Translate this page into:
A systematic review and meta-analysis on the impact of nail length in treating intertrochanteric fractures
*Corresponding author: Ghalib Ahmed, MBChb. FRCS. (Trauma and Orth), Department of Orthopedic Surgery, Hamad Medical Corporation, Doha, Qatar. gahmed@hamad.qa
-
Received: ,
Accepted: ,
How to cite this article: Hantouly AT, Alzobi O, Toubasi AA, Kayali H, Salman LA, Derbas J, et al. A systematic review and meta-analysis on the impact of nail length in treating intertrochanteric fractures. J Musculoskelet Surg Res, 2023;7:241-51.
Abstract
The management of intertrochanteric hip fractures remains a subject of ongoing debate, particularly regarding the ideal nail length for treatment. To address this, a systematic review and meta-analysis, based on randomized controlled trials (RCTs), were conducted to assess the outcomes associated with using short and long nails to fix intertrochanteric femur fractures. Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines for comprehensive reporting, a thorough search was conducted across four databases (Cochrane, Google Scholar, Web of Science, and PubMed) from inception until March 07, 2022. The study encompassed all RCTs comparing the outcomes of short and long nail fixation for intertrochanteric hip fractures. A total of 620 patients with intertrochanteric fractures from six RCTs were included in this analysis. Short nails were used in 50.3% of the patients (312 out of 620). The utilization of short nails was significantly associated with a reduction in operative time (weighted mean difference [WMD] = −20.33; 95% confidence interval [CI]: −29.90–−10.76) and decreased blood loss (WMD = −106.31; 95% CI: −155.43–−57.19). However, no substantial differences were observed between the two types of implants in terms of length of hospital stay, Harris hip score, reoperation rate, complication rate, and 1-year mortality rate. The length of nails used to treat intertrochanteric hip fractures does not have a notable impact on factors such as functional recovery, blood transfusion frequency, reoperation likelihood, complications, or 1-year mortality rates. Nonetheless, when comparing the fixation of intertrochanteric fractures, it is worth noting that short nails result in shorter surgery duration and reduced blood loss compared to long nails.
Keywords
Hip fractures
Proximal femur fractures
Fracture fixation
Intertrochanteric
Intramedullary
Cephalomedullary
Peritrochanteric
INTRODUCTION
Hip fractures are common injuries that can cause severe debilitation. Hip fractures are projected to increase twofold, reaching 500,000 cases/year in the United States alone over the next two decades.[1] This rise can be linked to advancements in life expectancy and higher levels of physical activity among the elderly population.[1,2] Roughly, one out of every three women and about 8% of men are expected to experience a hip fracture at some points in their lives.[3] With such high prevalence, in addition to the high morbidity and mortality rates of such injuries, these fractures impose an enormous burden on public health systems.[4,5] Hip fracture care was ranked among the most expensive diagnoses to treat in 2011 in The United States of America, with estimated annual costs of 15 billion US dollars.[5]
Intertrochanteric fractures accounted for 50% of all hip fractures in the old-age group.[5-7] These fractures can be fixed using different devices, including cephalomedulary nails (CMNs). CMNs are available in various designs and lengths, which have undergone several modifications to duplicate the femur’s anatomic characteristics. The theoretical advantages of both lengths are still debatable. Short nails offer lower rates of blood loss and shorter operative time. However, long nails provide full femur-length protection.[8-10]
Nevertheless, there remains a lack of agreement regarding the potential impact of nail length on outcomes, particularly for unstable fractures. This uncertainty is evident in the field, as surgeons employ CMNs of different lengths (short and long) without a unified body of evidence demonstrating any clear superiority. As a result, this research was undertaken to investigate the consequences of employing short and long CMNs for intertrochanteric hip fractures. Our hypothesis posited that no noteworthy disparity in functional outcomes would emerge between the two groups. However, longer surgical durations and heightened blood loss might be observed with the application of longer nails.[11-16]
MATERIALS AND METHODS
Study registration and reporting protocol
This systematic review and meta-analysis were formally registered on PROSPERO under the registration number CRD42022378375. The study adhered to the rigorous reporting framework of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.[17] Moreover, the review methods were predefined and established before the commencement of the review in accordance with the recommendations outlined in the AMSTAR-2 guidelines. This robust methodology ensures the reliability and validity of the study’s findings.
Search strategies
Following the PRISMA guidelines, a comprehensive search was conducted across four databases: PubMed, Google Scholar, Web of Science, and Cochrane, spanning from their inception up to March 07, 2022. The objective of the search was to identify all relevant randomized controlled trials (RCTs) that compared the utilization of short and long nails in the context of intertrochanteric femur fractures. Including RCTs was prioritized to ensure the incorporation of the most robust level of evidence.
The following keywords were used: (intramedullary OR cephalomedullary) AND nail AND (hip OR intertroch* OR peritroch*) AND fracture AND randomized AND short AND long.
The comprehensive search for eligible studies extended to the references of the included studies. Two independent reviewers carried out initial screening based on titles and abstracts. Studies that met the predefined eligibility criteria then underwent a meticulous full-text review. Furthermore, to ensure the inclusion of all relevant studies, the references of these eligible articles were scrutinized, demonstrating a rigorous approach to study selection and inclusion.
In case of any disparities between the reviewers, a consultation with a senior researcher was undertaken to reach a consensus and resolve disagreements.
Eligibility criteria
Inclusion criteria
Only RCTs that directly compared the use of short and long nails for fixing intertrochanteric fractures were considered eligible for inclusion. Moreover, the selection was limited to articles that were published in English and accessible for review.
Exclusion criteria
Studies that used implants other than nails were excluded from the study. Technical studies, cadaveric studies, biomechanical studies, pathological fractures, and single-armed studies were also excluded, which did not report the outcomes regarding using short and long nails.
Outcome
The outcome measures of interest encompassed several key factors, including blood loss, blood transfusion requirements, operative duration, length of hospital stay, functional assessment using the Harris hip score (HHS), occurrence of complications, reoperation frequency, and 1-year mortality rates.
Data collection process and data items
The following data items were collected: studies characteristics, patients’ demographics, fracture classification, operative time, tip apex distance (TAD), blood loss, type of implant used, length of stay, functional outcome using HHS, complications, reoperation, and 1-year mortality.
Risk of bias in individual studies
The qualitative analysis was conducted using the revised Cochrane risk-of-bias tool for randomized trials (RoB-2).[18] Two reviewers used this tool independently, and any discrepancy was discussed with the senior author to arrive at a consensus.
