Translate this page into:
Neglected perilunate injuries: Management strategies and long-term consequences: A narrative review
*Corresponding author: Dr. J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India. terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome JTJ. Neglected perilunate injuries: Management strategies and long-term consequences: A narrative review. J Musculoskelet Surg Res. 2025;9:202-12. doi: 10.25259/JMSR_380_2024
Abstract
Neglected perilunate injuries are a challenging and often overlooked condition that can result in significant long-term consequences if not properly managed. These injuries, typically resulting from high-energy trauma, involve dislocations and fractures around the lunate bone, with delayed diagnosis leading to complex management scenarios. This narrative review examines the management strategies for neglected perilunate injuries and the associated long-term outcomes. The review explores the efficacy of different surgical approaches, including open reduction and internal fixation, proximal row carpectomy, wrist fusion, and bone retinacular bone graft scapholunate reconstruction. By evaluating the existing literature, this article highlights the critical need for early diagnosis and appropriate intervention to minimize the risk of post-traumatic arthritis and other degenerative changes.
Keywords
Bone retinacular bone graft
Long term
Neglected
Perilunate injury
Post-traumatic arthritis
Proximal row carpectomy
Scapholunate
Wrist fusion
INTRODUCTION
Perilunate injuries, encompassing a spectrum of carpal dislocations and fractures centered around the lunate bone, present a formidable challenge in hand and wrist traumatology.[1-3] Although relatively uncommon, comprising approximately 10% of carpal injuries, their severity and potential for long-term complications demand prompt recognition and meticulous management.[1,2] The intricate ligamentous and bony wrist architecture, susceptible to disruption in various patterns during these injuries, can lead to significant instability, pain, and compromised hand function.
Typically triggered by a high-energy impact to a hyperextended and ulnarly deviated wrist, often accompanied by intercarpal supination, perilunate injuries frequently occur due to falls from a height or motor vehicle accidents.[1,3] The force transmitted through the carpus initiates a cascade of ligamentous disruption, beginning with the scapholunate (SL) ligament and potentially progressing to involve other crucial stabilizers such as the lunotriquetral (LT) and capitolunate ligaments.[2] In severe cases, this ligamentous instability can culminate in complete carpal dislocation or fracture-dislocations, further jeopardizing wrist function and stability. Alarmingly, despite their severity, the diagnosis is missed initially in 25% of cases.[1,3]
Neglected perilunate injuries, where diagnosis and treatment are delayed beyond 45 days, represent an especially complex clinical scenario.[4-6] The prolonged period of instability and abnormal joint mechanics can trigger a series of debilitating complications, including post-traumatic arthritis, carpal tunnel syndrome (CTS), median nerve dysfunction, and chronic regional pain syndrome.[7-10] These sequelae can severely impact a patient’s quality of life, underscoring the critical importance of timely diagnosis and intervention.
This narrative review aimed to provide a comprehensive overview of current management strategies for perilunate injuries, particularly emphasizing the challenges posed by neglected cases.
TIMING OF TREATING PERILUNATE INJURIES
The timing of surgery for perilunate injuries is crucial in determining the overall outcome for patients. According to the systematic review and meta-analysis by van der Oest et al.,[3] perilunate injuries, including perilunate dislocations (PLDs) and perilunate fracture-dislocations (PLFDs), are complex and often missed, representing 7% of all carpal traumas. The study highlights that patients who undergo surgical treatment within 7 days of injury tend to have better clinical outcomes, mainly when treated with closed reduction and internal fixation (CRIF). In contrast, delayed treatment, defined as surgery performed between 7 and 45 days, still offers reasonable outcomes but is less favorable than acute treatment. However, the most concerning results are seen in cases where surgery is delayed beyond six weeks, with these patients experiencing the worst outcomes, particularly in chronic PLD cases. These findings underscore the importance of early diagnosis and prompt surgical intervention to optimize recovery and minimize long-term complications. Early referral to specialized treatment centers is recommended to ensure timely and targeted care for these challenging injuries.
PLDS AND PLFDS
PLDs and PLFDs are rare but serious injuries that often lead to poor outcomes, particularly in high-demand populations. A study by Dunn et al.[11] evaluated the outcomes of these injuries in a young, active military population, highlighting the challenges associated with their treatment. The study included surgical treatment for PLD or PLFD, with an average follow-up of nearly four years. The findings revealed that these injuries frequently result in significant functional limitations, with an average range of motion (ROM) of 74% and grip strength of 65% compared to the unaffected wrist.[11] In addition, 78% of patients reported pain during activity, and only 55% remained on active duty at the final follow-up. Worse outcomes were associated with injuries to the dominant extremity, trans-scaphoid PLFDs, greater arc injuries, and cases managed with pinning alone.[11] Conversely, injuries to the non-dominant extremity were more likely to result in good to excellent outcomes, with better ROM and a higher likelihood of returning to sports. These findings underscore the complexity of PLD/PLFD injuries and suggest that patients in high-demand roles should be counseled on the potential for significant postoperative limitations.
