Translate this page into:
A Case of proximal humeral physeal separation in a newborn: Is internal fixation justified?
2 Department of Orthopaedic Surgery, Faculty of Medicine, Ain-Shams University, Cairo, Egypt
Corresponding Author:
Khalid Nabil Youssef
Department of Orthopaedic Surgery, Faculty of Medicine, Ain-Shams University, 11591 Abbasia, Cairo
Egypt
k_n_y_3@yahoo.com
| How to cite this article: Amen JF, Youssef KN. A Case of proximal humeral physeal separation in a newborn: Is internal fixation justified?. J Musculoskelet Surg Res 2019;3:231-234 |
Abstract
We aim to investigate the clinical and radiologic outcome of conservative management in a newborn with proximal humeral physeal separation (PHPS) on the intermediate term. PHPS is rare and occur typically in newborns. In general, the prognosis is satisfactory. The largest series of PHPS in neonates used routine open reduction and internal fixation for management. We treated a newborn girl with a severe PHPS conservatively with excellent intermediate-term results. The remodeling potential of the proximal humerus in neonates allows for conservative treatment. Closed reduction or operative fixation is not routinely justified. Based on the results of this case and the current literature, we caution against the potential hazards of overtreatment in such patients.Introduction
The physeal injury of the proximal humerus is rare, and many surgeons have little experience with this type of injury. Fractures of the proximal humerus represent approximately 0.45% of all pediatric fractures. Proximal humeral physeal separations (PHPSs) represent 3% of all physeal injuries, which represent about one-third of all pediatric fractures.[1],[2] Isolated epiphyseal separation is rare and occurs typically in newborns and toddlers.[3]
Treatment of such physeal separation is usually conservative, with immobilization for several weeks. In general, remodeling potential is enormous and the prognosis for adequate healing is excellent.[4],[5],[6] The largest and most recently reported series for such entity of injuries in neonates used routine open reduction and Kirschner wire fixation for management following failed attempts of closed reduction.[7]
We assume that separation of the proximal humeral epiphysis in neonates due to birth trauma is a benign injury that yields excellent results with conservative management. This case report assesses the functional and radiologic outcome of conservative management in such an injury on the intermediate term. We aim to emphasize the clinical significance of the satisfactory remodeling potential of newborns in the event of displaced physeal injuries of the proximal humerus. We also aim to alert the orthopedic community to the potential hazards of overtreatment in such cases. The parents consented to the publication of data concerning this case.
Case Report
A girl was delivered after full-term twin gestation to a multiparous mother. Her twin sister was delivered vaginally at home by a nurse. Unsuccessful attempts of vaginal breech delivery of that girl necessitated transfer of the mother to a hospital. The obstetrician carried out repeated unfruitful attempts of vaginal delivery at the hospital. Eventually, the girl was delivered by a cesarean section. The girl was incubated for 10 days due to neonatal jaundice and convulsions that resolved with no residual manifestations. The parents also gave a history of ecchymosis and loss of active movements of the left arm. The parents reported that the newborn was diagnosed as having a left obstetric palsy and were asked to initially immobilize the arm with a simple sling. No history suggestive of infection was encountered. The patient presented to us 5-week postnatal.
Passive motion of the left upper limb was painful. The arm lay limp by the side. Palpation revealed a bony irregularity of the proximal humerus. No signs suggestive of neonatal brachial plexus injury were encountered. The elbow, forearm, wrist, fingers, and hand movement and position showed no abnormality. No deformity of the hand or posture abnormalities was noticed. Spontaneous movements and neonatal reflexes were intact. No ptosis or meiosis indicative of severe neonatal brachial plexus palsy was present. The patient was afebrile. Local signs of infection were absent and laboratory parameters were not suggestive of infection. No additional birth injuries were present.
Radiographs of the left shoulder of the newborn obtained 1-week postnatal revealed the absence of ossification of the proximal humeral epiphysis. The metaphysis appeared completely caudal in relation to the scapular articulation. Thus, a physeal separation was diagnosed retrospectively [Figure - 1]a and [Figure - 1]b. No attempt of closed or open reduction was performed. A simple sling was applied to be used on demand. The patient gradually regained full and painless active and passive movements of the left shoulder within 16-week postnatal.
