Translate this page into:
What about burnout syndrome among orthopedic surgery residents in Abidjan (Côte d’Ivoire)?
*Corresponding author: Dr. Hermann Victoire Feigoudozoui, Department of Orthopaedic and Trauma Surgery, Félix Houphouët-Boigny University, Abidjan, Cote D’Ivoire. hfeigoudozoui@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Feigoudozoui H, Parteina D, Mapouka M, Koné S. What about burnout syndrome among orthopedic surgery residents in Abidjan (Côte d’Ivoire)? J Musculoskelet Surg Res. 2025;9:84-9. doi: 10.25259/JMSR_274_2024
Abstract
Objectives:
The objectives of the study are to describe the etiologies and the effects and propose how to prevent burnout syndrome (BOS) in orthopedic surgery residents (OSRs) in Abidjan, Côte d’Ivoire.
Methods:
This analytical cross-sectional study took place in May 2023. Fifty-eight OSRs, including six (10%) females, each answered a questionnaire distributed to all OSRs in Abidjan. The average age was 33.8 years old (Ranging 27–43). The anonymous questionnaire included the Maslach Burnout Inventory assessment.
Results:
Nine (15%) OSRs had a high degree of BOS, 13 (22%) had a loss of empathy, and six (10%) had a high degree of personal accomplishment. We found an increase in the frequency of the symptoms of BOS in OSRs in Abidjan, Côte d’Ivoire.
Conclusion:
BOS is a real public health problem among OSRs in Abidjan. However, burnout does not attract, and its consequences can have repercussions on the quality of work. It seems to impact some resident’s training negatively. It is imperative to implement preventive actions.
Keywords
Africa
Burnout
Côte d’Ivoire
Maslach burnout inventory
Orthopedic surgery
Residents
Young surgeons
INTRODUCTION
Burnout is a state of physical and emotional exhaustion and a sense of low personal accomplishment that may impact efficiency at work.[1] It is a syndrome of physical and emotional exhaustion involving the development of self-deprecation and negative professional attitudes, as well as a loss of involvement and feeling for customers.[2] The phenomenon of burnout has existed for as long as man has worked and has been given various names throughout the ages.[3] The attention given to this condition is justified by its consequences and damage to health.[4]
This syndrome can negatively impact professionals’ quality of life, both psychologically and physically.[5] All professions are affected, especially those with a social or community focus.[4,6,7] Any worker may experience burnout syndrome (BOS) during his/her career.[2] The medical profession is highly stressful, and the chronic stress associated with it can lead to BOS, with a deleterious effect on the quality of care.[8,9]
For doctors in training, this syndrome is even more pronounced, as it complements the pre-existing stress of their studies. In Abidjan, hospital practitioners are aware of the existence of BOS but do not pay enough attention to it. We have observed an increasing number of symptoms of professional exhaustion among orthopedic surgery residents (OSRs) in Abidjan. BOS has become a particularly worrying pathology among OSRs in Abidjan, with a tangible on the quality of care.[10] In the whole of Côte d’Ivoire, from a medical point of view, it is only in the university hospital of Bouake, the country’s third largest city, that an observational study has been carried out among healthcare professionals in the pediatric department. This cross-sectional, descriptive study found a prevalence of 56% among a population of 78 staff interviewed.[10] To date, no study has been carried out to describe the various aspects and prove the existence of BOS in OSRs in Abidjan. We conducted this study for the first time because it is essential to document the epidemiological data confirming the existence, etiological factors, different manifestations, and consequences of professional exhaustion among OSRs in Abidjan, Côte d’Ivoire.
This study aimed to describe BOS’s etiologies, effects, and consequences in OSRs in Abidjan, Côte d’Ivoire.