CHALLENGES
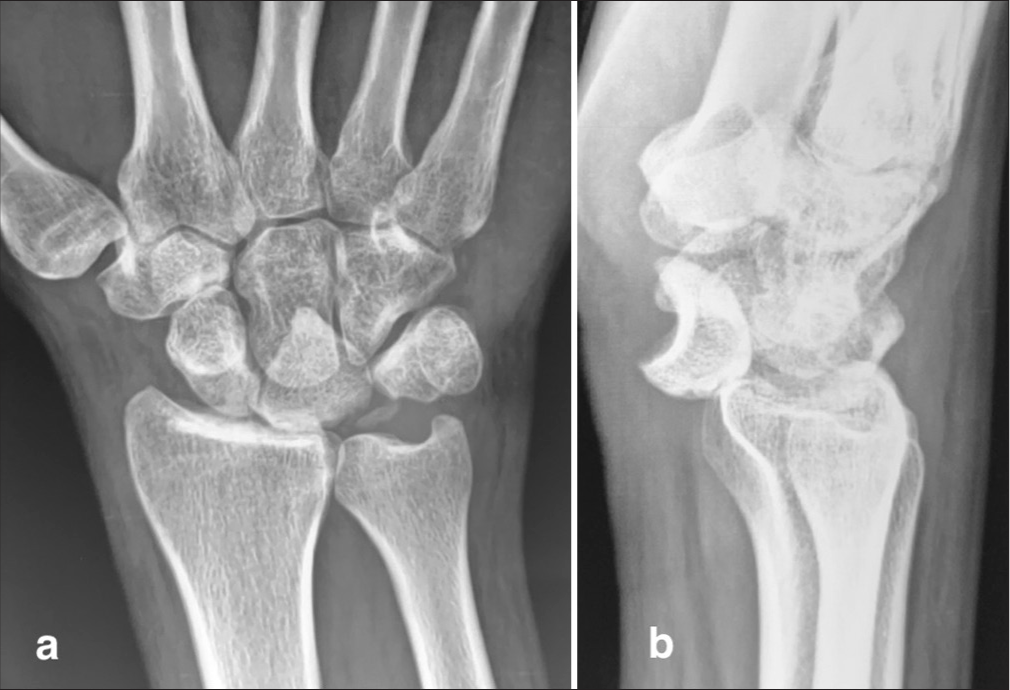
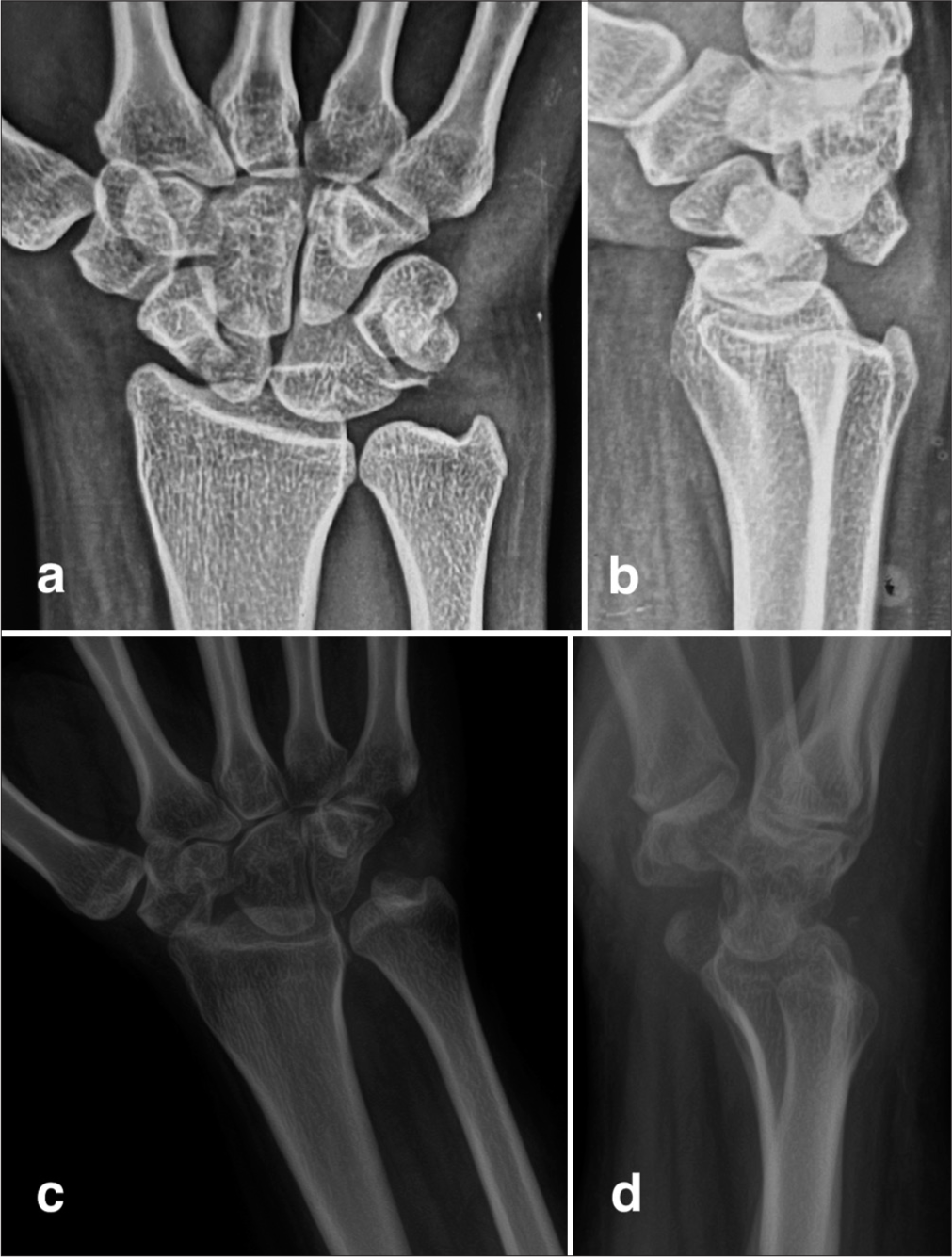
Managing neglected perilunate injuries is fraught with challenges due to the complex nature of the wrist’s anatomy and the delayed presentation of these cases. One of the primary challenges is the accurate diagnosis of these injuries, as poor-quality radiographs often lead to missed or incorrect diagnoses [Figure 1].[1-4] Even when diagnosed promptly, the timing of intervention remains critical. Delayed treatment can lead to ligament scarring and contracture of surrounding tissues, rendering CRIF with K-wires ineffective due to insufficient ligamentous support and stability [Figure 2].[4-7] In such cases, closed reduction and immobilization alone often fail to maintain adequate reduction, necessitating timely surgical intervention.
