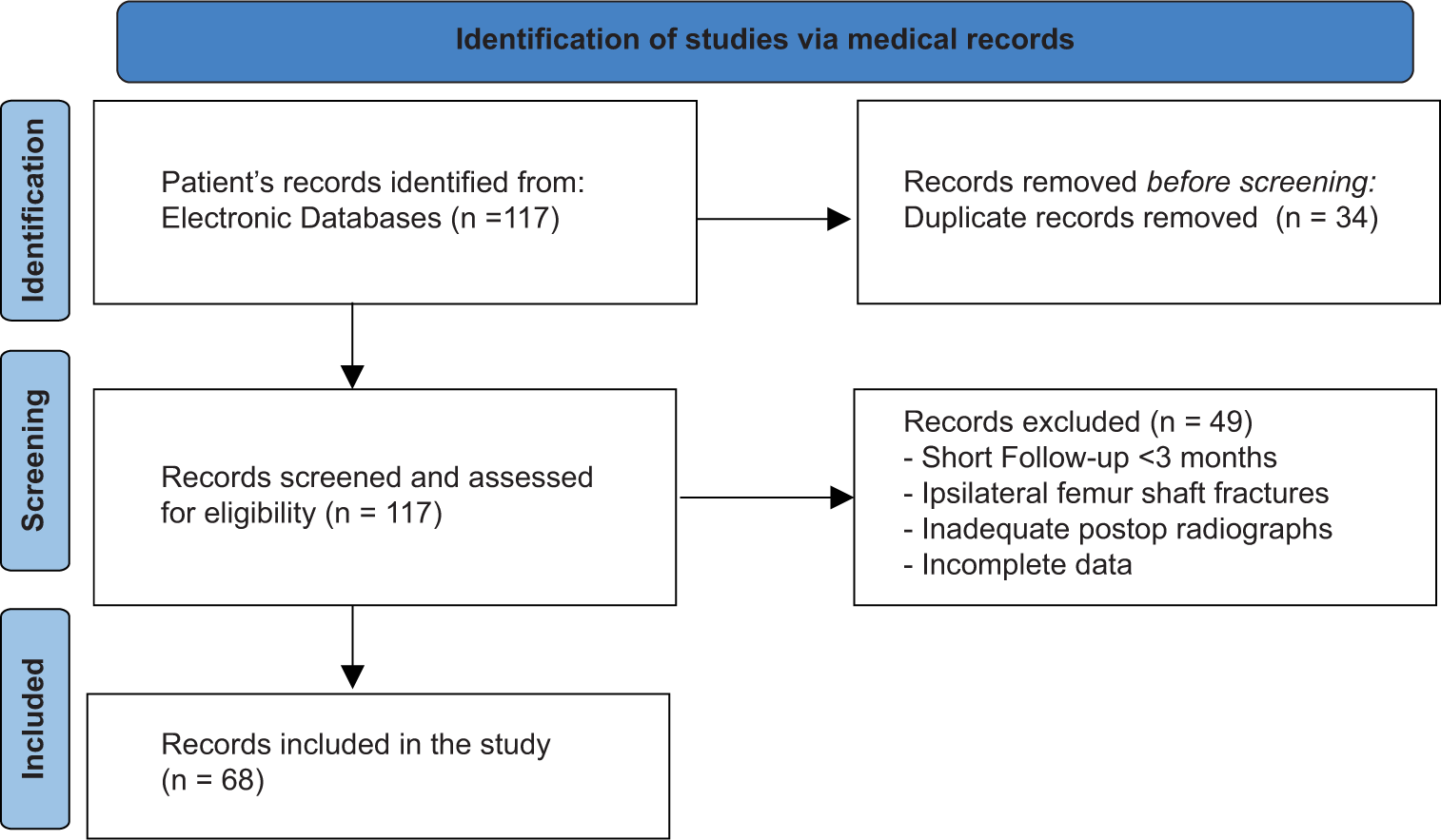
- Eligibility criteria.
Statistical analysis
Stata/IC 15.1 statistical package[15] was utilized for the statistical analysis. Differences in ordinal variables between TAD <25 and ≥25 mm were compared using Kruskal– Wallis’s test, while Mann–Whitney U-test and Fisher’s exact test were used for continuous and dichotomous outcomes, respectively. Continuous variables were presented as median with standard deviation or 95% confidence intervals, while dichotomous variables were presented as proportions. P ≤ 0.05 was considered statistically significant in all tests. No power analysis was conducted, as all patients meeting the inclusion criteria were included in this study.