Statistical analysis
The mean and standard deviation were the primary statistical parameters used in the analysis of continuous variables. In cases where median and interquartile ranges were provided, they were transformed into mean and standard deviation using the formula developed by Wan et al [19]
The effect size for continuous variables was quantified as the weighted mean difference (WMD), along with its associated 95% confidence intervals (95% CIs).
The effect size was presented as the relative risk (RR) for binary variables, accompanied by its corresponding 95% CIs.
Both the Cochrane Q statistic and the I2 statistic were employed to assess heterogeneity among the included studies. A random-effect model was utilized to consolidate the study results if the I2 value exceeded 50%, indicating substantial heterogeneity. Conversely, a fixed-effect model was applied when the I2 value was below 50%.
The analysis was performed using Meta XL, version 5.3, a software developed by EpiGear International in Queensland, Australia, which is specifically designed for conducting meta-analyses.
RESULTS
Study selection
The initial search yielded a total of 376 articles, out of which 61 were identified as duplicates. Following screening titles and abstracts, 278 articles were excluded based on predetermined criteria. The full-text versions of the remaining 37 articles were then carefully reviewed to determine their eligibility according to the predefined inclusion criteria. Ultimately, six articles met the criteria and were included in the meta-analysis. A visual representation of this process can be seen in Figure 1, as presented in the PRISMA flowchart.
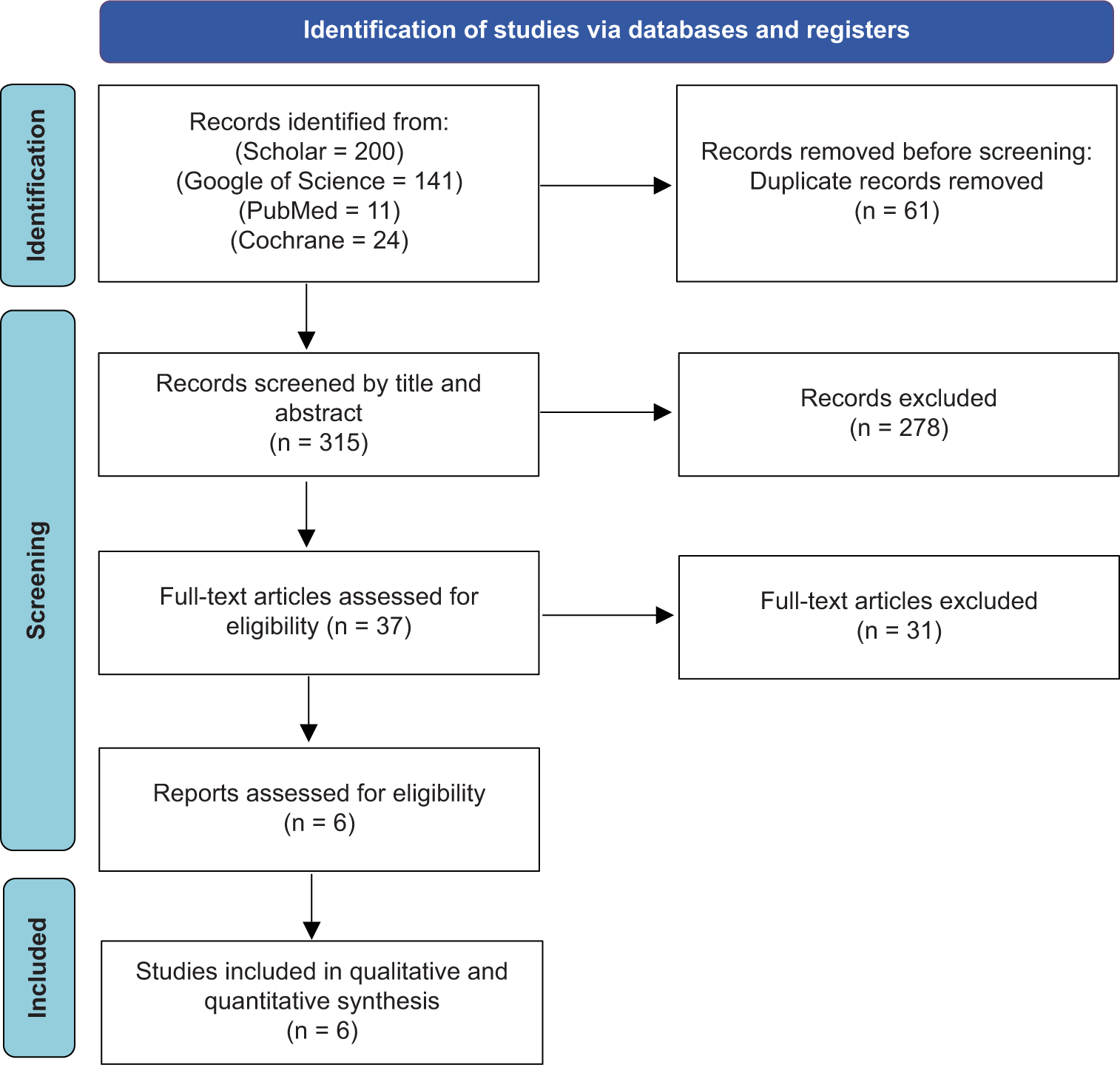
- Search strategy flowchart.
The characteristics of the included studies
The total number of patients included in this study was 620 patients pooled from six RCTs. The total number of patients who underwent fixation using short nails was 312, 21.7% of whom were males. On the other hand, 308 patients underwent fixation using long nails, 27.6% of whom were males. The mean age for patients who underwent short and long nail fixation was 79.76 ± 8.57 and 79.36 ± 9.03, respectively. In addition, the follow-up duration in the included studies varied from 10.93 months to 24 months. Table 1 provides a summary of the key characteristics of the studies that were included in this analysis.
