Translate this page into:
Radial nerve injuries in unrecovered radial nerve palsy associated with humerus fractures
*Corresponding author: J. Terrence Jose Jerome, Department of Orthopaedics, Hand and Reconstructive Microsurgery, Olympia Hospital and Research Centre, Trichy, Tamil Nadu, India. terrencejose@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jerome JTJ, Karunanithi D, Matsui C. Radial nerve injuries in unrecovered radial nerve palsy associated with humerus fractures. J Musculoskelet Surg Res. 2025;9:58-63. doi: 10.25259/JMSR_253_2024
Abstract
Objectives:
The therapeutic management of radial nerve palsy secondary to humerus fractures presents a complex clinical scenario with diverse presentations and treatment approaches. However, there is limited understanding of the specific patterns of unrecovered radial nerve injuries in this context. This study sought to investigate and characterize the spectrum of radial nerve injuries associated with humerus fractures, particularly focusing on cases with persistent palsy.
Methods:
A retrospective analysis was conducted on 20 patients with persistent radial nerve palsy following humerus fractures, who underwent radial nerve exploration and subsequent wrist drop tendon transfers between 2017 and 2023. Functional outcomes were assessed using Jerome’s scoring system.
Results:
The study identified four distinct types of radial nerve injury: Nerve entrapment within the fracture (n = 6), nerve gap (n = 6), nerve crush injury with minimal continuity (n = 5), and nerve adhesions with the plate (n = 3). All patients underwent tendon transfers to address wrist drops. Of these, 16 patients (80%) achieved favorable outcomes, while three exhibited fair outcomes, and one had a poor outcome.
Conclusion:
Untreated radial nerve palsy associated with humerus shaft fractures and definitive radial nerve injury presents a complex clinical scenario, necessitating further investigation and management strategies.
Keywords
Humerus fracture
Nerve palsy
Pattern of nerve injury
Radial nerve
Tendon transfers
Untreated
Wrist drop
INTRODUCTION
The incidence of radial nerve palsy in relation to humerus fractures ranges from 7% to 17%.[1] The treatment for it is still under debate. In a recent systematic review, Ilyas et al.[1] analyzed the expectant treatment, late exploration of the radial nerve (after eight weeks), and early exploration of the radial nerve (within three weeks of injury). Non-surgical treatment led to a spontaneous recovery in 77.2% of cases, while late exploration resulted in 68.1% recovery and early exploration had 89.8% recovery. Many articles have been published on these treatments.[2-4] Furthermore, surgical fixation for humerus fractures through intramedullary nail or plating has increased in recent times.[5,6]
However, little information about non-recovered radial nerve palsies and how they affect nerve injuries is available. If untreated, radial nerve palsy can lead to persistent wrist drop, requiring tendon transfer.[7,8] Jerome et al.[8] developed an outcome score for tendon transfers that evaluate wrist arc of motion (extension/flexion), pronation/supination, metacarpophalangeal (MCP) joint extension and flexion, first web space opening, and pinch and grip strength, comparing these metrics to the uninvolved side. This comprehensive scoring system covers all essential aspects of functional outcome assessment. This article aimed to review the pattern of radial nerve injuries in patients who had humerus fractures with radial nerve palsy and did not undergo nerve exploration.
MATERIALS AND METHODS
Patients, setting, and ethics
There were 156 patients with humerus fractures and radial palsy identified from the Olympia Hospital and Research Center (OHRC) registry between 2017 and 2023. Among them, 136 patients underwent radial nerve exploration. This study is a retrospective analysis of the remaining 20 patients who were managed expectantly (wait and watch) for radial nerve palsy associated with humerus fractures during the same period [Figure 1].
