Translate this page into:
A review article of medial tibial stress syndrome
Corresponding Author:
Abdulaziz Z Alomar
Department of Orthopaedic, King Saud University Medical City, College of Medicine, King Saud University, Riyadh
Saudi Arabia
dr_abdulaziz@yahoo.com
| How to cite this article: Alfayez SM, Ahmed ML, Alomar AZ. A review article of medial tibial stress syndrome. J Musculoskelet Surg Res 2017;1:2-5 |
Abstract
Medial tibial stress syndrome (MTSS), which also known as “shin splints,” is leg pain due to repetitive stresses. It is common among athletes, especially runners. It is estimated that up to 35% of all athletes have MTSS. As a consequence, the athletes spend less time in training and some of them refrain from exercises because of the exercise-induced pain, which adversely affects their career. The exact cause is still unclear. Some studies in the literature have suggested that the underlying mechanism is microdamage due to repetitive stresses. Risk factors include female gender, increased range of hip external rotation in males, navicular bone drop, increased body mass index, and training intensity. Patients usually complain of bilateral pain mainly in the anterior and/or medial side of their distal leg. Pain is aggravated by activity and relieved by rest. The examination may reveal swelling and tenderness, especially in the tibial posteromedial aspect along with other suggestive signs. Imaging modalities including radiographs, computed tomography, magnetic resonance imaging, and bone scintigraphy can be utilized to rule out other causes of similar presentation. Prevention is by repetitive stress avoidance, shock absorbing insoles, appropriate treatment of other stress-induced injuries, and screening for anatomical abnormalities. It is mostly treated conservatively with rest, ice and pain control. Athletes can keep training by doing different exercises that do not cause recurrent stresses. Surgery, which is rarely performed, is a treatment option in recalcitrant cases.Introduction
Medial tibial stress syndrome (MTSS) is characterized by pain or discomfort of the leg secondary to repetitive stresses.[1] It affects approximately 35% of athletes and is considered one of the most prevalent overuse-induced pain in this population.[2] Furthermore, up to 70% of runners may develop an overuse injury including MTSS over a 1-year period.[3] MTSS has been noticed in running along with other sports such as American football and basketball.[4] In soccer, overuse injuries including shin splints represent 18.5% of hindering injuries.[5] Although MTSS is one of the most common causes of exercise-related leg pain among different populations, its exact cause is still unclear.[2],[6] MTSS requires early detection and management. Otherwise, limitations due to repetitive stresses will ensue.[7]
This review article aims to evaluate, discuss, and summarize findings in the literature about MTSS.
Pathogenesis and Risk Factors
The exact cause and pathophysiology behind MTSS are still unclear; however, multiple risk factors have been discussed thoroughly in the literature.[8],[9],[10],[11]
A mechanism of developing MTSS can be possibly explained by repetitive stress inducing microdamage higher than the repair threshold. This type of stress on a bone is unlike the optimal stress with adequate rest where the bone strengthens instead. It is also thought that MTSS can occur when individuals have increased bending forces on the tibia exceeding the opposing strength of leg muscles.[12],[13] MTSS has been linked to periostitis or repeated tibial bending and bowing.[9],[14],[15] Multiple contributory factors to the periostitis are related to the training intensity and training surfaces.[6] Moreover, training errors such as a sudden increase in training volume, along with aging footwear, is one of the more common causes of MTSS, especially on the hard surfaces.[13],[16] A relation between MTSS and the crural fascia of the deep posterior compartment has been suggested in the literature. Muscles that are thought to be involved are soleus and tibialis posterior as both can cause periosteal traction. It has also been suggested that the contractions of flexor digitorum longus increase the strain on the tibial fascia.[17],[18] Beck and Osternig concluded in their study that MTSS can be induced by muscle traction of the periosteum with the soleus being the major one.[17] Magnetic resonance imaging (MRI) showed abnormalities over the soleus origin, which proposes its association with MTSS.[19] Hence, MTSS is also known as soleus syndrome.[20] Based on the findings of several studies, MTSS is not a compartment syndrome since measured compartment pressures were normal although other authors reported variation in compartment pressures among MTSS patients.[2],[15],[21]