MATERIALS AND METHODS
This cross-sectional study was carried out over 1 month in the OSRs in Abidjan, Côte d’Ivoire. Of the 67 doctors included, nine had not consented to the survey and were excluded. Fifty-eight OSRs were selected, including 52 males and 6 females with an average age of 33.8 years (ranging from 27 to 43). We used an individual, anonymous survey form written in French, the official language in Côte d’Ivoire. The survey form considered aspects of the student life of OSRs in Côte d’Ivoire, namely sex, work schedules, possible harassment situations, and the family life conditions of OSRs. Each participant completed his/her survey form, which took no more than a few minutes to complete. The survey form and the interests of the study were explained to them to obtain their consent. This form included the Maslach Burnout Inventory (MBI). The MBI is the reference instrument for measuring BOS for medical personnel.[6,11] Maslach also described the main manifestations as professional exhaustion, depersonalization, loss of empathy, and diminished or lost personal accomplishment.[1,2]
The series grouped interns and residents together under the name OSR. Those at the start of their internship and those who had not consented were excluded.
All data were compiled and analyzed using Epi Info software. Statistical tests were performed using Person’s Chi-square with a significance threshold of 95% and a probability for which a value of <0.05 was considered significant. If the Chi-square test was invalid, Fisher’s exact test was performed. The anonymous survey form, which we gave individually to each OSR, was filled out enthusiastically and with peace of mind.
RESULTS
Our study included 58 OSRs from Abidjan out of 67 (86.5%). The sample was representative, but eight OSRs did not consent and were excluded. This exclusion, representing 13.5% of the population, may have led to a selection bias. This did not allow us to be even more convincing in our statistical test outcomes.
Thirty-one (53%) participants practiced leisure activities. Concerning workload, 20 (34%) OSRs worked between eight and 45 h weekly, and 38 (65%) worked over 45 h weekly. OSRs participated in an average of 4.5 on-call month shifts in their respective departments. We also found that workplace harassment is one of the etiological factors associated with BOS among OSRs in Abidjan. Thirteen (22%) doctors were harassed at work, and six (10%) did not wish to comment on harassment at work.
The overall analysis of the outcomes according to the MBI was exposed in Figure 1. Of the 15 (25%) OSRs concerned by the burnout score (Professional Exhaustion Score [PES]), nine (15%) had it to a high degree. Of the 25 (43%) OSRs affected by depersonalization/loss of empathy score (DS), 13 (22%) had a high degree. Of the 18 (31%) ORSs with personal accomplishment scores (PAS), six (10%) had a high degree.
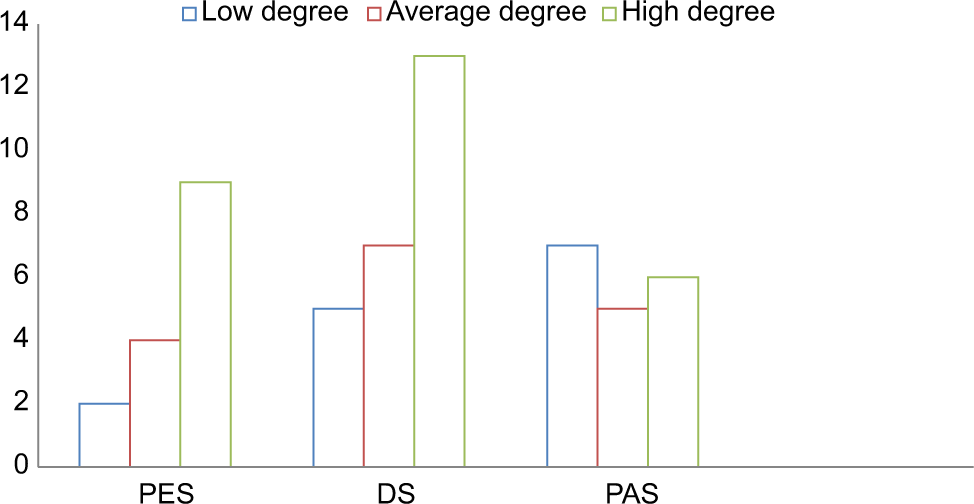
- Results of MBI score. MBI: Maslach burnout inventory, PES: Professional exhaustion score, DS: Depersonalization/loss of empathy score, PAS: Personal accomplishment score.