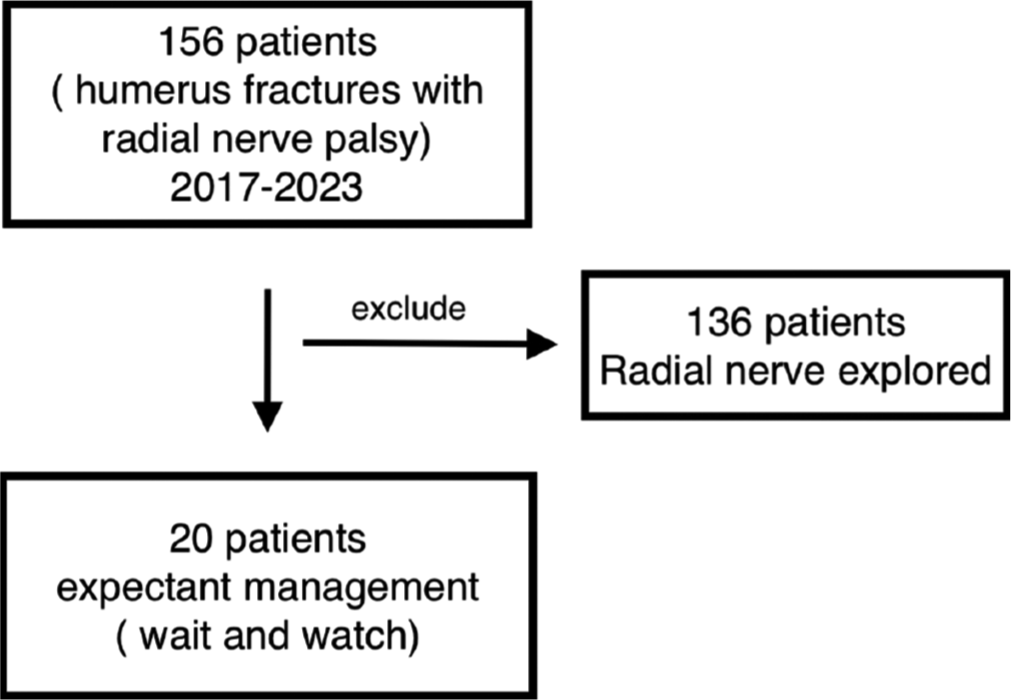
- Selection of patients.
Inclusion criteria
This study included all patients with radial nerve palsy after a humerus fracture who had an expectant line of management (conservative) and surgical fixation of the humerus (open and closed injuries). All these patients developed radial nerve palsy after the fracture.
Exclusion criteria
All patients with radial nerve palsy in humerus fractures who had recovered either by expectant (conservative) treatment or surgical treatment for the nerve were excluded from this study. Patients who underwent surgical exploration involving nerve repair, neurolysis, or nerve grafting were also excluded, as their results are irrelevant to understanding the status of radial nerve injury in long-standing, unoperated, or surgically unexplored cases.
The patient’s demographics, smoking, mechanism of injury, fracture pattern, injury-surgery interval, and intraoperative pattern of nerve injuries were collected from the hospital medical records.
Surgical exploration
Patients undergoing surgical exploration were given supraclavicular block anesthesia. The radial nerve was explored between the brachialis and brachioradialis through a surgical incision in the arm’s lateral aspect. If possible, nerve stimulators were used to look for distal muscle contractions and to identify the pattern of radial nerve damage. Common procedures involved transferring the pronator teres to the extensor carpi radialis brevis, flexor carpi radialis to extensor digitorum communis, and palmaris longus to extensor pollicis longus. The gap was not surgically repaired or bridged using nerve graft cables because the patients presented long after the injury, resulting in inevitable neuromuscular degeneration.
Post-operative care
After the surgery, all patients were given an above elbow cast/splint with the elbow flexed at 90°, forearm pronated, wrist extended at 30°, thumb abducted and extended, and the MCP joint fully extended for two weeks. The sutures were removed after two weeks, and a below-elbow thermoplastic splint was applied for four weeks. During this time, patients continued shoulder and finger interphalangeal joint range of motion exercises and started elbow flexion and extension exercises while extending the wrist and fingers. At six weeks, wrist flexion and extension exercises were started with the fingers extended and the elbow flexed. Muscle retraining was initiated to activate the tendon transfer, and the splints were used at night for up to eight weeks post-surgery before being completely weaned at 12 weeks. After that, full activity was resumed.