| Study | Shannon et al., 2019[11] | Dragosloveanu et al., 2021[12] | Sahu and Pandey, 2020[13] | Parker and Cawley, 2020[14] | Galanopoulos et al., 2018[15] | Okcu et al., 2013[16] |
|---|---|---|---|---|---|---|
| Country | United States of America | Romania | India | United Kingdom | Greece | Turkey |
| Short nail group (male/female) | 80 (5/75) | 26 (14/12) | 45 (15/30) | 121 (30/90) | 25 | 15 (4/11) |
| Long nail group (male/female) | 88 (16/72) | 27 (13/14) | 42 (15/27) | 108 (37/71) | 25 | 18 (4/14) |
| Age (Short vs. Long) |
82 (79–84) vs. 79 (76–82) |
78.65±4.84 vs. 78.07±5.03 |
75.2±8.3 vs. 77.3±9.8 |
83.7 (47–103) vs. 81.8 (32–102) |
81 (74–92) vs. 79 (74–93) |
78 (67–95) vs. 81 (73–89) |
| Classification (short nail group) | A1: 13 A2: 61 A3: 6 |
AO31-A2: 21 AO31-A3: 5 |
31-A1: 15 31-A2: 24 31-A3: 6 |
A1: 31 A2: 90 |
- | - |
| Classification (long nail group) | A1: 12 A2: 67 A3: 9 |
AO31-A2: 21 AO31-A3: 6 |
31-A1: 12 31-A2: 21 31-A3: 9 |
A1: 28 A2: 80 |
- | - |
| Implant used (Short vs. Long) |
DePuy Synthes TFN-A nail + Stryker Gamma 3 + Biomet Affixus vs. DePuy Synthes TFN-A nail + Stryker Gamma 3 + Biomet Affixus |
Standard 180-mm Stryker Gamma3 Trochanteric Nail 135° vs. Stryker Gamma3 Long Nail 135° |
Short PFN A2 Vs. Long PFN A2 |
Targon PFT nail 175 mm vs. Targon PFT nail 220 mm |
Affixus Hip Fracture Nail System 180 mm vs. Orthofix VeroNail Trochanteric Nail 280–440 mm |
130°, standard PFN-A, which was 24 cm in length vs. 130°, long PFN-A in variable lengths ranging from 34–42 cm |
| Operative time (Short vs. Long) |
51 (48–55) vs. 80 (74–87) |
53.11±8.36 vs. 81.38±12.01 |
48.7±13.7 vs. 78.8+/-24.7 |
30.0 (7.3) vs. 35.1 (7.6) |
41 (20–51) vs. 54 (35–70) |
52.6 (34–65) vs. 71.8 (57–94) |
| Intraoperative blood loss (milliliters) (Short vs. Long) |
70 (61–79) vs. 207 (185–229) |
75.4±14.8 vs. 210±12.1 |
124.5±107.4 vs. 226.5±185.8 |
127.5 (96.5) vs. 178.5 (70.1) |
- | - |
| Length of stay in days (Short vs. Long) |
- | 8.5±0.88 vs. 9.07±1.32 |
10.2±5.1 vs. 12.3±4.8 |
21.9 (13. 7–25) vs. 20.1 (13. 7–30) |
- | 5.4 (2–11) vs. 4.9 (2–9) |
| Harris hip score (Short vs. Long) |
3 months 76 (IQR, 74–78) vs. 3 months 71 (IQR: 68–74) |
6 months: 84.76±3.68 12 months: 88.53±3.32 vs. 6 months: 82.37±3.79 12 months: 87.29±3.43 |
- | - | - | 12 months 74 (61–88) vs. 12 months 79 (59–92) |
| TAD mm (Short vs. Long) |
8.3 (17.2–19.4) vs. 18.8 (17.7–0.51 19.7) |
18.1±1.53 vs. 17.8±1.69 |
- | - | - | 22 (14–31) vs. 24 (15–39) |
| Complications (Short) |
12 total complications including: Peri-implant fracture 2 Lag Screw Cut-out 3 Deep infection 1 |
Screw cut-out 2 | Femoral canal impingement 1 Screw cut-out 1 Limb shortening 4 |
Implant cut-out 2 Non-union 1 Femoral Aneurysm 1 5 Pneumonia Urinary tract infection 5 Pressure sores 3 Delirium 8 Gastrointestinal bleed 1 Congestive heart failure 1 Acute renal failure 4 |
Trendelenburg gait 11 Leg length discrepancy 3 Peri-implant fracture 1 |
Implant failure 1 Malunion 3 |
| Complications (Long) |
12 total complications including: Peri-implant fracture 2 Lag Screw Cut-out 2 Deep infection 2 |
Screw cut-out 1 Peri-implant fracture 1 |
Femoral canal impingement 5 Screw cut-out 2 Limb shortening 1 |
Implant cut-out 4 Pneumonia 4 Urinary tract infection 6 Pressure sores 1 Delirium 6 Gastrointestinal bleed 3 Congestive heart failure 1 Myocardial infection 1 Atrial fibrillation 1 Deep vein thrombosis 1 |
Trendelenburg gait 10 Leg length discrepancy 2 Z-effect phenomenon |
Deep infection 2 Malunion 6 |
| Reoperation for any reason (Short vs. Long) |
5 vs. 8 |
2 vs. 2 |
1 vs. 4 |
5 vs. 3 |
1 vs. 1 |
0 vs. 2 |
| 1-Year mortality (Short vs. Long) |
- | - | 0 vs. 0 |
30 Days: 15 120 Days: 28 365 Days: 44 vs. 30 Days: 8 120 Days: 15 365 Days: 27 |
- | 2 vs. 3 |
IQR: Interquartile range, W-A: Trochanteric fixation nail-advanced, PFN: Proximal femoral nail, PFN-A: Proximal femoral nail-antirotation, vs.: Versus
Quality assessment
Figure 2 demonstrates the quality assessment of the studies included in the analysis.
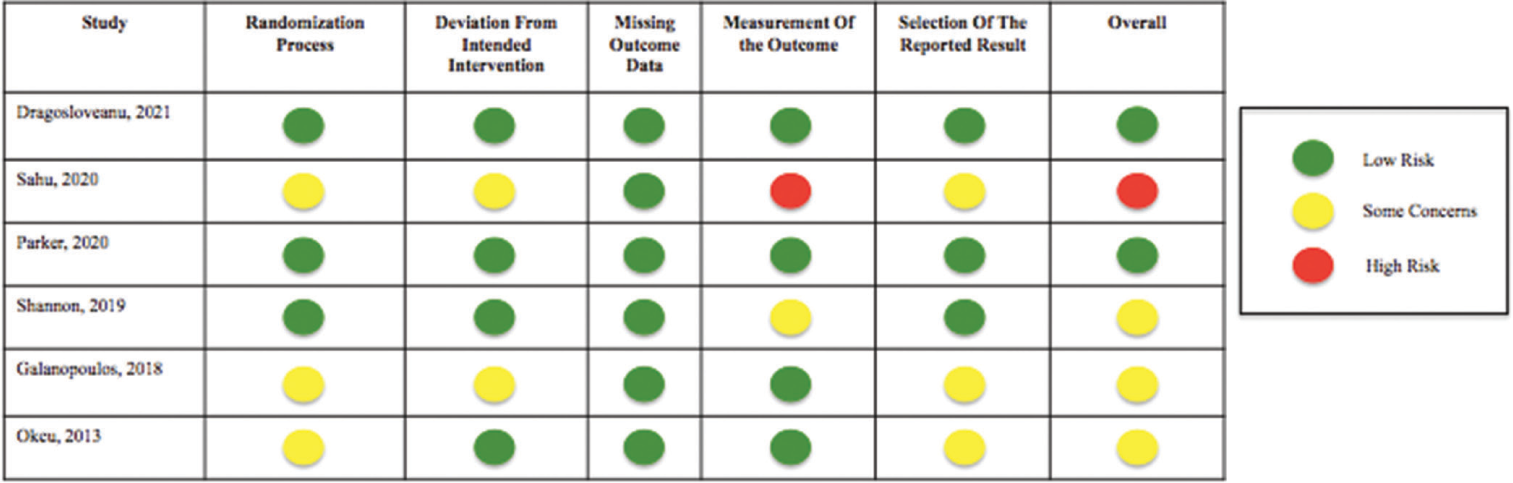
- Quality assessment of the included studies using RoB-2 Tool.