Statistical analyses had established that the occurrence of BOS signs was also related to sex [Table 1]. Of the 15 (25%) OSRs concerned by PES, nine (15%) had it to a high degree. The Fisher’s exact test was significant at 0.0051. Of the 25 (43%) OSRs concerned by DS, thirteen (22%) had a high degree. The Fisher test was significant at 0.0331. Of the 18 (31%) OSRs concerned by PAS, six (10%) males had a high degree. The Fisher test was significant at 0.0313.
| Items | Male | Female | Total | P-value |
|---|---|---|---|---|
| PES | 0.0051 | |||
| Low level | 1 | - | 1 | |
| Moderate level | 4 | - | 4 | |
| High level | 7 | 2 | 9 | |
| Total | 14 | |||
| DS | 0.0331 | |||
| Low level | 5 | - | 5 | |
| Moderate level | 7 | - | 7 | |
| High level | 9 | 4 | 13 | |
| Total | 25 | |||
| PAS | 0.0313 | |||
| Low level | 8 | - | 8 | |
| Moderate level | 5 | - | 5 | |
| High level | 6 | - | 6 | |
| Total | 19 | |||
| Total | 52 | 6 | 58 |
PES: Professional exhaustion score, DS: Depersonalization/loss of empathy score, PAS: Personal accomplishment score
Personal exhaustion had four types of impact on the OSR. These repercussions [Table 2] were as follows: 13 (22%) OSRs had acknowledged having already committed a medical error, six (10%) OSRs already had suicidal thoughts, 33 (56%) OSRs were not satisfied with their salary, and 29 (36%) OSRs were unwilling to recommend their profession to their friends and family.
| Items | n(%) |
|---|---|
| Medical errors | |
| Yes | 13 (22) |
| No | 34 (58) |
| No opinion | 11 (18) |
| Total | 58 |
| Suicidal ideals | |
| Yes | 6 (10) |
| No | 52 (89) |
| Total | 58 |
| Salary satisfaction | |
| Satisfied | 11 (18) |
| Dissatisfied | 33 (56) |
| Indifferent | 14 (24) |
| Total | 58 |
| Recommendation for the medical profession | |
| OSR who wished to recommend | 37 (63) |
| OSR who did not wish to recommend | 21 (36) |
| Total | 58 |
OSR: Orthopedic surgery resident
Statistical analysis also revealed that a lack of leisure activities could cause the onset of BOS signs [Table 3]: Of the nine (15%) OSRs who had suffered from it to a high degree, only two (3%) practiced a leisure activity. The Fisher test was not significant at 0.3123. Of the 13 (22%) OSRs who had suffered from it greatly, only two (3%) practiced a leisure activity. The Fisher test was not significant at 0.1905. Eighteen (31%) OSRs had suffered to a high degree, and only one (1%) practiced a leisure activity. The Fisher test was not significant at 0.6669.
| Items | Yes | No | Total | P-value |
|---|---|---|---|---|
| PES | 0.3123 | |||
| Low level | - | 1 | 1 | |
| Moderate level | - | 4 | 4 | |
| High level | 2 | 7 | 9 | |
| Total | 14 | |||
| DS | 0.1905 | |||
| Low level | 1 | 4 | 5 | |
| Moderate level | - | 7 | 7 | |
| High level | 2 | 11 | 13 | |
| Total | 25 | |||
| PAS | 0.6669 | |||
| Low level | - | 8 | 8 | |
| Moderate level | - | 5 | 5 | |
| High level | 1 | 5 | 6 | |
| Total | 19 | |||
| Total | 6 | 52 | 58 |
PES: Professional exhaustion score, DS: Depersonalization/loss of empathy score, PAS: Personal accomplishment score
Statistical analysis outcomes have shown that working more than 20 h/week could be the cause of the onset of BOS signs [Table 4]: Out of 15 (25%) OSRs concerned by PES, an accumulation of working hours between 20 and 45 h/week was the cause of BOS in two (3%) cases. Cumulative working hours of more than 45 h a week were the cause of PES in seven (12%) cases. The Fisher test was not significant at 0.369. An accumulation of working hours between 20 h and 45 h a week was the cause of DS in two (3%) cases. Cumulative working hours of more than 45 h a week were the cause of DS in 11 (18%) cases. The Fisher test was significant at 0.01575. Out of 18 (31%) OSRs concerned by PAS. An accumulation of working hours between 20 h and 45 h a week was the cause of PAS in one (1%) case. Cumulative working hours of more than 45 h a week were the cause of PAS in five (8%) cases. The Fisher test was significant at 0.03547.