Follow-up
Follow-up evaluations were conducted using the Jerome et al.[8] outcome score based on the simplified grade from the value of wrist arc of motion (wrist extension/flexion), pronation/supination, MCP extension and flexion, first web space opening, and pinch and grip strength compared with the uninvolved side [Table 1].
| Grade | Wrist arc of motion, pronation/supination, MCP joint extension, MCP flexion, first web space opening, pinch and grip strength |
|---|---|
| Good | >75% of contralateral side |
| Fair | 50–75% |
| Poor | <50% |
MCP: Metacarpophalangeal
Statistics
The data were analyzed using Centers for Disease Control and Prevention Epi Info software and expressed as mean and standard deviation. Fisher exact tests were used to compare categorical variables, and Mann–Whitney U tests were used to compare differences between two independent groups distributed as ordinal or continuous variables. A P = 0.05 or less was considered significant.
RESULTS
Patients and characteristics
The study found that the average age of participants was 36 years, ranging from 21 to 43. Four types of radial nerve injuries were observed [Figures 2-6]. The radial nerve was either entrapped in the fracture (n = 6), had a gap (n = 6), was crushed with minimal continuity (n = 5), or had adhesions with the plate (n = 3). The average time between injury and surgery was 74 months, ranging from 8 to 120 months [Table 2].
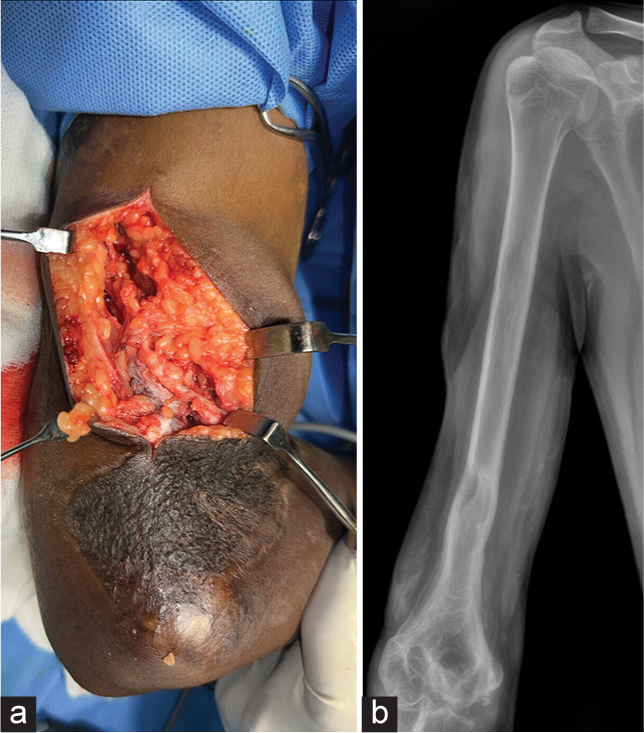
- (a, b) The gap pattern of nerve injury is seen in the humerus fractures.
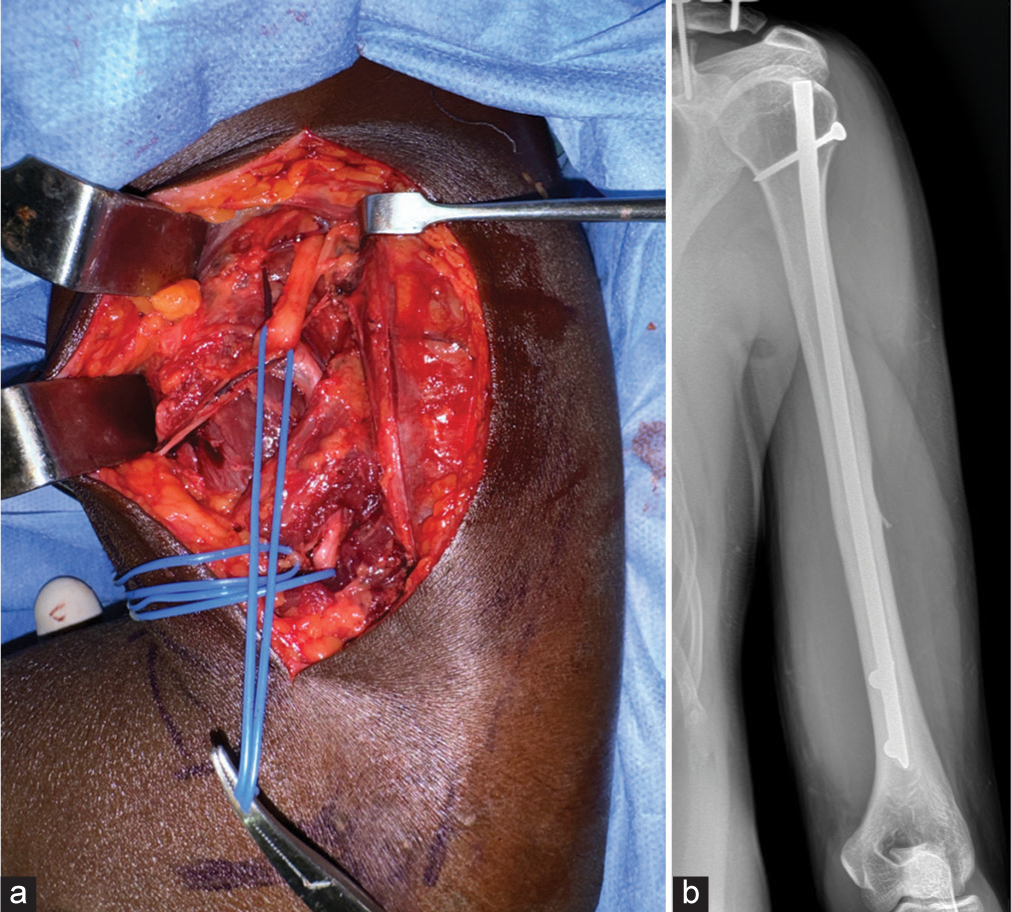
- (a, b) The crushed pattern of nerve injury seen in the humerus fractures has few fascicles in continuity.
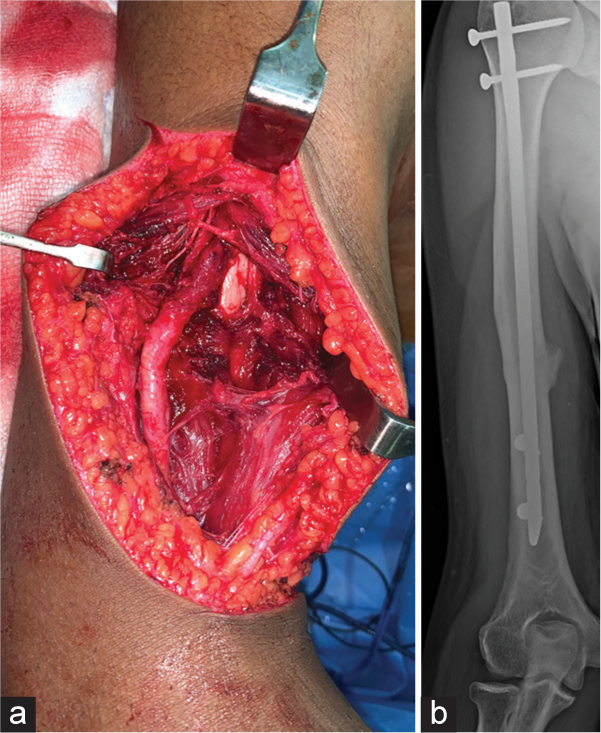
- (a, b) The entrapped pattern of nerve injury is seen in the humerus fractures that appear thickened and contused at the entrapment site.