Outcome analysis
Operation time, length of stay, blood loss, and blood transfusion
The analysis comparing the operative time difference between short and long nail fixation encompassed six studies. The utilization of short nails had significantly lower operative time compared to the long nails (Figure 3; WMD = −20.33; 95% CI: −29.90–−10.76). Notably, this analysis exhibited substantial heterogeneity (I2 = 96%, P = 0.00).
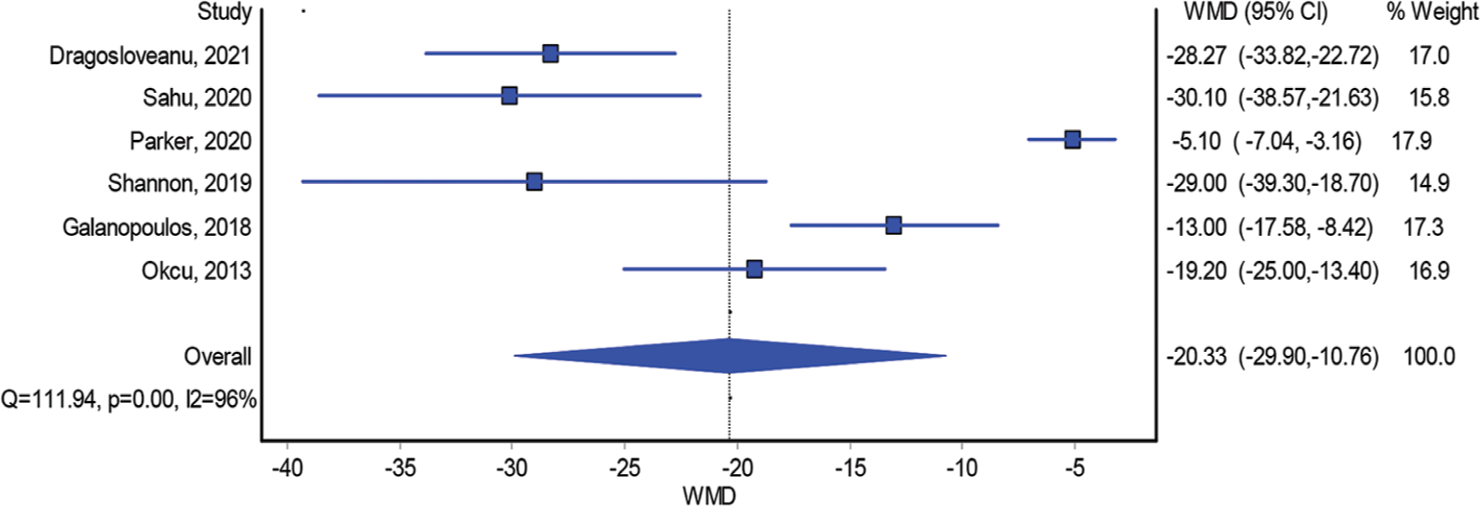
- Operative time.
Furthermore, the examination of blood loss involving four studies unveiled that patients subjected to short nail fixation experienced significantly lower blood loss compared to those with long nail fixation (Figure 4; WMD = −106.31; 95% CI: −155.43–−57.19). Notably, this analysis also displayed substantial heterogeneity (I2 = 94%, P = 0.00).
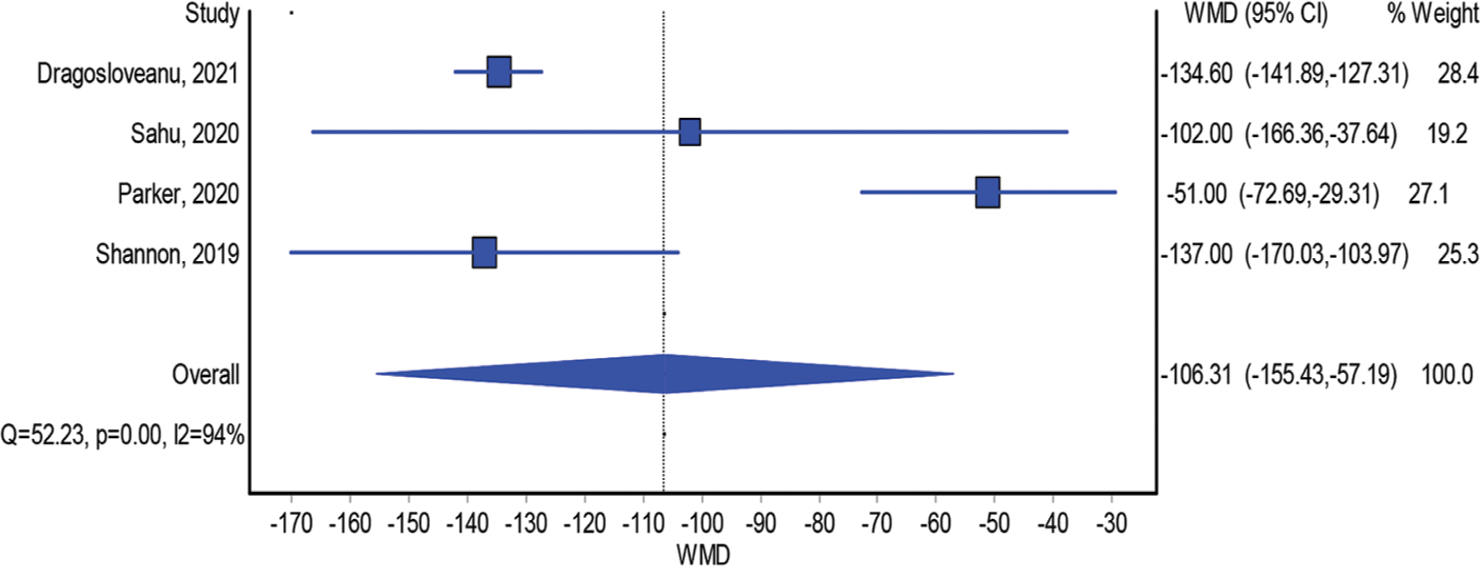
- Blood loss.