| Items | 20–45 h | >45 h | Total | P-value |
|---|---|---|---|---|
| PES | 0.3690 | |||
| Low level | 1 | - | 1 | |
| Moderate level | - | 4 | 4 | |
| High level | 2 | 7 | 9 | |
| Total | 14 | |||
| DS | 0.01575 | |||
| Low level | 4 | 1 | 5 | |
| Moderate level | 2 | 5 | 7 | |
| High level | 2 | 11 | 13 | |
| Total | 25 | |||
| PAS | 0.03547 | |||
| Low level | 7 | 1 | 8 | |
| Moderate level | 1 | 4 | 5 | |
| High level | 1 | 5 | 6 | |
| Total | 19 | |||
| Total | 20 | 38 | 58 |
PES: Professional exhaustion score, DS: Depersonalization/loss of empathy score, PAS: Personal accomplishment score
Workplace harassment would also be one of the causes of the onset of BOS signs [Table 5]: For the nine (15%) OSRs that had presented a high degree of PES, workplace harassment was the cause in one (1%) case. Two (3%) OSRs did not comment on harassment at work. The Fisher’s exact test was insignificant at 0.3663. For the 13 (22%) OSRs with a high degree of DS, harassment at work was the cause in nine (15%) cases. Two (3%) OSRs did not comment on harassment at work. Fisher test was insignificant at 0.1002 for the six (10%) OSRs, with a high degree of PAS harassment at work as the cause in four (6%) cases. One (1%) OSR did not comment on harassment at work. The Fisher test was not significant at 0.1536.
| Items | Yes | NOP | No | Total | P-value |
|---|---|---|---|---|---|
| PES | 0.3663 | ||||
| Low level | - | - | 1 | 1 | |
| Average level | - | - | 4 | 4 | |
| High level | 1 | 1 | 7 | 9 | |
| Total | 14 | ||||
| DS | 0.1002 | ||||
| Low level | - | 1 | 4 | 5 | |
| Average level | - | - | 7 | 7 | |
| High level | 9 | 2 | 2 | 13 | |
| Total | 25 | ||||
| PAS | 0.1536 | ||||
| Low level | - | - | 8 | 8 | |
| Average level | - | - | 5 | 5 | |
| High level | 4 | 1 | 1 | 6 | |
| Total | 18 | ||||
| Total | 14 | 5 | 39 | 58 |
PES: Professional exhaustion score, DS: Depersonalization/loss of empathy score, PAS: Personal accomplishment score, NOP: Abstention
DISCUSSION
However, we found that some OSRs we interviewed did not feel they took the BOS seriously.[12] This is even though it is a real psychic problem that is widespread in almost all medical professions.[1,4,6] However, we found a high prevalence (57%) of BOS among OSRs in Abidjan (Côte d’Ivoire). In general, the incidence of severe BOS among physicians varies from 5% to 40%. This rate had approached 80% in internal medicine residents.[4,13] In Oman, Al Subhi et al. have found a 16% prevalence of BOS among all residents of different specialties.[1] BOS prevalence varies from country to country, depending on the working conditions and organizations.