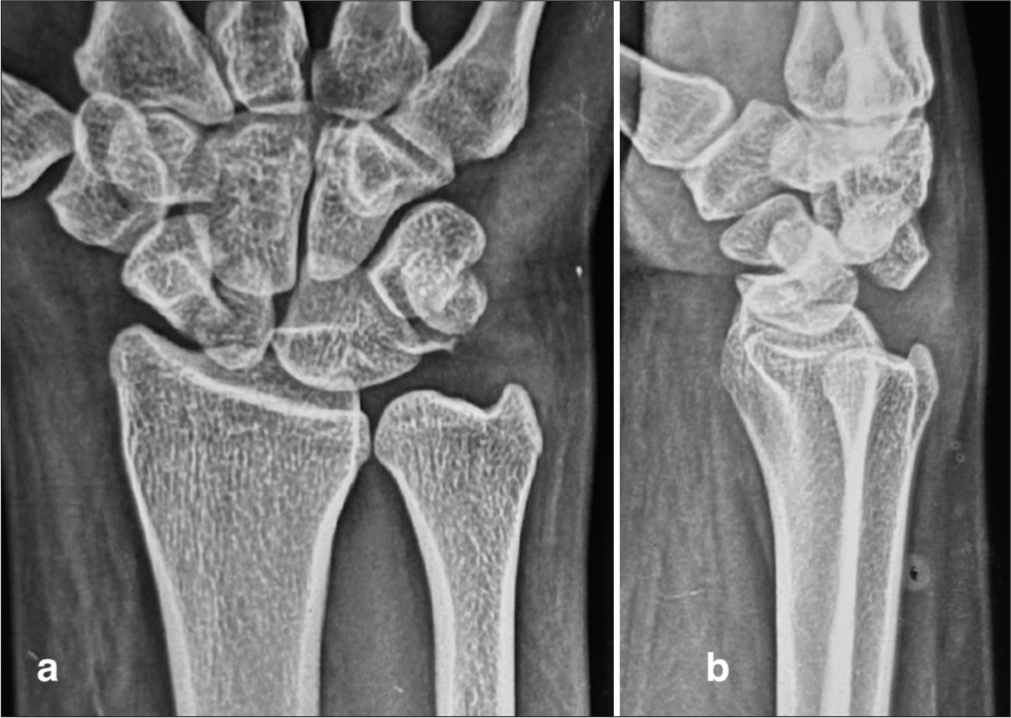
- Radiographs of a 25-year-old woman initially diagnosed with a wrist sprain without imaging. Six months post-injury, imaging (a and b) reveals a trans-scaphoid perilunate fracture-dislocation. This case highlights the importance of obtaining radiographs for suspected wrist injuries to avoid missed or delayed diagnoses, especially in high-impact mechanisms.

- Trans-scaphoid perilunate fracture dislocation: Initial treatment and subsequent complications (a) Pre-operative radiograph: Demonstrates a trans-scaphoid perilunate fracture-dislocation in a 30-year-old man. (b) Post-operative radiograph: Shows the initial treatment with closed reduction and internal fixation using multiple K-wires. (c) Follow-up radiograph at 9 months: Reveals persistent scaphoid non-union despite K-wire removal at 6 weeks, accompanied by the patient’s reported pain and difficulty using the hand. This case underscores the challenges of managing perilunate injuries, even with initial surgical intervention. The development of scaphoid non-union (white arrow) highlights the importance of close follow-up and consideration of additional procedures, such as ligament repair or reconstruction, and headless compression screw fixation with bone grafting, to promote healing and restore function.
Another significant challenge is selecting the appropriate surgical approach. Given the variability in the presentation and extent of damage in neglected cases, there is no onesize-fits-all solution. Surgical options must be tailored to the individual patient’s needs, considering factors such as the duration of neglect, the degree of carpal bone displacement, and the presence of associated conditions like CTS.
EARLY VERSUS DELAYED TREATMENT
The timing of surgical intervention for trans-scaphoid PLFD significantly impacts clinical outcomes, as highlighted by the study conducted by Komurcu et al.[4] This retrospective and randomized study compared the results of ORIF results in patients treated acutely (within a short period post-injury) or after a delay. The findings revealed that early surgical treatment led to better overall outcomes, with the early-treated group achieving a mean clinical score of 89.2 (classified as good) compared to 72.5 (fair) in the delayed treatment group.[4] In addition, the range of motion (flexion and extension) was notably higher in the early-treated group (129.5°) compared to the delayed group (95.5°).[4] Grip strength outcomes also favored early intervention, with four out of six patients in the acute group regaining normal grip strength, whereas the delayed group had a higher incidence of significant grip strength loss.
Furthermore, post-traumatic mid-carpal arthritis developed in two of the six patients in the delayed group, highlighting the increased risk of long-term complications with delayed treatment. Despite these differences, the study recommended ORIF for the early and delayed cases. However, the superior outcomes associated with early treatment underscore the importance of timely surgical intervention in managing PLFD.
ORIF
ORIF is a common approach for managing neglected perilunate injuries, particularly in cases where there is significant displacement of the carpal bones.[2-4] The procedure involves realigning the dislocated bones and securing them with hardware such as screws or K-wires. ORIF is often combined with ligament repair or reconstruction, particularly when the SL and LT ligaments are involved.[5-8] The choice of approach, whether dorsal, volar, or a combination, depends on the specific injury pattern.[9-12]
TIMING FOR ORIF
Open reduction with direct ligament repair is typically recommended for acute PLD or lunate dislocations (LD). However, when treatment is delayed, the procedure becomes more challenging due to factors such as chronic scarring, ligament contraction, and proximal carpal migration. It is generally recognized that open reduction of LDs is more difficult than PLD. The optimal time frame for performing open reduction remains debated, with no clear consensus. Inoue and Shionoya have suggested that open reduction should be attempted within the first 2 months post-injury, noting that the likelihood of good outcomes decreases significantly if surgery is delayed beyond 8–12 weeks.[2] Conversely, Siegert et al.[13] reported favorable results in chronic PLD cases even when surgery was performed as late as 35 weeks after the injury.
Despite the challenges associated with delayed intervention, various authors have advocated for open reduction regardless of the injury’s duration. Studies, including one by Kailu et al.,[5] have demonstrated that ORIF can yield satisfactory outcomes even in delayed and chronic cases. In Kailu’s study, patients who underwent ORIF three weeks or more after injury achieved good clinical outcomes, with an average post-operative clinical score of 81 in the delayed group and 76.7 in the chronic group.[5] Although the timing of the intervention plays a crucial role, with delayed cases often leading to residual instability and a higher risk of post-traumatic arthritis, ORIF remains a viable and effective option for managing PLDs, offering the potential for significant functional recovery.
CARPAL LIGAMENTS REPAIR OR RECONSTRUCTION
Kailu et al.[5] employed a primarily dorsal approach for open reduction in chronic perilunate injuries, with meticulous removal of scar tissue and manual distraction facilitating reduction. Scaphoid fractures were stabilized with screws, and bone grafts were utilized when necessary. Ligament repair and reconstruction were also performed, followed by applying a wrist external fixator for stability and early mobilization. The study showed promising outcomes for delayed and chronic treatment groups.[5] The delayed group, treated within 3–17 weeks post-injury, demonstrated good functional recovery, with low pain levels, 90% grip strength recovery, and return to work for all patients. However, one patient developed mid-carpal arthritis, and a slight decrease in carpal height ratio was observed. The chronic group, treated beyond 17 weeks post-injury, also achieved satisfactory outcomes but with a higher incidence of midcarpal arthritis and lower grip strength recovery. Despite these challenges, most patients in this group also returned to their previous work. Both groups maintained normal SL and LT intervals at the final follow-up. Overall, Kailu et al. demonstrated the feasibility of ORIF even in delayed and chronic PLDs, highlighting the potential for good functional recovery.[5] However, the study emphasizes the importance of early intervention to minimize complications and optimize outcomes.