RESULTS
A total of 117 cases of patients with PT hip fractures who underwent surgical fixation by either DHS or CMN were identified retrospectively. Sixty-eight (40 DHS cases and 28 CMN cases) patients met the inclusion criteria and were included in the final analysis [Table 1]. The mean age was 64 ± 20 years, with an average BMI of 25.5 and a minimum 3-month follow-up period. Patients were primarily males, 65% (44), and 35% (24) females.
| Variable | TAD value | |
|---|---|---|
| <25 (%) | ≥25 (%) | |
| Implant (% of total) | ||
| DHS | 25 (65.8) | 15 (50.0) |
| CMN (Gamma nail) | 13 (34.2) | 15 (50.0) |
| Age (years), mean (±SD) | 65±20 | 63±20 |
| Body mass index | 26±4 | 25±5 |
| Gender | ||
| Female | 17 (44.7) | 7 (23.3) |
| Male | 21 (55.3) | 23 (76.7) |
| Fracture classification | ||
| Stable | 18 (48.6) | 16 (53.3) |
| Unstable | 19 (51.4) | 14 (46.7) |
| Surgeon | ||
| Trainee | 25 (65.8) | 17 (56.7) |
| Attending | 13 (34.2) | 13 (43.3) |
| Reduction AP view | ||
| LAT type | 4 (10.5) | 1 (3.3) |
| Medial type | 11 (28.9) | 3 (10.0) |
| Good | 23 (60.5) | 26 (86.7) |
| Reduction LAT view | ||
| IM type | 9 (23.7) | 1 (3.3) |
| Good | 29 (76.3) | 29 (96.7) |
| Position of lag screw | ||
| Centro-anterior | 2 (7) | 2 (8) |
| Central-central | 14 (48) | 12 (48) |
| Centro-posterior | 1 (3.5) | 1 (4) |
| Antero-inferior | 1 (3.5) | 6 (24) |
| Centro-inferior | 11 (38) | 3 (12) |
| Postero-inferior | 0 | 1 (4) |
TAD: Tip apex distance, DHS: Dynamic hip screw, CMN: Cephalomedullary nail, AP: Anteroposterior, LAT: Lateral, SD: Standard deviation
Results were subclassified based on the TAD criterion into two main groups: Group A, where TAD is <25 mm, and Group B, where TAD equals or exceeds 25 mm. The mean age was 65 ± 20 years in Group A and 63 ± 20 years in Group B. The average BMI was 26 ± 4 in Group A and 25 ± 5 in Group B. Twenty-one patients (55.3%) and 23 (76.7%) were males in Groups A and B, respectively.
Regarding fracture stability, 51.4% (19) and 46.4% (14) cases were unstable in Groups A and B, respectively. Most cases were operated by trainees surgeon, with 65.8% (25) in Group A compared to 56.7% (17) in Group B. “Good” appropriate fracture reduction was achieved on postoperative AP and LAT radiographs across both groups. In Group A, the lag screw position was observed to be consistently centralized (central-central or central-inferior) in 86% of the cases. In Group B, central placement of the lag screw was found in approximately 72% of the cases, with 28% exhibiting screw malposition. The detailed analysis is shown in [Table 1].
Five cases (7.35%) of screw cutouts were observed in this cohort study; four of which [Cases 1–4 in Table 2] were fixed with DHS and one [Case 5 in Table 2] by CMN. A sub-analysis assessed the relationship between these predicting factors (TAD, age, BMI, fracture classification, lag screw position pattern of fracture reduction on AP and LAT views, implant type, and performing surgeon level) and their impact on screw cutout. It was shown that age, BMI, fracture classification, and the level of performing surgeon were statistically insignificant (P = 0.617, P = 0.535, P = 0.707 and P = 0.445, respectively) in predicting screw cutout.
| Cases | Implant | Factors | |||||||
|---|---|---|---|---|---|---|---|---|---|
| TAD | Age | BMI | Fracture classification | Lag screw position | Reduction AP view | Reduction LAT view | Surgeon | ||
| Case 1 | DHS | 17 | 85 | 23 | Stable | Centro-anterior | Appropriate | Appropriate | Trainee |
| Case 2 | DHS | 26 | 77 | 19 | Unstable | Centro-posterior | Medial reduction | Intramedullary reduction | Trainee |
| Case 3 | DHS | 31 | 74 | 28 | Stable | Central | Appropriate | Appropriate | Attending |
| Case 4 | DHS | 41 | 72 | 33 | Stable | Centro-anterior | Appropriate | Appropriate | Trainee |
| Case 5 | CMN | 47 | 60 | 26 | Unstable | Inferio-anterior | Medial reduction | Appropriate | Attending |
TAD: Tip apex distance, DHS: Dynamic hip screw, CMN: Cephalomedullary nail, BMI: Body mass index, AP: Anteroposterior, LAT: Lateral
Furthermore, the proportion of failed cases in CMN use was 3.6%, and the proportion in DHS device use was 10%. A two-sample proportion test found no statistically significant difference in the proportion of failed cases between CMN use and DHS device use (P = 0.157), indicating that both treatment modalities have similar failure rates [Table 2].
In contrast, the measurement of TAD (in 80%, the TAD was more than 25 mm), lag screw malposition, and the fracture malreduction in AP (40%) and LAT views (20%) radiographs were statistically significant factors (P = 0.02, P = 0.03, P = 0.02 for AP and P = 0.024 LAT, respectively). A sub-analysis of screw cutout cases is summarized in [Table 2].