Our study analyzed the repercussions of personal exhaustion in OSRs, the proportions of which are described in Table 1. These repercussions concerned medical errors (13%), suicidal ideation (10%), salary dissatisfaction (56%), and non-recommendation of the profession (36%). Like some others, we thought that these were essentially the busiest doctors in terms of workload.[4,14-19] Table 4 shows this. However, other studies show no link between BOS and work overload.[19,20]
The MBI outcomes are shown in Figure 1. In addition to workload, depersonalization could be explained by difficult working conditions and the stress of studying. Gueye et al. in Senegal also point to difficult learning conditions, which they claim are more marked than in France.[21] However, unlike our study, they found a low rate of personal fulfillment (84.9%), much higher than those suffering from emotional exhaustion (64%) and depersonalization (45.2%).[21] However, these two studies examined BOS in junior doctors in West Africa.
In our study, males were more affected [Table 1] than females.[9] This may be explained by the high proportion of males in the specialty and the study.[11,12,19] No link has been demonstrated between sex and the occurrence of BOS.[20,22] Other authors have found that females are most affected.[14,18] The role of sex in the occurrence of BOS is frequently debated in the literature on the subject.[23]
The doctors surveyed did not engage in enough leisure activities. Yet leisure activities are seen as a means of preventing BOS.[3,16,23,24] Maslach argues that having leisure time alongside work can correspond to a change of tasks for the doctor.[2] Hobbies are potentially very conducive to personal fulfillment, enabling people to return to work with greater energy and pleasure and to put professional difficulties into perspective.[20] A significant link (P < 0.005) has been demonstrated between the absence of leisure activities and the onset of severe BOS.[14] Not knowing or not being able to take time for oneself is the primary disturbance in BOS.[25]
Finally, psychological harassment by seniors played an essential role in the occurrence of BOS in our study. Harassment in its various forms was experienced as an oppressive situation by the participants in this study. It is clear to conclude that this factor is closely linked to BOS. Faivre et al. found that 28% of participants reported having experienced harassment.[19] They call it a manifestation of suffering.
Limitations of the study
Furthermore, as other authors have done, our work did not study the doctor-patient relationship. In Côte d’Ivoire, there are two public universities where OSRs are trained. Our study could only include OSRs from one of the two universities because the other university is in another town. We were unable to obtain permission from the department head.
CONCLUSION
BOS exists among orthopedic residents in this study. It appears to have negatively impacted the training and efficiency of some residents. Work overload, lack of seizure, and harassment were the main factors identified. Preventive action is imperative.
RECOMMENDATIONS
BOS exists among OSRs in Côte d’Ivoire. Nowadays, the causes are well known: A predominance of males, lack of regular leisure activities, working more than 45 h a week, and harassment in the workplace. All we need to do is avoid these etiologies and make work more adaptive.
Based on these etiologies, we have formulated a few suggestions to help reduce or even completely avoid BOS in OSRs:
Work schedules must be strictly respected.
On-call rest periods should start at 8 a.m. the next day and last a minimum of 24 h. The night shifts usually last an average of 34 h (from 8 a.m. to 6 p.m. the next day).
OSRs need to be able to take their legally prescribed annual leave.
Orthopedic surgery departments must organize leisure outings at least once a quarter.
Young OSRs must not be considered “robots ready to do everything at all times.” This can contribute to physical and mental exhaustion.
Monthly remuneration should be increased and paid regularly basis. This will encourage OSRs and enable them to take pride in and enjoy their work.
We would like to state that these are suggestions only and do not constitute institutional instructions, and they are not exhaustive.
ACKNOWLEDGMENTS
The authors would like to thank all the staff who contributed to the management of this article.
AUTHORS’ CONTRIBUTIONS
HVF and DP conceived and designed the study, conducted research, provided research materials, and collected and organized data. MM analyzed and interpreted data. HVF wrote the initial and final draft of the article and provided logistic support. SK corrected the list version of the article and supervised. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The study was approved by the Institutional Ethics Committee at Felix Houphouet-Boigny University, number 10129/2024.R, dated October 7, 2024.