The author of this study prefers ORIF with SL repair through a dorsal approach using suture anchors when there is an adequate remnant of the ligament in the scaphoid [Figures 3 and 4]. If there is no dorsal SL ligament, the author prefers using two suture anchors in the scaphoid and lunate [Figures 5-8]. In all circumstances, K-wires are used for the SL and scaphocapitate joints.

- (a and b) Pre-operative radiographs of a 45-year-old man presenting with a 5-month-old neglected perilunate dislocation of the right wrist. Note the volar displacement of the lunate and associated median nerve dysfunction.

- (a and b) Intraoperative images demonstrating open reduction of the lunate and scapholunate ligament repair using 3.5 mm suture anchors. Scaphocapitate and scapholunate K-wires provide additional stability. The lunotriquetral (LT) ligament was not repaired but the LT joint was immobilized with K-wires. (c and d) Two-year post-operative radiographs showing maintained carpal bone alignment with preserved scapholunate space. The patient reported being symptom-free at this follow-up.
- (a and b) Pre-operative radiographs of a 20-year-old man with a 3-month-old neglected perilunate dislocation of the right wrist, accompanied by median nerve dysfunction.
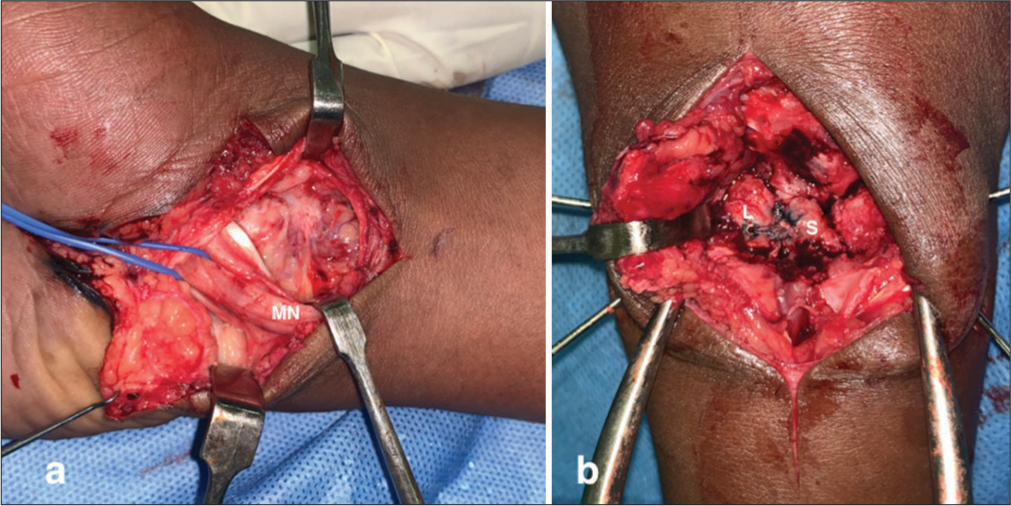
- (a) Intraoperative image showing compression of the median nerve by the dislocated lunate, necessitating carpal tunnel release. (b) Intraoperative image demonstrating scaphoid (S), lunate (L) and scapholunate ligament reconstruction using two 3.5 mm suture anchors due to the absence of viable remnants of the dorsal scapholunate interosseous ligament.
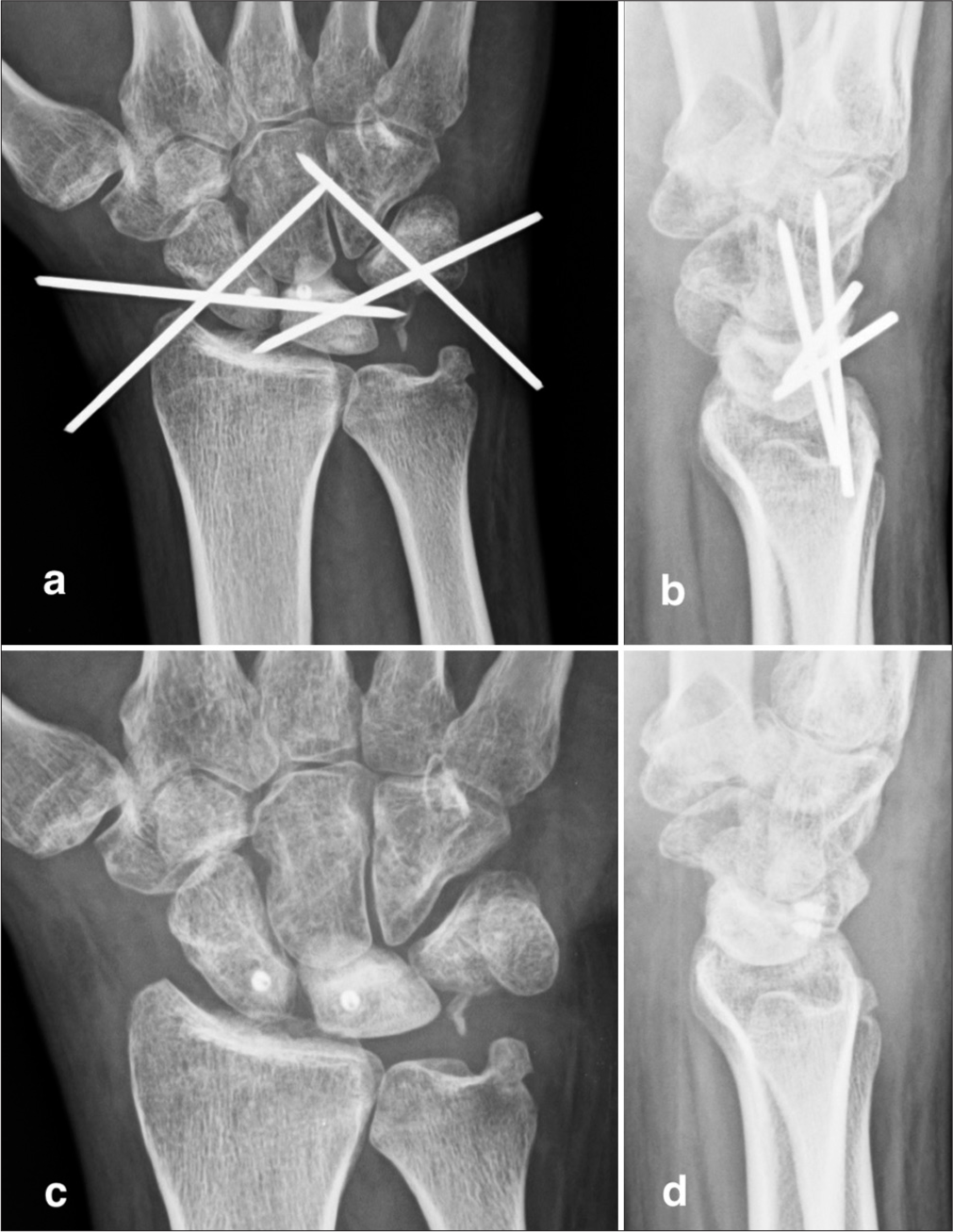
- (a and b) Post-operative radiographs showing K-wire stabilization of the scapholunate and lunotriquetral joints and the triquetrum-hamate joint due to intraoperative ligament injury and subsequent instability. (c and d) Three-year follow-up radiographs of the same patient reveal an intact scapholunate space and a symptom-free status.