Similarly, the duration of hospital stay was evaluated in five studies that encompassed both groups. However, no statistically significant difference was detected in the length of hospital stay between the two groups (Figure 5; WMD = 0.05; 95% CI: −1.44–1.53). Nevertheless, a significant level of heterogeneity was evident in this model (I2 = 87%, P = 0.00).
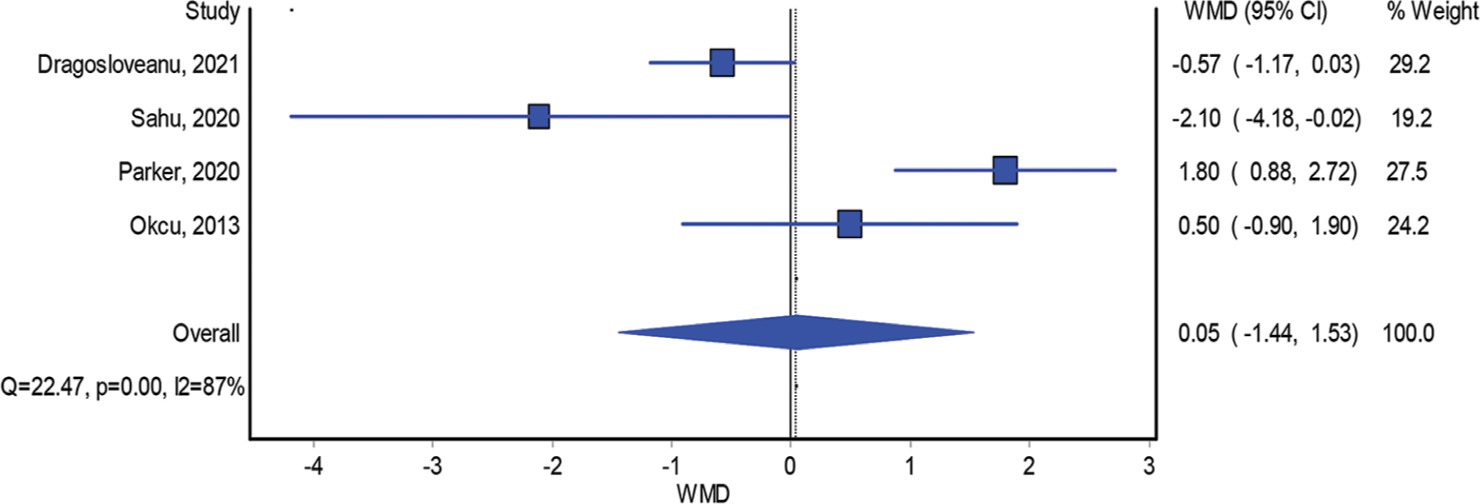
- Length of hospital stay.
Furthermore, the investigation into the necessity for blood transfusion, involving two studies, found no distinction across the two arms (Figure 6; RR = 0.96; 95% CI: 0.57−1.60). Notably, minimal heterogeneity was observed in this analysis (I2 = 4%, P = 0.31).
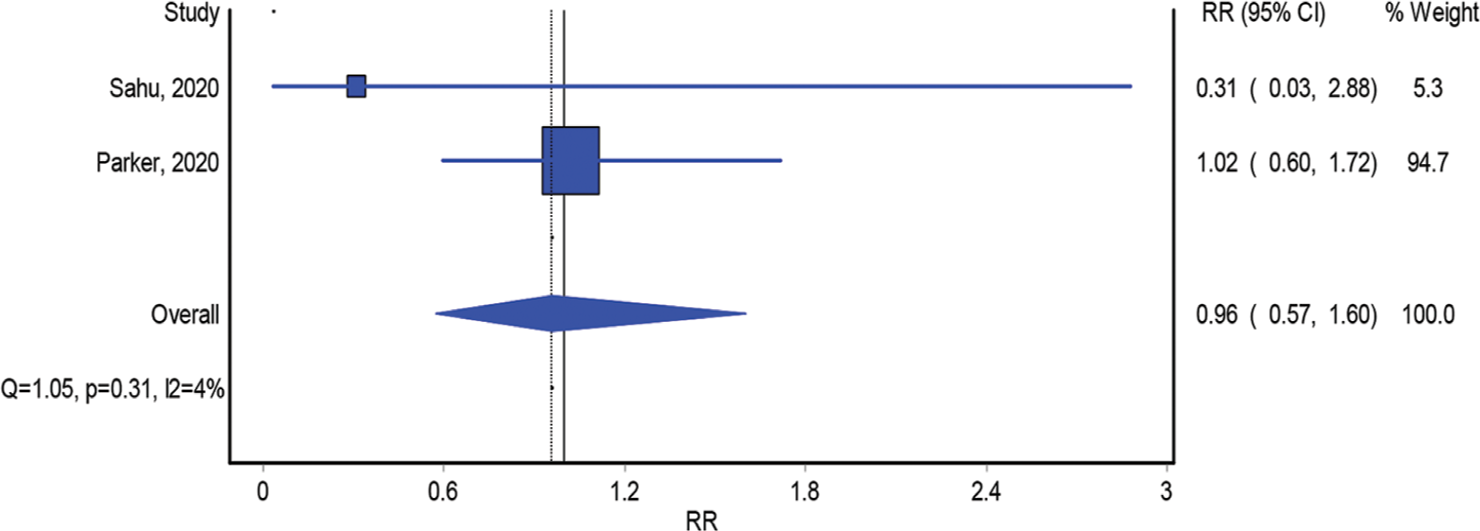
- The need for blood transfusion.
Functional outcome
Two studies compared short and long nail fixation in treating intertrochanteric fractures regarding HHS. The model that included studies that compared the interventions according to HHS showed insignificant differences between the two implants (Figure 7; WMD = −1.40; 95% CI: −7.45–4.64). The model also showed significant heterogeneity (I2 = 80%, P = 0.02).