DISCUSSION
There has been considerable debate regarding the optimal implant that ensures anatomical reduction and the best clinical outcome. DHS and CMN (Gamma nails) are the most representative extramedullary and intramedullary fixation devices.
The most important finding of the present study is that the TAD of equal or more than 25 mm, pattern of the lag screw position, and fracture reduction on AP and LAT views were statistically significant contributing factors for screw cutout. However, the age, BMI, fracture classification, and level of performing surgeons were statistically insignificant in predicting screw cutout.
In line with other studies, our present study shed light on multiple factors that affect the TAD, resulting in fixation failure. Various factors have been associated with implant failure in PT hip fractures, including patient age, bone quality, fracture pattern, fracture reduction stability, implant angle, and lag screw position within the femoral head.[16] However, there is currently no consensus on each factor’s interrelationships or relative importance. Accurate screw placement has been widely recognized as crucial, but methods for evaluating screw position have proven to be cumbersome and of limited predictive value in clinical settings. In this cohort, most of the screw cutout cases (80%) were fixed with DHS. In contrast to our findings, a meta-analysis conducted by Matre et al.[8] found no significant difference in fixation failure (cutting-out or non-union) between Gamma nails and proximal femoral nails anti-rotation (PFNA) or DHS. However, a significantly lower risk of fixation failure was found in the PFNA group compared to DHS. Moreover, implant cutout and other complications were significantly associated with higher TAD, poor reduction, or reduction in varus and that these factors were independent of the implant type.[8] Thus, achieving surgical perfection is paramount to selecting the implant to address this issue. In addition, using a CMN may lead to a reduced incidence of medialization >5 mm due to its resistance to excessive sliding along the axis of the lag screw.
Among the aforementioned factors, a retrospective analysis conducted by Fujii et al.[17] confirmed that only a TAD of >20 mm was associated with screw cutout after internal fixation of intertrochanteric fractures with PFNA systems.
Due to the retrospective nature of the study, it is important to acknowledge several limitations, such as the presence of selection bias and the absence of randomized comparative groups. However, a sub-analysis based on the TAD within the same cohort was conducted to mitigate these limitations. In addition, one of the setbacks of this study was lacking power analysis and the small sample size due to the limited number of cases meeting the inclusion criteria. Future prospective studies, ideally multicentric, are needed to adjust for these drawbacks.
CONCLUSION
This study demonstrated that a TAD of ≥25 mm, lag screws malposition, and inappropriately reduced fracture in post-operative radiographs are statistically significant risk factors for screw cutout in DHS and CMN fixation of PT fractures. However, this finding should be applied in context, given.
AUTHOR CONTRIBUTIONS
All authors contributed to the study’s conception and design. Material preparation, literature review, data collection, and quality assessment were performed by MA, LAS, and AMA. Statistical analysis was performed by AMA and LAS. The first draft of the manuscript was written by MA, MH, and GK, and all authors commented on previous versions of the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Medical Research Centre at Hamad medical corporation approved this retrospective study on the March 23, 2020, with the reference number MRC–01–19–267 and can provide access to protocol on direct request.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
DECLARATION OF PATIENTS CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726-33.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of hip fracture using disability-adjusted life-years: A pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health. 2017;2:e239-46.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364-70.
- [CrossRef] [PubMed] [Google Scholar]
- The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058-64.
- [CrossRef] [PubMed] [Google Scholar]
- 3,066 consecutive Gamma Nails. 12 years experience at a single centre. BMC Musculoskelet Disord. 2010;11:133.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical outcomes with three different intramedullary nailing devices in the treatment of unstable trochanteric fractures. Ulus Travma Acil Cerrahi Derg. 2015;21:469-76.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Joint Surg Am. 2012;94:1266-72.
- [CrossRef] [PubMed] [Google Scholar]
- TRIGEN INTERTAN intramedullary nail versus sliding hip screw: A prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am. 2013;95:200-8.
- [CrossRef] [PubMed] [Google Scholar]
- Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013;14:1.
- [CrossRef] [PubMed] [Google Scholar]
- Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1-133.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of trochanteric fractures. Acta Orthop Scand. 1980;51:803-10.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of excessive postoperative sliding of the short femoral nail in femoral trochanteric fractures. Arch Orthop Trauma Surg. 2015;135:651-7.
- [CrossRef] [PubMed] [Google Scholar]
- A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41A:1399-408.
- [CrossRef] [Google Scholar]
- Strocss 2021: Strengthening the Reporting of cohort, cross-sectional and case-control studies in Surgery. Int J Surg. 2021;96:106165.
- [CrossRef] [PubMed] [Google Scholar]
- Stata Statistical Software: Release 15.1 Texas, College Station, TX: StataCorp LLC; 2017.
- [Google Scholar]
- Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79:969-71.
- [CrossRef] [Google Scholar]
- Tip-apex distance is most important of six predictors of screw cutout after internal fixation of intertrochanteric fractures in women. JB JS Open Access. 2017;2:e0022.
- [CrossRef] [PubMed] [Google Scholar]