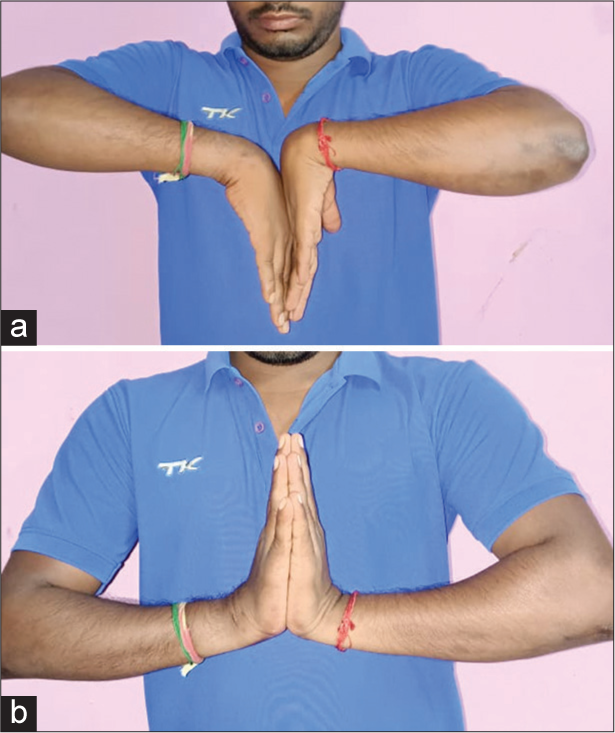
- (a and b) This clinical image demonstrates the wrist movements of the same patient, showcasing a normal range of motion with painless movement.
LIGAMENT RECONSTRUCTION USING AUTOGENOUS TENDON AND SYNTHETIC TAPE
Kang et al.[10] presented a surgical technique for neglected volar LDs, utilizing a combined volar and dorsal approach. The volar approach addressed median nerve decompression and flexor tendon repair. In contrast, the dorsal approach enabled lunate reduction and reconstruction of the SL and LT ligaments using a combination of autogenous palmaris longus tendon and synthetic tape secured with suture anchors. Post-surgery, K-wires provided temporary fixation, and a wrist external fixator was applied for 6–8 weeks to aid healing.[10]
The three cases showcased promising results at the final follow-up (11–13 months post-surgery), with patients reporting minimal or no pain and a successful return to daily activities. The average wrist flexion and extension were 45° and 53.3°, respectively, and the modified Mayo wrist score averaged a favorable 78.3. These findings suggest that surgical intervention can effectively restore function and improve quality of life, even in neglected cases.
INTERNAL BRACING (IB)
IB, a technique utilizing high-strength, non-absorbable tape, has gained considerable traction in recent years as an adjunct to traditional ligament repair in the wrist. It functions by providing crucial reinforcement to the repaired ligaments during the healing process, allowing for early controlled motion while minimizing the risk of re-rupture.[12] Studies have demonstrated that augmenting ligament repairs with IB significantly enhances their strength and stability compared to repairs without it.[12]
The benefits of IB extend beyond simply improving the biomechanical properties of the repair. Facilitating early mobilization can help prevent joint stiffness and promote faster functional recovery. This is particularly important in the context of perilunate injuries, where prolonged immobilization can lead to significant morbidity.
A recent biomechanical study investigated the efficacy of different IB configurations (short-transverse, long-oblique, and a combination of both) in a cadaveric model of SL dissociation.[12] The findings suggested that short-transverse IB was more effective in limiting SL widening, while long-oblique IB was better at addressing scaphoid flexion deformity. The combination of both techniques proved to be the most effective in managing the complex instability associated with SL dissociation.
These findings highlight the potential of IB to not only augment ligament repair strength but also to address specific biomechanical challenges associated with different injury patterns. The ability to tailor IB configurations to the individual patient’s needs may lead to improved outcomes and a faster return to function.
However, despite its promising potential, IB is not without its limitations. The technique requires careful surgical execution and meticulous attention to detail to ensure optimal placement and tensioning of the tape. In addition, long-term data on the efficacy and durability of IB in perilunate injuries are still limited. Further research is needed to fully elucidate the role of IB in the management of both acute and neglected perilunate injuries.
BONE RETINACULAR BONE (BRB) GRAFT SL RECONSTRUCTION
The BRB surgical technique, as described by Soong et al.[14] provides a structured approach to SL ligament reconstruction, particularly in cases of dynamic SL instability. The technique demonstrated a generally good functional outcome over an average follow-up period of 11.9 years, with an average Mayo wrist score of 83. However, a 50% failure rate was observed, with three out of six patients requiring additional surgery due to graft-related issues. Despite these challenges, BRB reconstruction remains a viable option for managing dynamic SL instability.