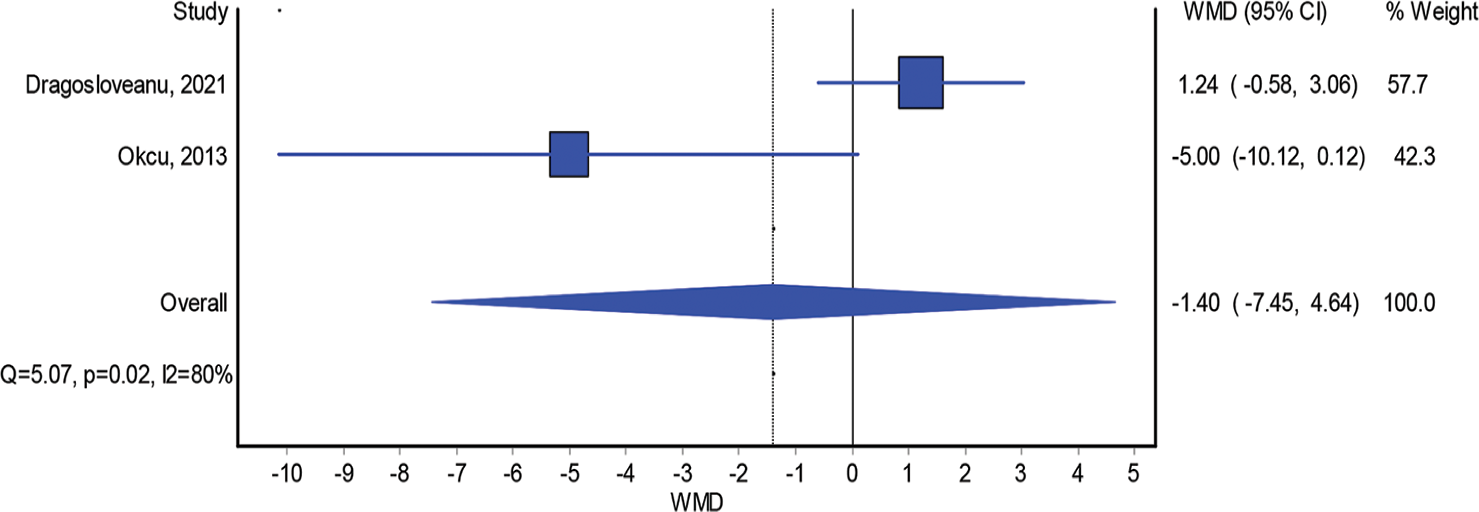
- Harris hip score.
Complication, reoperation, and mortality rates
The analysis examining complications associated with short and long nail fixation encompassed six studies. The findings from this analysis demonstrated the absence of difference in the occurrence of complications between patients who underwent fixation with short and long nails (Figure 8; RR = 1.00; 95% CI: 0.76–1.32). Importantly, this analysis exhibited negligible heterogeneity (I2 = 0%, P = 0.80).
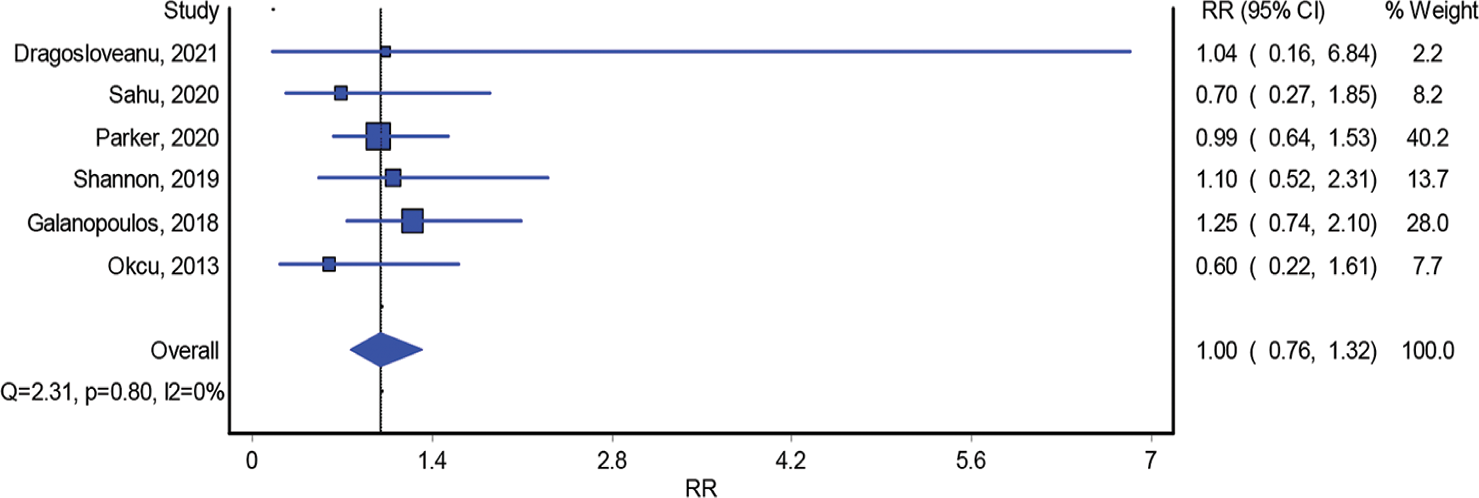
- Complication rate.
Moreover, rates of reoperation were evaluated across six studies. The model incorporating these studies found no distinction in the reoperation rates across the two arms (Figure 9; RR = 0.76; 95% CI: 0.38–1.51). This model displayed minimal heterogeneity (I2 = 0%, P = 0.73).