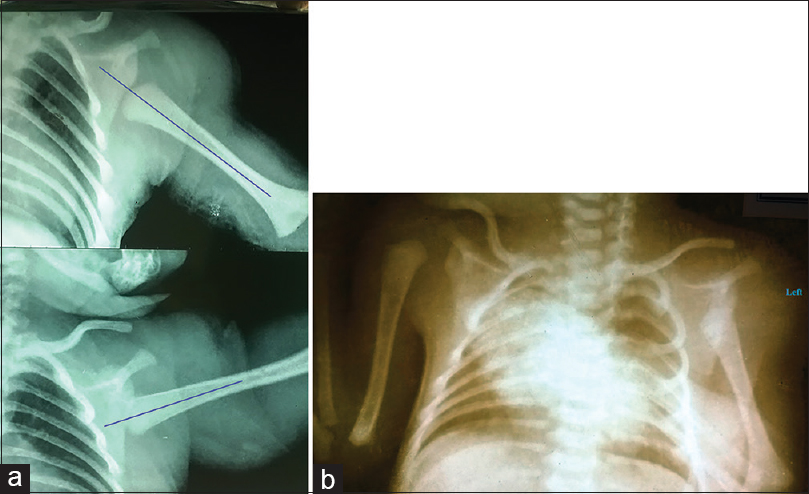 |
| Figure 1: (a and b) Radiographs of the left shoulder. (a) And both shoulders. (b) One-week postnatal demonstrating proximal humeral physeal separation. Note the long axis of the metaphysis is projected completely caudad (distal) in relation to the glenoid articulation. This is demonstrated in both views |
Radiographic examination of the left shoulder 5-week postnatal demonstrated significant subperiosteal new bone formation and subsequent progressive remodeling [Figure - 2]a, [Figure - 2]b, [Figure - 2]c. At 1-year follow-up, radiographs showed an anatomic relationship between the epiphyses and metaphysis, and the growth plate was open. In addition, the radiographs demonstrated a normal relationship of the ossification center with the glenoid and normally growing well-formed epiphyses with no evidence of avascular necrosis or deformation [Figure - 3]a and [Figure - 3]b. Moreover, the patient demonstrated a pain-free range of motion of the left shoulder and whole upper extremity. At 4-year postinjury, we contacted the child's parents by telephone to enquire about the outcome. The parents did not report any functional limitations of the injured upper extremity. Nor did they report any noticeable shortening. The parents were satisfied with treatment offered to their child. The patient was unavailable for a radiographic assessment at that point in time.
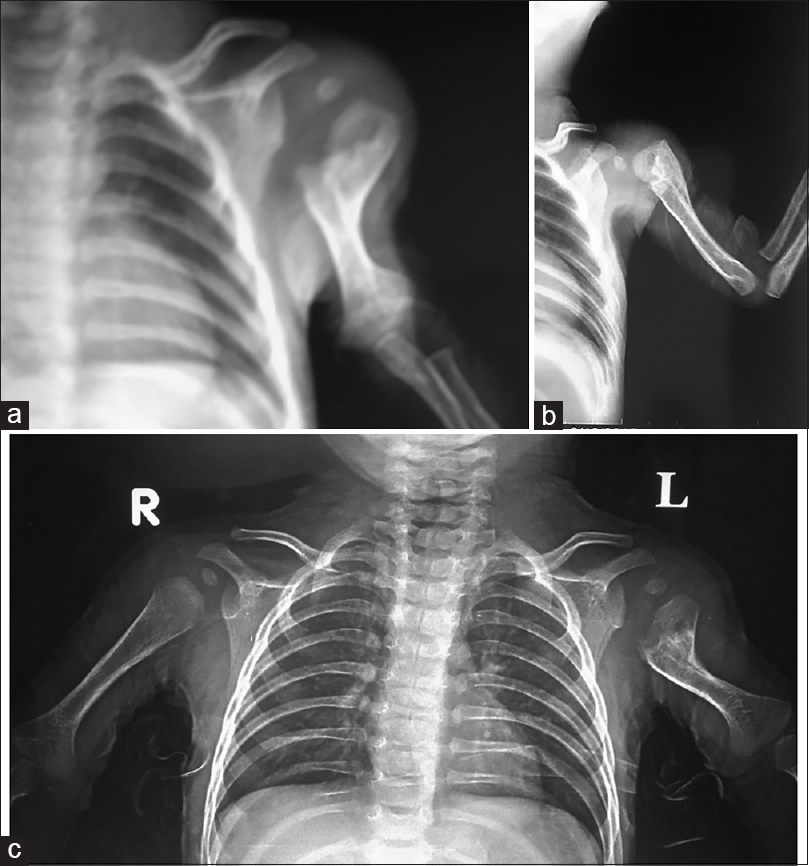 |
| Figure 2: (a-c) The remodeling process of left proximal humeral physeal separation. Note the extensive subperiosteal new bone formation at 5-week postnatal and ossification of the proximal humeral epiphysis (a), progressive remodeling of the metaphysis at 11-week postnatal (b), and at 17-week postnatal (c) |
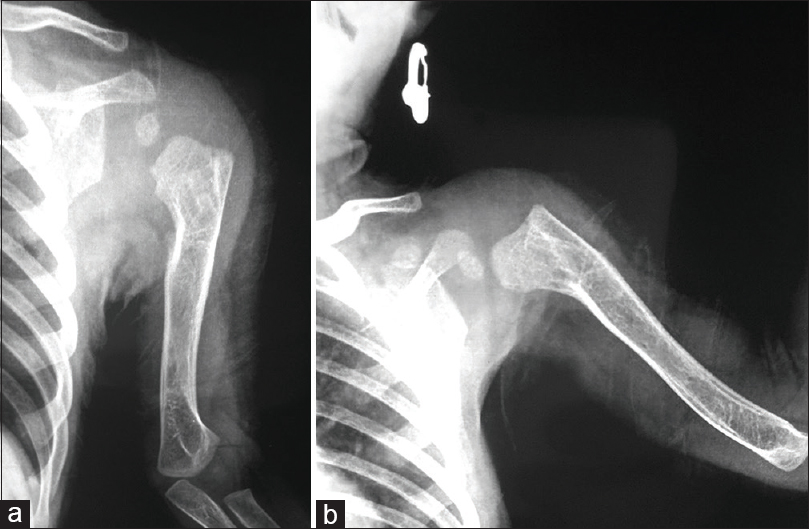 |
| Figure 3: (a and b) One-year follow-up of the left proximal humeral physeal separation. Note complete remodeling and restoration of humerus length and absence of signs of avascular necrosis of proximal humeral epiphysis in anteroposterior (a) and lateral views (b) |
Discussion
Isolated PHPS corresponding to Salter and Harris type I injury is rare and occurs typically in newborns and toddlers.[3],[7] Although the growth plate is interrupted at the level of the degenerative layer of cells, these lesions remain with low risk of growth disturbance.[5] The proximal humeral epiphysis is responsible for 80% of the humeral growth in length. As a consequence, its remodeling potential is considerable and is related to the age of the patient: the older the child, the lower the potential.[8],[9],[10],[11]