The author has successfully extended to treat neglected PLDs. The procedure begins with a dorsal incision over the Lister’s tubercle to access the SL interval. A bone block, along with the attached retinaculum and periosteum, is harvested from the Lister’s tubercle, and the central portion of the bone block is removed to create a trough for graft insertion. The SL interval is then carefully reduced and temporarily stabilized with K-wires while recipient sites on the scaphoid and lunate are prepared to accommodate the graft. The BRB graft is inserted into these troughs and secured with a mini-screw to ensure stable fixation. The procedure concludes with the repair of the dorsal capsule and the closure of the retinaculum, with the extensor pollicis longus tendon transposed above it. Overall, the BRD reconstruction yielded favorable long-term results in terms of Mayo scores, grip strength, and return to work rates in the authors’ series [Figures 9-11].

- (a and b) Radiographs of a 46-year-old man with a 4-month-old perilunate dislocation of the right wrist.

- (a) Intraoperative image showing the absence of the dorsal scapholunate interosseous ligament (SLIL) and its remnants. A trough was created over the dorsal aspect of the lunate and scaphoid at the anatomical site of the dorsal SLIL. (b) A 2 cm bone-retinaculum-bone graft was harvested from Lister’s tubercle, including the retinaculum and distal radius with periosteum. (c) The bone-retinaculum-bone graft was inserted into the prepared trough and stabilized with two mini-screws, one in the scaphoid (S) and one in the lunate (L).

- (a and b) K-wires were used to immobilize the scapholunate joint, scaphocapitate joint, and lunotriquetral joint. (c and d) At the 2-year follow-up, the scapholunate space was well maintained, and the patient remained symptom-free, having returned to his previous work.
ROLE OF STAGED REDUCTION, FIXATION, AND LIGAMENT RECONSTRUCTION
Staged reduction is an effective surgical technique for managing neglected trans-scaphoid PLFD when early reduction is not feasible. Garg et al.[8] treated patients using a two-stage approach. In the first stage, a spanning external fixator was applied with two pins in the dorsolateral radius and two in the second metacarpal, allowing gentle distraction at 1 mm per day. Weekly radiographs monitored the process, confirming adequate distraction when the proximal capitate aligned with the distal lunate and the radiocarpal joint began to distract. The second stage involved ORIF of the carpal bones and intercarpal ligament reconstruction.
The ORIF was performed through a dorsal approach, with a transverse incision 1 cm distal to the radiocarpal joint. The extensor retinaculum was incised, and the tendons were retracted to expose the dorsal joint capsule. After opening the dorsal capsule with a radial V-shaped flap, the fractures were reduced and stabilized with K-wires, followed by definitive fixation with Herbert screws. SL and scaphocapitate ligaments were reconstructed using suture anchors, and in cases of redundancy, a capsular flap was used for reinforcement. The scaphoid’s vascularity was confirmed with a K-wire, and bone grafting from the iliac crest supported healing. This staged technique achieved a good functional, pain-free ROM in most patients.
PROPHYLACTIC CARPAL TUNNEL RELEASE (CTR)
In their case series, Pelrine et al.[15,16] reported on eight patients with delayed diagnoses of PLDs, with an average diagnostic delay of 133 days. The majority of these patients were young males, and half had greater arc injuries. For the five patients with chronic injuries (diagnosed over 45 days post-injury), treatment varied depending on injury severity. Three underwent proximal row carpectomy (PRC), one had scaphoid excision and four-corner fusion, and one received wrist arthrodesis. The three subacute cases (diagnosed within 7–45 days) were treated with a combination of scaphoid ORIF and ligament repair. Prophylactic CTR was performed in 62.5% (5/6) of patients. However, the effectiveness of CTR in reversing deficits from acute CTS diminishes over time. Pre-operative electromyography can help determine the potential benefit of CTR but should not delay definitive treatment of the perilunate injury. Overall, the study highlighted the challenges of managing neglected perilunate injuries and the need for individualized treatment approaches.[15]
PRC
PRC is often considered for cases where the scaphoid is proximally displaced or when the injury is not reducible.[4,5,17] This procedure involves the removal of the proximal row of carpal bones, including the scaphoid, lunate, and triquetrum, to alleviate pain and restore function.[17-20] PRC is particularly useful in cases where the carpal bones are irreparably damaged, or the patient presents with proximal carpal row advanced degenerative changes.
Shinohara et al.[19] conducted a study evaluating the outcomes of PRC in six patients with unreduced PLD. The average time between injury and surgery was 24 weeks. The pain was eliminated in most cases, and patients achieved an average flexion-extension arc of 59% and grip strength of 72% compared to the unaffected side. The modified Mayo wrist score averaged 71 points, indicating satisfactory outcomes. However, the post-operative radius-capitate alignment, which was influenced by the pre-operative capitate position, significantly impacted the final results. Patients with poor alignment tended to have lower scores than those with favorable alignment.
Rettig and Raskin reported on their experience managing 12 patients with chronic, severe PLDs using PRC.[20] These injuries had been untreated or inadequately addressed for at least eight weeks, with an average delay of 15 weeks before surgery. Their surgical approach involved both dorsal and volar incisions in addressing median nerve decompression, lunate excision, capsuloligament repair, and carpectomy of the scaphoid and triquetrum. Temporary K-wire fixation was used to stabilize the wrist during healing. The study found that PRC effectively relieved pain and median nerve symptoms, while also restoring a significant degree of wrist motion and grip strength. These results support PRC as a viable treatment option for chronic, severe PLDs, even when presented late.
In the author’s experience with acute and chronic PLFD, the outcomes of PRC are generally favorable, with patients reporting significant pain relief and improved wrist function [Figure 12].[17] However, the long-term success of PRC is variable, particularly in younger patients, where the risk of progressive degenerative changes is higher.
- A 25-year-old woman presented with a 9-month history of persistent pain and stiffness in her left wrist, initially diagnosed as a wrist sprain following a fall. (a and b) Radiographs revealed a trans-scaphoid perilunate dislocation. (c and d) Due to intraoperative findings of irreducibility, instability, and loss of carpal ligaments, a proximal row carpectomy was performed, preserving an intact capitate. The patient achieved a good functional outcome at the 2-year follow-up.