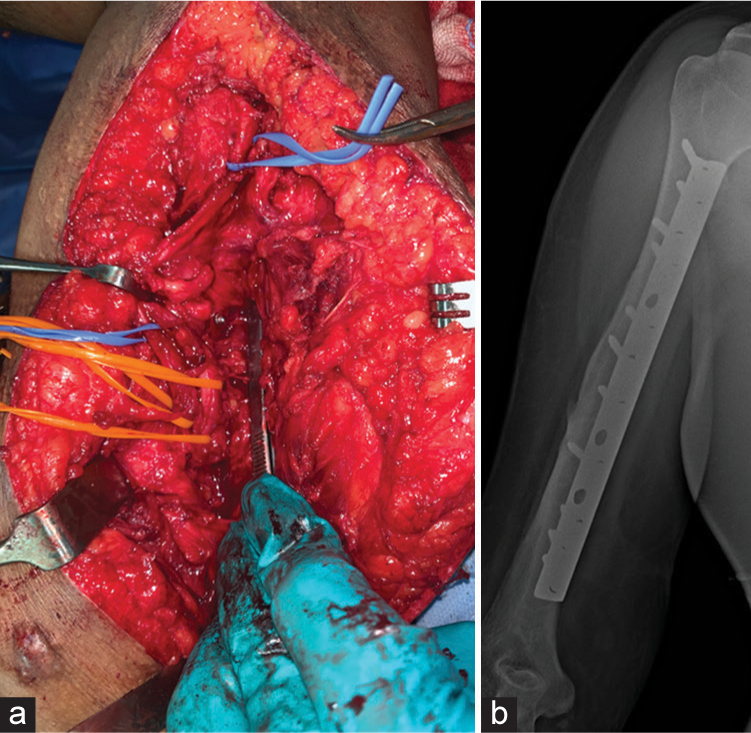
- (a, b) The plate adhesion pattern of nerve injury is seen in the humerus fractures.
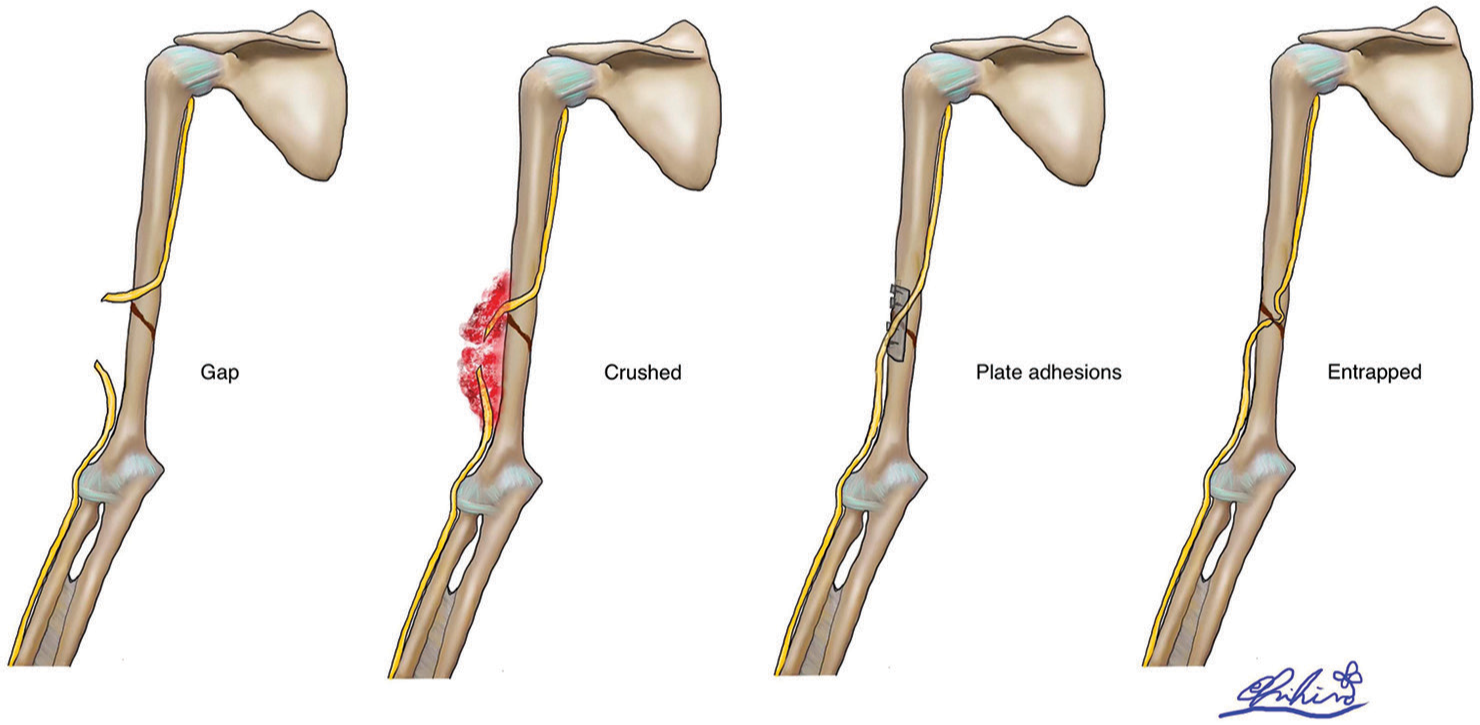
- The illustration depicts the four different patterns of radial nerve injury seen in our study.