Because of the high potential of spontaneous correction due to the proximal humeral epiphysis, the prognosis of PHPS is good, especially in neonates.[5],[8],[9],[10],[11] On the other hand, displaced and late presenting epiphyseal fractures around the distal humerus are generally more likely to have a significant residual deformity than is a displaced and late presenting fracture separations of the proximal humeral epiphysis.[12],[13],[14] Therefore, we paid little attention to realignment or reduction, especially in the event of the delayed presentation we faced. Our patient attained an excellent clinical outcome and demonstrated an enormous remodeling potential on radiographs. The timing and sequence of eruption of secondary ossification centers around the skeleton follows a fairly predictable pattern and correlates with race.[15],[16],[17] This can serve as a guide for the appropriate reading of children's radiographs in acute skeletal trauma. Typically, the secondary ossification centers of the proximal humerus of the newborn remain unossified until 4 months of age.[15] This conforms to the findings reported in our newborn. Furthermore, this served as an important differentiating point between a physeal separation and a glenohumeral joint dislocation, an extremely rare occurrence in newborns.
El-Adl et al.[7] reported eight cases of PHPS in newborns, which failed closed reduction; subsequent open reduction was performed using Kirschner wires, with subsequent excellent healing and no avascular necrosis of the epiphysis or limb length deformity. Yet, their management plan that they employed leaves many questions unanswered. They did not provide any justification for routinely resorting to open reduction and internal fixation. EL-Adl et al.[7] reported that they built their decision on the necessity of surgical intervention on the operative findings of the long head of the biceps that was entrapped in the site of slipping in all cases. These operative findings still do not clarify the “preoperative” criteria, on which their operative decision was based on. These authors also reported that they have never seen a child that had a neglected physeal separation to know the exact outcome of nonsurgical treatment.[7] In contrast, a large study reporting long-term results of PHPS in 72 patients[5] and a matched cohort study comparing operative versus non-operative treatment of displaced PHPS[4] have argued the conservative treatment in PHPS, and have augmented the existing literature reports of favorable clinical outcomes with nonsurgical treatment for such injuries. In the current case study, our patient was managed conservatively, as the literature support excellent outcome with conservative treatment, and satisfactory clinical and radiologic results were achieved. We believe that the remodeling potential of the proximal humerus in neonates allows a conservative treatment and that closed reduction or open reduction and internal fixation are not routinely justified.
Generally speaking, PHPSs are rarely accompanied by injury of the brachial plexus.[4],[5] The clinical findings of the current case are in line with the previous authors. The authors of the current study remain concerned about the potential hazards of closed reduction performed by others[7] with respect to brachial plexus injury. Furthermore, concerns remain about the thick Kirschner wires penetrating the largely unossified epiphysis of the proximal humerus used by the previous authors.