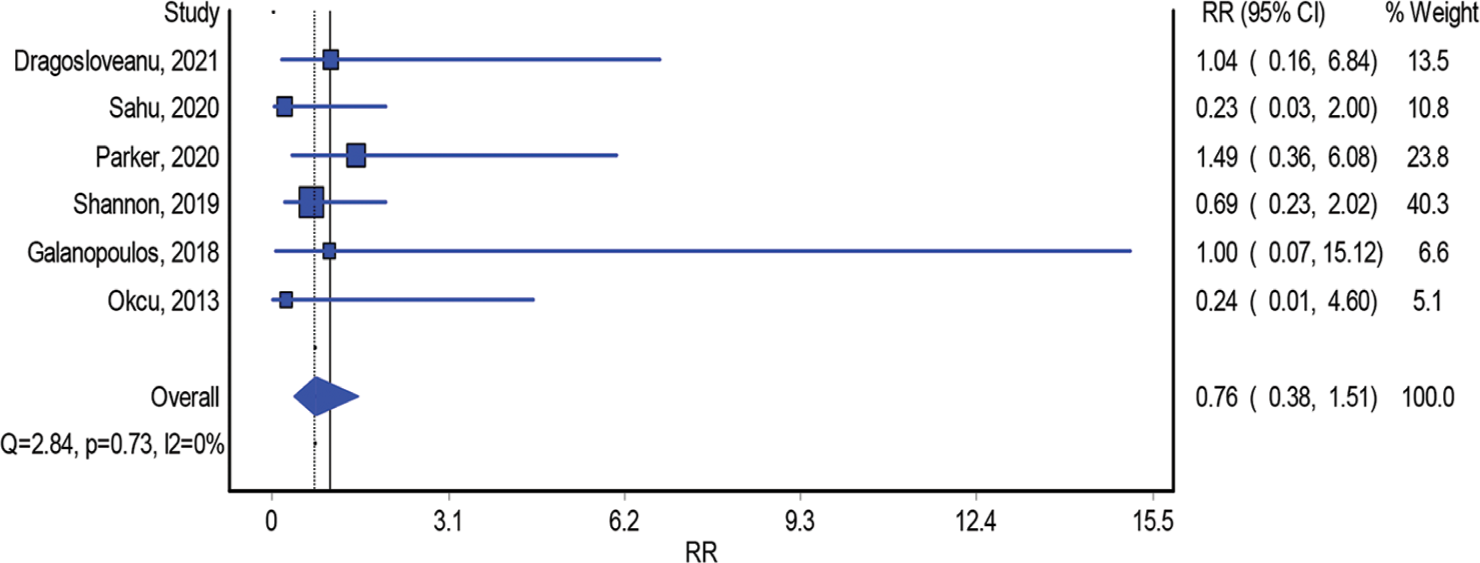
- Reoperation rate.
Furthermore, the assessment of mortality rates within the two groups was based on two studies. The model analyzing these studies indicated no substantial difference in mortality rates (Figure 10; RR = 1.40; 95% CI: 0.95–2.08). Notably, this analysis demonstrated insignificant heterogeneity (I2 = 0%, P = 0.50).
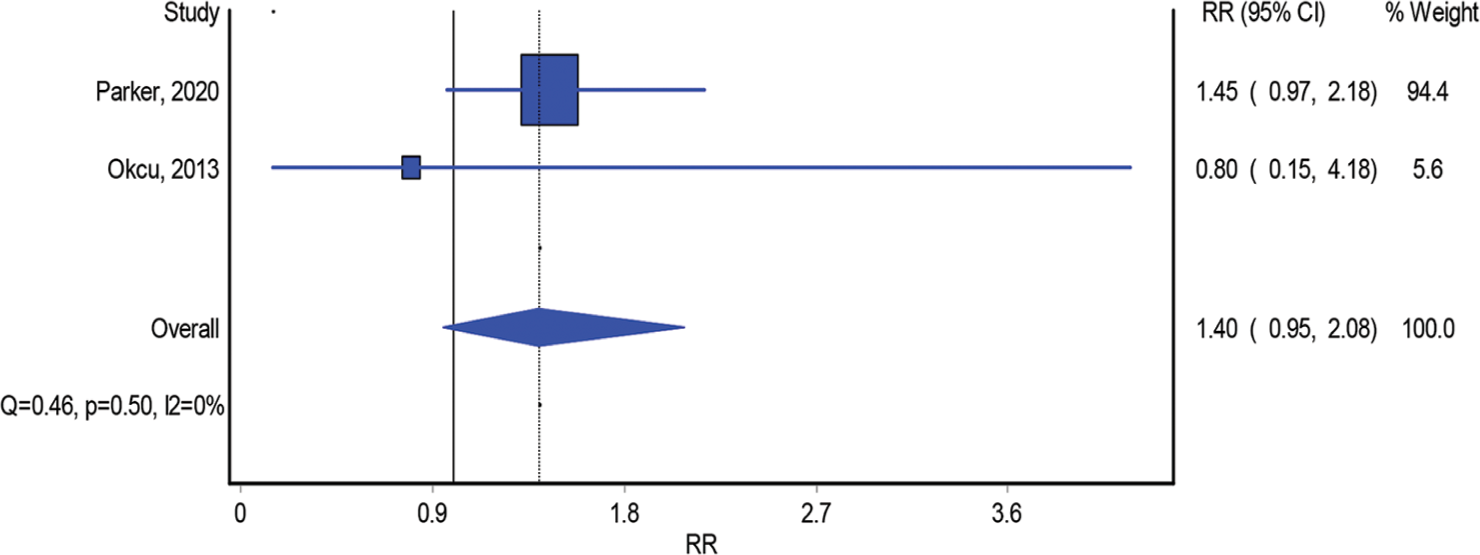
- One-year mortality rate.
DISCUSSION
In managing unstable variations of intertrochanteric hip fractures, intramedullary nailing has emerged as the preferred treatment method.[20] Numerous RCTs have been published, examining the outcomes linked to using short and long intramedullary nails for these types of fractures, utilizing various outcome measures. The motivation behind conducting this meta-analysis was the absence of robust consensus regarding the appropriate indications for using long or short nails in intertrochanteric fractures.[21]
The findings of this meta-analysis, based on RCTs, revealed notable benefits of employing short nails. Specifically, using short nails was linked to significant reductions in both blood loss and operative time. However, no significant disparities were observed in terms of HHSs, duration of hospital stay, blood transfusion requirements, complication rates, reoperation rates, and 1-year mortality rates. Operative time can have significant impacts on blood loss and blood transfusion.
Our study observed that the mean operative time for short nails was significantly shorter than that for long nails. This finding aligns with existing literature and can be attributed to various factors associated with the long nailing technique. This technique often necessitates additional steps such as distal reaming, precise nail length measurement, and the placement of distal interlocking screws under the guidance of fluoroscopic intensifiers. These added procedural elements in long nail fixation contribute to the longer operative times observed.
Long nails require longer operative times, which is expected to be associated with more blood loss. Furthermore, the time interval between opening the canal and introducing the long nail tends to be longer, which can result in a delay in achieving the tamponade effect. This delay in achieving hemostasis can contribute to increased blood loss when long nails are used in the fixation procedure. Zhang et al.’s study on 2431 patients reported 12.5 min longer surgical times and 37.4 mL more intraoperative blood loss when long nails are used.[22] Similarly, Hou et al and Boone et al yielded comparable results, highlighting that the utilization of long nails correlated with elevated levels of blood loss (43 mL and 35 mL, respectively) and extended operative durations (13 min and 20 min, respectively).[10,23]
The findings of this meta-analysis are consistent with the existing body of research, strengthening the prevailing consensus that short intramedullary nails are linked to decreased blood loss and shorter operative times.