| Mechanism of injury | |
| RTA | 11 |
| Fall | 8 |
| Machine belt | 1 |
| Injury | |
| Closed | 15 |
| Open | 5 |
| Location | |
| Midshaft | 9 |
| Distal | 11 |
| Fracture | |
| Transverse | 10 |
| Spiral | 5 |
| Oblique | 5 |
| Treatment | |
| IMN | 6 |
| Plating and screw | 8 |
| Conservative | 5 |
| External fixator | 1 |
RTA: Road traffic accident, IMN: Intramedullary nail
All patients with distal humerus fractures (n = 11) had a posterior approach, while those with midshaft fractures (n = 9) had an anterior approach. None of the patients had radial nerve exploration. Among the 20 patients, 15 had closed humerus fractures and five had open fractures. The main reasons for the delay in surgery were surgeons preferring non-operative treatment for 15 patients and five patients opting against surgery themselves.
Only six patients had electrophysiological studies performed at various intervals after their injury. All of these patients demonstrated severe axonal loss, absent or reduced compound muscle action potential, fibrillation potentials, and positive sharp waves.
Outcomes
In terms of outcomes, the participants were followed up for an average of 24 months, with a range of 10–56 months. Of the 20 patients, 16 (80%) achieved a good score, three achieved a fair score, and only one had a poor score. Age, sex, side, smoking, and treatment delay did not significantly impact the functional outcome [Table 3]. The only patient who had a poor outcome did not follow the regular therapy protocol. There were no significant complications among any of the patients.
| Factors | Value/mean | P-value |
|---|---|---|
| Age | 36 | 0.9b |
| Gender | ||
| Male | 17 | 0.1a |
| Female | 3 | |
| Side | ||
| Left | 8 | 1.0a |
| Right | 12 | |
| Smoker | ||
| Yes | 4 | 1.0a |
| No | 16 | |
| Time injury-surgery | 74 | 0.9b |
DISCUSSION
The studies by Ilyas et al.[1] and Schoch et al.[5] indicate that in cases of humeral shaft fractures, surgeons often opt for a wait-and-see approach regarding radial nerve recovery, with a good recovery observed in 77% of cases. However, 23% of cases did not recover under expectant management, and the outcomes for these patients remain unclear. The authors aimed to analyze the natural progression and status of radial nerves in patients with humeral fractures who experienced persistent palsy. This rationale led to exploring the radial nerve in our series, which spanned from 8 to 120 months.
There is also a common question about how this article improves clinical outcomes in unexplored or non-operated radial nerve palsies with wrist drops. This article highlights that 23% of cases will invariably develop irrecoverable radial nerve palsy, indicating a need for improved management strategies. It recommends that surgeons perform early nerve exploration, as documented by Ilyas et al.[1] in their systematic review.
The strength of this article lies in exploring the radial nerve in 20 patients who had not recovered from radial nerve palsy on expectant management. Four different patterns of radial nerve injuries were observed, including entrapped, crushed, gap, and plate adhesions. At present, there are no studies on this pattern of nerve injury, and the authors highlighted its significance in unrecovered radial palsy.
Our study’s mean interval from injury to surgery was 74 months (8–120 months). The spontaneous nerve recovery in an expectant approach after the humerus fracture is 8.29 weeks to 4.91 months.[1] All operated patients in our series (n = 15) had no radial nerve exploration or nerve recovery. Five non-operated cases managed conservatively also had no nerve recovery. Therefore, this made us explore the radial nerve and understand the pattern of nerve injuries that did not recover. This may also help the readers to introspect that these patients would have done better had they been intervened. Ilyas et al.[1] reported that radial nerve exploration within three weeks in a total and primary radial nerve palsy associated with humerus fractures recovered completely in 87–90% of cases. This recovery rate is better and may be considered acceptable than expectant or wait-and-watch management, which reported 77% recovery.