PARTIAL/TOTAL WRIST FUSION
Wrist fusion, or arthrodesis, is often reserved for cases with extensive damage to the wrist’s articular surfaces, or when other surgical options have failed.[2-6] This procedure permanently fuses the carpal bones to eliminate pain and stabilize the wrist. The study by Eid[21] on Scaphoid Excision and Four-Corner Fusion (SE4CF) for neglected PLDs reported positive preliminary results. The procedure effectively relieved pain and improved all patients’ ROM and grip strength. The average Quick DASH score at the final follow-up was 12.5, indicating good hand function. The authors suggest that SE4CF is a viable treatment option for neglected PLDs, offering pain relief and good hand function. The study’s limitations include a small sample size and the need for longer follow-up to assess long-term outcomes.
FUNCTIONAL OUTCOME
The functional outcomes of treating chronic perilunate injuries with ORIF are generally satisfactory, even when the injuries are managed well beyond the acute phase.[21-25] Inoue and Shionoya’s study on late treatment of unreduced PLDs revealed that timing significantly impacts surgical outcomes.[2] Early intervention (within two months) for ORIF of the lunate led to the best results, while delayed treatment resulted in mid-carpal arthritis, even if asymptomatic in some cases. PRC generally yielded fair to poor outcomes, with low pain levels but limited ROM and grip strength. Lunate excision and arthrodesis had the poorest outcomes, often leading to arthritic changes and the need for further surgery. Total wrist arthrodesis offered fair results with occasional pain in the follow-up. Overall, this review emphasizes the importance of timely treatment for optimal outcomes in perilunate injuries.
Massoud and Naam treated 19 male patients with chronic perilunate injuries using ORIF, with the mean time from injury to surgery being 29 weeks.[6] The study revealed that most patients experienced favorable outcomes despite the delayed intervention. Postoperatively, the average pain scores were low during rest, daily activities, and manual work, with no significant differences between those with PLDs and those with PLFD.
Functionally, the active extension and flexion of the wrist averaged 39% and 52% of the uninjured side, respectively, and grip strength averaged 87% of the uninvolved extremity. According to the Mayo wrist scoring system, 58% of the patients achieved good to excellent results, with a higher success rate observed in those with fracture dislocations (69%) compared to those with pure dislocations (33%). Notably, 74% of the patients were very satisfied with their outcomes, and 18 out of 19 returned to their original work activities.
This narrative review concludes that ORIF is a valid treatment option for chronic perilunate injuries, yielding satisfactory results despite the delay [Table 1]. However, patients with lesser arc injuries or those with irreducible dislocations and major articular damage may require wrist salvage procedures, as their outcomes tend to be less successful.
| Surgical Approach | Advantages | Disadvantages |
|---|---|---|
| Open Reduction and Internal Fixation (ORIF) | - Effective in restoring carpal alignment and stability - Can be combined with ligament repair or reconstruction - Suitable for both acute and chronic cases. |
- More difficult in delayed cases due to scarring and ligament contraction - Increased risk of residual instability and post- traumatic arthritis in chronic cases. |
| Proximal Row Carpectomy (PRC) | - Effective for pain relief and improving wrist function. - Good option for cases with irreducible scaphoid displacement. - Eliminates the need for ligament repair |
- Limited wrist motion and grip strength postoperatively. -Higher risk of long-term degenerative changes, particularly in younger patients. |
| Wrist Fusion (Arthrodesis) | - Provides permanent pain relief. - Effective in stabilizing the wrist. - Suitable for severe cases with extensive damage to articular surfaces. |
- Loss of wrist motion. - Not suitable for younger patients or those requiring high wrist functionality |
| Bone Retinacular Bone (BRB) Scapholunate Reconstruction | - Useful for addressing dynamic scapholunate instability. -Provides good long-term functional outcomes |
- T echnically demanding. - Risk of graft failure, with some cases requiring revision surgery. |
| Internal Bracing (IB) | - Enhances ligament repair strength. - Allows for early mobilization, reducing stiffness. - Improves outcomes in scapholunate dissociation cases |
-Limited long-term data on efficacy. - Requires precise surgical execution. - Potential for complications if tensioning is not optimal. |
| Staged Reduction and Fixation | - Effective in severely neglected cases. - Allows for gradual reduction of carpal bones, minimizing damage |
- Requires multiple surgical stages, increasing the overall recovery time. - Technically challenging and requires careful monitoring during distraction. |
EMERGING TECHNOLOGIES: 3D PRINTING AND ROBOTICS
The potential of emerging technologies, such as 3D printing and robotics, in managing perilunate injuries is an exciting avenue for future exploration. 3D printing could revolutionize treatment by enabling the creation of patient-specific implants and surgical guides, facilitating more precise and personalized surgical interventions.[26] Robotics, with its enhanced precision and dexterity, could offer significant advantages during complex reconstructive procedures, potentially leading to improved surgical outcomes and reduced complications.[27]
AUTHOR’S PREFERRED APPROACH
The author’s preferred approach for treating neglected PLD and PLFDs is ORIF, particularly when there is no gross carpal instability or proximal migration of the scaphoid bone. For these cases, the scaphoid is typically fixed with a headless compression screw, and the triquetrum is stabilized with K-wires. The author recommends SL ligament reconstruction using suture anchors supplemented with scaphocapitate, SL, and radiolunate K-wires for six weeks. If there is gross instability at the LT joint, the author also stabilizes this joint with K-wires for six weeks. When there is no remnant of the SL ligament on both the scaphoid and lunate, the author prefers BRB reconstruction with two mini-screws, supplemented with conventional K-wires stabilizing the nearby joints as usual.
The author advises against using closed reduction with K-wires alone for certain fractures due to the increased risks of scaphoid non-union, carpal instability, and mid-carpal arthritis [Figure 2]. The author also does not recommend prophylactic CTR for all patients, as the dorsal approach often relieves median nerve compression indirectly. However, the author acknowledges its usefulness in specific scenarios, such as volar LD causing nerve compression, proximal migration of fractured scaphoid or lunate, or when the lunate is inaccessible through a dorsal approach. The author has no experience with staged reconstruction or the use of external fixators as a supplement to ORIF.
The author prefers PRC for cases where the scaphoid is proximally displaced or when SL and LT ligament injuries are irreducible with gross instability [Figure 13]. The author acknowledges having limited experience with wrist fusion. The author strongly emphasizes the importance of early diagnosis and surgical intervention for PLD and PLFD to achieve optimal results. Neglected cases present considerable challenges, but with advancements in ORIF and ligament repair or reconstruction, these approaches offer a viable alternative for managing such injuries.