DECLARATION OF PARTICIPANT CONSENT
The authors certify that they have obtained all appropriate participant consent forms. In the form, the participants have given their consent for their images and other clinical information to be reported in the journal. The participants understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Prevalence of burnout of residents in Oman medical specialty board: A cross-sectional study in Oman. J Musculoskelet Surg Res. 2020;4:136-40.
- [CrossRef] [Google Scholar]
- Clinical manifestations of burnout in physicians. Sante Ment Que. 1985;10:145-50.
- [CrossRef] [PubMed] [Google Scholar]
- Burnout syndrome among generalist medical doctors Douala region (Cameroon): Can physical activities be a protective factor? Rev Med Brux. 2017;38:10-5.
- [Google Scholar]
- A meta-analysis of job burnout using the MBI scale. Encéphale. 2007;33:947-53.
- [CrossRef] [PubMed] [Google Scholar]
- Burnout syndrome and associated factors among physicians in two University Hospitals in Antananarivo. Pan Afr Med J. 2018;31:63.
- [Google Scholar]
- To suffer to heal: Burn out among doctors working in palliative care. The letter from the oncologist. 2004;. ;13:64-75.
- [Google Scholar]
- Burnout in French doctors: A comparative study among anaesthesiologists and other specialists in French hospitals (SESMAT study) Ann Fr Anesth Reanim. 2011;30:782-94.
- [CrossRef] [PubMed] [Google Scholar]
- Job stress and burnout in hospital employees: Comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4:e004185.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and factors associated with burnout syndrome among health personnel in the pediatric department of the University Hospital of Bouake (Côte d'Ivoire) Rev Int Med (Abidj). 2023;5:175-80.
- [Google Scholar]
- Burnout syndrome among orthopedic surgery residents in Saudi Arabia: A multicenter study. J Muskuloskelet Surg Res. 2019;3:184-8.
- [CrossRef] [Google Scholar]
- The journey of orthopaedic surgery from residency to fellowship: A cross-sectional study in the Gulf Cooperation Council countries. J Taibah Univ Med Sci. 2019;14:131-8.
- [CrossRef] [PubMed] [Google Scholar]
- Burnout, patient compliance and psychological withdrawal among GPs: An exploratory study. Encéphale. 2011;37:48-53.
- [CrossRef] [PubMed] [Google Scholar]
- Burnout among Tunisian medical residents: About 149 cases. Encéphale. 2018;44:337-42.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of burnout syndrome among doctors in training at the Ibn Rochd University Hospital, Casablanca. Pan Afr Med J. 2017;27:243.
- [CrossRef] [Google Scholar]
- Career choice among resident physicians at Mohamed VI University Hospital of Marrakech: Impact factors and proposal for innovative practices. Rev Int Sci Gestion. 2020;3:423-47.
- [Google Scholar]
- Burnout syndrome in orthopaedic and trauma surgery residents in France: A nationwide survey. Rev Chir Orthop Trauma. 2018;104:855-9.
- [CrossRef] [PubMed] [Google Scholar]
- Burn-out among young doctors: A study conducted in the Sousse region. Ann Med Psycho. 2016;175:332-8.
- [CrossRef] [Google Scholar]
- Burnout syndrome among students in specialization at the University Hospital of Dakar (Senegal) Ann Med Psycho. 2016;174:551-6.
- [CrossRef] [Google Scholar]
- Burnout-associated factors in anesthesia and intensive care medicine 2009 survey of the French Society of anesthesiology and intensive care. Ann Fr Anesth Reanim. 2013;32:175-88.
- [CrossRef] [PubMed] [Google Scholar]
- Rates of medication errors among depressed and burnout residents: Prospective cohort study. BMJ. 2008;336:488-91.
- [CrossRef] [PubMed] [Google Scholar]
- The burnout syndrome of the caregiver. Presse Med. 2004;33:394-8.
- [CrossRef] [PubMed] [Google Scholar]
- Objective and quantitative analysis of daytime sleepiness in physicians after night duties. Int J Psychophysiol. 2009;72:307-13.
- [CrossRef] [PubMed] [Google Scholar]