This article conveys two strong messages:
Four patterns of nerve injuries have led to non-recovery, which might have been managed differently with better outcomes
Exploration is preferable; even if it results in a scar, it is still more favorable than multiple tendon transfers.
This article raises two important questions:
Should all radial nerve palsy cases associated with humerus fractures be explored?
Can patients with neglected radial nerve palsy caused by medical intervention be classified as having iatrogenic neglected radial nerve palsy?
While we do not have answers to these questions, they remind us to be vigilant and practical when approaching radial nerve palsy.
The study’s limitations include that most patients underwent inadequate electrophysiological studies following radial nerve palsy. Among the few who did (n = 6), the results indicated axonotmesis or neurotmesis, offering limited information for correlating electrophysiological findings with outcomes in expectantly managed, unrecovered radial nerve palsies. In addition, the study’s small sample size and retrospective design further limit its conclusions. Nonetheless, the study underscores the importance of a more holistic approach to managing this type of injury to prevent the consequences of persistent palsy in an injured, unrecovered nerve.
CONCLUSION
This study highlights the significant impact of radial nerve injury on humerus fracture outcomes, emphasizing the need for early intervention. A significant proportion of patients (1 in 5) experience persistent palsy, often requiring multiple tendon transfers. While the ideal timing for surgical exploration remains debated, our findings suggest that early exploration, guided by clinical and neurophysiological assessments, may lead to superior functional outcomes compared to expectant management. The treating surgeon plays a crucial role in navigating the complexities of decision-making in these cases. Multiple tendon transfers offer a viable solution for restoring function, with outcomes effectively assessed using Jerome’s score. Early intervention in radial nerve palsy associated with humerus fractures is paramount to optimize patient outcomes and minimize the need for complex reconstructive procedures.
AUTHORS’ CONTRIBUTIONS
JTJJ: Conceptualization, Methodology/Study design, Software, Validation, Formal analysis, Investigation, Resources, Data curation, Writing – original draft, Writing – review and editing. DK and CM: Visualization, drawing, Supervision, Project administration. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Ethical approval was obtained from the Ethical Committee Board of OHRC, reference number 03/2024, dated 3rd May 2024.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Radial nerve palsy recovery with fractures of the humerus: An updated systematic review. J Am Acad Orthop Surg. 2020;28:e263-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radial and ulnar nerve palsies in closed humerus fracture: A case report and literature review. J Musculoskelet Surg Res. 2023;7:298-301.
- [CrossRef] [Google Scholar]
- Multiple (median, ulnar, radial and medial antebrachial) nerve injury associated with brachioplasty. J Hand Microsurg. 2020;12(Suppl 1):S78-80.
- [CrossRef] [PubMed] [Google Scholar]
- Iatrogenic nerve injuries in orthopaedics. J Musculoskelet Surg Res. 2019;3:9-14.
- [CrossRef] [Google Scholar]
- Humeral shaft fractures: National trends in management. J Orthop Traumatol. 2017;18:259-63.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of nerve reconstruction for radial nerve injuries based on the level of injury in 244 operative cases. J Hand Surg. 2010;35:385-91.
- [CrossRef] [PubMed] [Google Scholar]
- Les transferts palliatifs de réanimation de l'extension du poignet et des doigts. A propos de 14 transferts pour paralysie radiale et dix transferts pour lésion plexique [Palliative tendon transfer for reanimation of the wrist and finger extension lag. Report of 14 transfers for radial nerve palsies and ten transfers for brachial plexus lesions] Chir Main. 2002;21:13-22.
- [CrossRef] [PubMed] [Google Scholar]
- Flexor digitorum superficialis tendon transfer to extensor pollicis longus in the absence of palmaris longus tendon: A wide-awake anaesthesia approach. Eur J Plast Surg. 2024;47:44.
- [CrossRef] [Google Scholar]