- A 50-year-old woman presented with a 5-month history of persistent pain, median nerve dysfunction, and stiffness in her right wrist following a fall. (a and b) Radiographs revealed a total volar lunate dislocation. (c and d) Intraoperative findings of irreducibility, instability, and loss of carpal ligaments led to performing a proximal row carpectomy, preserving an intact capitate. The lunate was removed through a dorsal approach, indirectly decompressing the median nerve. The patient achieved a good functional outcome at the 3-year follow-up.
CONCLUSION
Neglected perilunate injuries present a formidable challenge in orthopedic management, often leading to significant long-term complications such as post-traumatic arthritis and functional impairment. The optimal treatment strategy hinges on many factors, including the timing of the injury, the extent of damage, and the patient’s individual needs and expectations. While ORIF, PRC, wrist fusion, and bone retinacular bone graft SL reconstruction all offer potential solutions, their success is intrinsically linked to early diagnosis and intervention.
This review highlights the critical importance of timely and appropriate treatment for perilunate injuries. The high incidence of post-traumatic arthritis and other degenerative changes following neglected injuries serves as a stark reminder of the consequences of delayed care. As our understanding of these injuries continues to evolve, further research is imperative to refine existing treatment algorithms, develop standardized protocols, and explore novel therapeutic approaches.
Future investigations should focus on several key areas to enhance the management of neglected perilunate injuries. Comparative effectiveness studies are needed to directly compare the long-term outcomes of various surgical techniques, providing valuable insights into the most effective treatments. In addition, patient-reported outcomes should be evaluated, emphasizing patient satisfaction, functional outcomes, and quality of life following different treatment modalities. Identifying predictive factors determining the success or failure of specific treatments will allow for more personalized and effective treatment plans. Moreover, exploring novel technologies, such as tissue engineering and regenerative medicine, holds significant promise in advancing the management of these complex injuries. These research areas will contribute to refining treatment strategies and improving patient outcomes.
By addressing these research gaps, we can enhance our ability to provide optimal care for patients with perilunate injuries, ultimately improving their long-term outcomes and quality of life.
Ethical approval
Ethical approval was obtained from the Ethical Committee Board of OHRC, reference number 35/2024, dated July 3, 2024.
Declaration of patient consent
The author certifies that he has obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Conflicts of interest
There are no conflicting relationships or activities.
Financial support and sponsorship: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Late treatment of unreduced perilunate dislocations. J Hand Surg Br. 1999;24:221-5.
- [CrossRef] [PubMed] [Google Scholar]
- Perilunate injury timing and treatment options: A systematic review. J Wrist Surg. 2021;11:164-76.
- [CrossRef] [PubMed] [Google Scholar]
- Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations. J Orthop Trauma. 2008;22:535-40.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic perilunate dislocations treated with open reduction and internal fixation: Results of medium-term follow-up. Int Orthop. 2010;34:1315-20.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome of open reduction of chronic perilunate injuries. J Hand Surg Am. 2012;37:1852-60.
- [CrossRef] [PubMed] [Google Scholar]
- Functional outcome of neglected perilunate dislocations treated with open reduction and internal fixation. Indian J Orthop. 2011;45:427-31.
- [CrossRef] [PubMed] [Google Scholar]
- Staged reduction of neglected transscaphoid perilunate fracture dislocation: A report of 16 cases. J Orthop Surg Res. 2012;20:19.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of trans-scaphoid perilunate fracture dislocations treated by open reduction and internal fixation. BMC Musculoskelet Disord. 2022;31:825.
- [CrossRef] [PubMed] [Google Scholar]
- A novel surgical technique for neglected volar dislocation of the lunate: Cases report and literature review. Orthop Surg. 2023;15:1920-5.
- [CrossRef] [PubMed] [Google Scholar]
- Perilunate dislocations and perilunate fracture dislocations in the U.S. military. J Wrist Surg. 2018;7:57-65.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of three different internal brace augmentation techniques for Scapholunate dissociation: A cadaveric biomechanical study. J Clin Med. 2021;10:1482.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of chronic perilunate dislocations. J Hand Surg Am. 1988;13:206-12.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of bone-retinaculum-bone autograft for scapholunate instability. J Hand Surg Am. 2013;38:504-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment and outcomes of missed perilunate dislocations: A case series. J Wrist Surg. 2023;13:171-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acute median neuropathy and carpal tunnel release in perilunate injuries can we predict who gets a median neuropathy? J Hand Microsurg. 2015;7:237-40.
- [CrossRef] [PubMed] [Google Scholar]
- Proximal row carpectomy for complex perilunate fracture dislocations with migration of proximal scaphoid bone into the forearm. Hand Surg Rehabil. 2021;40:299-304.
- [CrossRef] [PubMed] [Google Scholar]
- Transstyloid perilunate fracture-dislocations of the carpus, a review of two cases. J Hand Microsurg. 2013;5:30-5.
- [CrossRef] [PubMed] [Google Scholar]
- Proximal row carpectomy for chronic unreduced perilunate dislocations. Acta Orthop Belg. 2011;77:765-70.
- [Google Scholar]
- Long-term assessment of proximal row carpectomy for chronic perilunate dislocations. J Hand Surg Am. 1999;24:1231-6.
- [CrossRef] [PubMed] [Google Scholar]
- Scaphoid excision and four-corner fusion for neglected perilunate dislocations: Preliminary results. Hand Surg. 2015;20:280-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acute proximal row carpectomy after complex carpal fracture dislocation. J Hand Microsurg. 2015;7:212-5.
- [CrossRef] [PubMed] [Google Scholar]
- Transscaphoid dorsal lunate dislocation: A case presentation and review of the literature. J Hand Microsurg. 2020;13:238-42.
- [CrossRef] [PubMed] [Google Scholar]
- Open dislocation of the lunate and triquetrum: A case report. J Hand Microsurg. 2024;16:100034.
- [CrossRef] [PubMed] [Google Scholar]
- Hybrid axial ulnar carpal and perilunate dislocation: A case report. J Hand Microsurg. 2015;7:335-9.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of in-hospital 3D printing and practical applications in hand surgery. Biomed Res Int. 2021;2021:4650245.
- [CrossRef] [PubMed] [Google Scholar]
- The future of robotics in hand surgery. Chir Main. 2009;28:278-85.
- [CrossRef] [PubMed] [Google Scholar]