However, long nails have been previously favored due to the lower risk of periprosthetic fractures. However, newer generations and designs of short nails have eliminated this concept by improving the diameter of the distal locking screws and the anatomic fitting of the nail.[24-26] This meta-analysis confirmed this, as we found no statistically significant difference in complication and reoperation rates when comparing both implants. These findings are consistent with Cinque et al and Shannon et al studies.[11,26]
Despite the advantages observed with the use of short nails, there were no significant differences in functional scores across the two arms.
In a study by Shannon et al., patients treated with short and long intramedullary nails exhibited similar HHS. Although there was a statistical variance of 5 points favoring the short nails group, this difference was not considered clinically significant.[11]
Limitations
In this study, several limitations should be acknowledged. First, the low number of available RCTs (six in total) and the small number of included patients. However, this study represents the highest available level of evidence in the literature. Second, the included studies had several types of biases, including observer and confounding bias. Third, substantial heterogeneity was observed in our analysis models. The observed heterogeneity can be attributed to the disparities among the studies included, stemming from variations in fracture classifications and nail types. Moreover, due to the restricted participant pool, conducting an in-depth analysis concerning the influence of each fracture classification and TAD on the outcome measures was impossible. Nonetheless, it is important to note that this meta-analysis, which is based on RCTs, offers the highest caliber of evidence available in the literature regarding the optimal nail length for intertrochanteric fracture fixation.
Finally, it is worth mentioning that, due to the limited number of studies included, an assessment of potential publication bias was not undertaken in this analysis.
CONCLUSION
The choice of nail length for treating intertrochanteric hip fractures does not significantly influence functional outcomes, blood transfusion rates, reoperation rates, complication rates, or 1-year mortality rates. Nevertheless, when comparing the fixation of intertrochanteric fractures, it is noteworthy that short nails result in significantly reduced operative time and lower blood loss compared to long nails.
AUTHORS’ CONTRIBUTIONS
ATH, HK, and LAS performed the literature search. ATH, JD and HK collected the data. ATH and LAS performed a quality assessment. AAT performed the statistical analysis. ATH, AAT, and OA wrote the manuscript. GA and HA supervised the whole project, helped prepare the manuscript, and reviewed the final manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
This article does not contain any studies with human participants performed by any of the authors.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
DECLARATION OF PATIENT CONSENT
Patient’s consent is not required, as there are no patients in this study.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- The future of hip fractures in the United States. Clin Orthop Relat Res. 1990;252:163-6.
- [CrossRef] [Google Scholar]
- A comparative study of the therapeutic effect between long and short intramedullary nails in the treatment of intertrochanteric femur fractures in the elderly. Chin J Traumatol. 2015;18:332-5.
- [CrossRef] [PubMed] [Google Scholar]
- The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1:6-14.
- [CrossRef] [PubMed] [Google Scholar]
- Intertrochanteric femur fracture stability: A surrogate for general health in elderly patients? Geriatr Orthop Surg Rehabil. 2015;6:192-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hip fractures: Relevant anatomy, classification, and biomechanics of fracture and fixation. Geriatr Orthop Surg Rehabil. 2019;10:215145931985913.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcomes of intramedullary and extramedullary fixation in unstable intertrochanteric fractures: A randomized clinical trial. Arch Bone Jt Surg. 2020;8:190-7.
- [Google Scholar]
- Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1-170.
- [CrossRef] [PubMed] [Google Scholar]
- Nail length in the management of intertrochanteric fracture of the femur. J Am Acad Orthop Surg. 2016;24:e50-8.
- [CrossRef] [PubMed] [Google Scholar]
- Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31-A1, A2 and A3): A systematic review. J Orthop Traumatol. 2016;17:361-7.
- [CrossRef] [PubMed] [Google Scholar]
- Short versus long intramedullary nails for treatment of intertrochanteric femur fractures (OTA 31-A1 and A2) J Orthop Trauma. 2014;28:e96-100.
- [CrossRef] [PubMed] [Google Scholar]
- Short versus long cephalomedullary nails for pertrochanteric hip fractures: A randomized prospective study. J Orthop Trauma. 2019;33:480-6.
- [CrossRef] [PubMed] [Google Scholar]
- Short vs. long intramedullary nail systems in trochanteric fractures: A randomized prospective single center study. Exp Ther Med. 2021;23:106.
- [CrossRef] [PubMed] [Google Scholar]
- Short proximal femoral nail A2 vs. long proximal femoral nail A2 for the management of intertrochanteric fractures in elderly. Eur J Mol Clin Med. 2020;7:1144-9.
- [CrossRef] [Google Scholar]
- Short (175 mm) versus standard (220 mm) length intramedullary nail for trochanteric hip fractures: A randomized trial of 229 patients. Bone Joint J. 2020;102B:394-9.
- [CrossRef] [PubMed] [Google Scholar]
- Similar function and complications for patients with short versus long hip nailing for unstable pertrochanteric fractures. SICOT J. 2018;4:23.
- [CrossRef] [PubMed] [Google Scholar]
- Which implant is better for treating reverse obliquity fractures of the proximal femur: A standard or long nail? Clin Orthop Relat Res. 2013;471:2768-75.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097.
- [CrossRef] [PubMed] [Google Scholar]
- RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
- [CrossRef] [PubMed] [Google Scholar]
- Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing two intramedullary devices for treating trochanteric fractures: A prospective study. J Orthop Surg Res. 2010;5:9.
- [CrossRef] [PubMed] [Google Scholar]
- Nailing intertrochanteric hip fractures: Short versus long; locked versus nonlocked. J Orthop Trauma. 2015;29(Suppl 4):S10-6.
- [CrossRef] [PubMed] [Google Scholar]
- Long and short intramedullary nails for fixation of intertrochanteric femur fractures (OTA 31-A1 A2 and A3): A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2017;103:685-90.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of pertrochanteric fractures (OTA 31-A1 and A2): Long versus short cephalomedullary nailing. J Orthop Trauma. 2013;27:318-24.
- [CrossRef] [PubMed] [Google Scholar]
- Gamma nails revisited: Gamma nails versus compression hip screws in the management of inter-trochanteric fractures of the hip: A meta-analysis. J Orthop Trauma. 2009;23:460-4.
- [CrossRef] [PubMed] [Google Scholar]
- Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: A systematic review of 13,568 patients. Injury. 2012;43:706-11.
- [CrossRef] [PubMed] [Google Scholar]
- Short versus long cephalomedullary nailing of intertrochanteric fractures: A meta-analysis of 3208 patients. Arch Orthop Trauma Surg. 2022;142:1367-74.
- [CrossRef] [PubMed] [Google Scholar]