Conclusion
The clinical and radiographic outcome of the current case study and literature update reveal that an excellent outcome could be achieved with conservative management in cases of PHPS in neonates. We believe that the necessity to achieve an absolute anatomic fracture reduction in all planes by closed or open procedures is not always necessary in neonates. The outcome of this study together with the existing literature demonstrates that closed reduction and routine open reduction and internal fixation for PHPS is unjustified and may be considered as a form of overtreatment.
Declaration of the patient
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient's guardian has given consent for the child's images and other clinical information to be reported in the journal. The patient's guardian understands that the name and initials of the child will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
JFHA conceived and designed the study, conducted research, provided research materials, and collected and organized data. JFHA and KNY analyzed and interpreted data. KNY wrote initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Rose SH, Melton LJ 3rd, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop Relat Res 1982;168:24-30. [Google Scholar] |
| 2. | Mallick A, Prem H. Physeal injuries in children. Surg Oxf Int Ed 2017;35:10-7. [Google Scholar] |
| 3. | Salter RB, Harris R. Injuries involving the epiphyseal plate. J Bone Joint Surg Am 1963;45:587-622. [Google Scholar] |
| 4. | Chaus GW, Carry PM, Pishkenari AK, Hadley-Miller N. Operative versus nonoperative treatment of displaced proximal humeral physeal fractures: A matched cohort. J Pediatr Orthop 2015;35:234-9. [Google Scholar] |
| 5. | Binder H, Schurz M, Aldrian S, Fialka C, Vécsei V. Physeal injuries of the proximal humerus: Long-term results in seventy two patients. Int Orthop 2011;35:1497-502. [Google Scholar] |
| 6. | Broker FH, Burbach T. Ultrasonic diagnosis of separation of the proximal humeral epiphysis in the newborn. J Bone Joint Surg Am 1990;72:187-91. [Google Scholar] |
| 7. | El-Adl WA, Elgohary HS, Elshennawy MM. Epiphyseal separation of the proximal humerus after birth trauma. Eur J Orthop Surg Traumatol 2014;24:863-7. [Google Scholar] |
| 8. | Baxter MP, Wiley JJ. Fractures of the proximal humeral epiphysis. Their influence on humeral growth. J Bone Joint Surg Br 1986;68:570-3. [Google Scholar] |
| 9. | Gladstein AZ, Schade AT, Howard AW, Camp MW. Reducing resource utilization during non-operative treatment of pediatric proximal humerus fractures. Orthop Traumatol Surg Res 2017;103:115-8. [Google Scholar] |
| 10. | King EC, Ihnow SB. Which proximal humerus fractures should be pinned? Treatment in skeletally immature patients. J Pediatr Orthop 2016;36 Suppl 1:S44-8. [Google Scholar] |
| 11. | Guo JB, Zhang JD, Zhao YM, Yang Y. Fracture separation of the proximal humeral epiphyses in neonate: A case report and literature review. Chin J Traumatol 2010;13:62-4. [Google Scholar] |
| 12. | El-Sobky TA, Haleem JF, Sakr HM, Aly AS. A neglected markedly displaced medial epicondyle fracture with simultaneous ulnar nerve palsy in an adolescent. Clin Orthop Surg 2017;9:542-6. [Google Scholar] |
| 13. | Bakarman KA, Alsiddiky AM, Alzain KO, Alkhawashki HM, Bin Nasser AS, Alsaleh KA, et al. Humeral lateral condyle fractures in children: Redefining the criteria for displacement. J Pediatr Orthop B 2016;25:429-33. [Google Scholar] |
| 14. | EL-Sobky TA, Samir S, Aly AS. Neglected anterior monteggia lesion with a displaced intra-articular medial condyle fracture in a child: A rare and challenging association. J Musculoskelet Surg Res 2017;1:49-52. [Google Scholar] |
| 15. | Zember JS, Rosenberg ZS, Kwong S, Kothary SP, Bedoya MA. Normal skeletal maturation and imaging pitfalls in the pediatric shoulder. Radiographics 2015;35:1108-22. [Google Scholar] |
| 16. | Miyazaki CS, Maranho DA, Agnollitto PM, Nogueira-Barbosa MH. Study of secondary ossification centers of the elbow in the Brazilian population. Acta Ortop Bras 2017;25:279-82. [Google Scholar] |
| 17. | Elhusseiny K, El-Sobky TA. Imaging pitfalls of the acutely traumatized pediatric elbow. Oman Med J 2018;33:444-6. [Google Scholar] |
Fulltext Views
5,010
PDF downloads
2,057