According to a systemic review and meta-analysis conducted in 2013, females are more prone to develop MTSS.[11] In this regard, a study involving naval recruits revealed that 53% of females and only 28% of males had MTSS.[22] Other proven risk factors are a previous history of MTSS, history of orthotics use, and increased hip external rotation range of motion in males. Modifiable-risk factors include increased body mass index, which is significantly associated with MTSS among high school runners as well as intense training. Increased navicular drop, which can be detected clinically, is also a risk factor for MTSS.[11],[22],[23] Furthermore, increased plantar flexion of the ankle joint is associated with MTSS.[24] Overpronation, causing flatting of the foot and the lower leg to rotate inward, is also a possible risk factor, but it has not been shown to be important during the stance phase.[6],[10] Oversupination, which causes the foot to roll outward too much during foot contact with the ground, increases stress in the distal tibia. Sobhani et al. studied the anthropometric variants including the navicular drop, lateral tibial length, and iliospinal and trochanteric heights along with a hip range of motion discrepancies in an internal and external rotation. The aforementioned variants were all significantly different among people with MTSS compared to healthy individuals.[25] After using fluoroscopic imaging while running, a recent paper showed that deformities of the medial and lateral longitudinal arches associated with significantly higher angular changes were all linked to MTSS. After the heel strike, they also observed a significant anterior displacement of the medial and lateral longitudinal arches. Moreover, there was an inferior displacement in both arches at certain timings following the heel strike in the MTSS group.[26] Patients with MTSS had a higher subtalar range of motion following the analysis of one forward step, unlike the talocrural joint, which had no significant difference in the range of motion between individuals with or without MTSS.[27]
Clinical Presentation
Patients with MTSS commonly present with bilateral pain or aches along the medial side of the tibia usually distally.[6] The middle portion of the medial tibia is a common site for pain as well. However, shin splints may involve any part of the leg. Pain is usually described as dull and often more aching if felt on the lateral side. Pain is aggravated by activity and relieved by rest; it is frequently felt at the beginning of an exercise and then decreases in intensity with further activity. Pain is often worse the next morning but may ease off over time. In severe and prolonged MTSS, pain can be felt even at rest. Radiations to the foot and dysesthesia have been reported. These presenting symptoms are similar in other overuse injuries such as stress fractures. Thus, a high index of suspicion is required.[1],[6],[13]
In the examination, it is emphasized that the physician starts with inspection looking for suggestive signs such as worn out shoes or abnormalities such as limb length discrepancy.[4] Although there are multiple signs of MTSS such as pain on hopping and pain on percussion, diffuse tenderness over the posteromedial border of the tibia has been shown to be the most sensitive sign [Figure - 1]. MTSS patient can also present with mild swelling characterized by subcutaneous thickening of the tibial border. This should be differentiated from palpable callus. The examination may reveal weakness and pain on passive stretching.[1],[2] It is important clinically to exclude stress fracture, which has more localized pain, tenderness, and edematous changes. Moreover, conditions such as chronic exertional compartment syndrome, tendinitis, vasculitis, nerve impingement, and popliteal artery entrapment should also be considered when assessing patients with MTSS.[13],[28],[29]
 |
| Figure 1: How to palpate the posteromedial aspect of the tibia to elicit tenderness in medial tibial stress syndrome |
Investigation
The importance of imaging modalities in the presence of accurate and suggestive history and physical examination has been questioned. However, they are often necessary to rule out other possible causes such as a stress fracture and chronic exertional compartment syndrome. The imaging modalities include radiographs, computed tomography (CT), MRI, and bone scintigraphy. Radiography is mainly used to rule out stress fracture even though the fracture may not be evident until 2 weeks when callus starts to form. It may also show posteromedial periosteal reaction, but it is not as clear as the reaction seen in other imaging modalities.[30],[31],[32] According to Gaeta et al., all long-distance runners had CT scan abnormalities. The CT scan findings are classified into three types. Type 0 was normal. Type 1 shows distributed and slightly reduced cortical attenuation without osteopenia. Type 2 shows osteopenia with or without cavitations or striations. The majority of asymptomatic runners had Type 0 CT scan findings. On the other hand, all symptomatic tibiae were of Type 2 with MTSS as the main cause.[31] Bone scintigraphy can confirm MTSS with a sensitivity rate of 74%–84% [Figure - 2]. The lesion in the affected site is most likely due to osteoblast activation by periosteal irritation. A way to distinguish between stress fracture and MTSS is the diffuse uptake that is most evident in the third phase in triple-phase bone scintigraphy, unlike stress fracture, which is more localized and tends to be positive in all phases. A disadvantage of bone scintigraphy is the high false-positive rate demonstrated by the presence of pathological changes in 80% of asymptomatic athletes.[13],[29] MRI is the most sensitive imaging modality in MTSS with a sensitivity rate of 88%.[30] Unilateral bone marrow edema was the most prominent MRI finding seen in 64% followed by periosteal edema (35%).[19],[33] Individuals with clinical MTSS can also have a normal MRI scan. A disadvantage of MRI in MTSS is the positive association between chronicity and normal scans.[19],[33] Biopsy findings in MTSS are characterized often by fibrous thickening and rarely infiltration by chronic inflammatory cells. However, histology in MTSS is inconclusive. Bhatt et al. reported that there was no correlation regarding periosteal reaction between the findings of bone scans and periosteal histological specimens in patients who underwent surgery.[34]
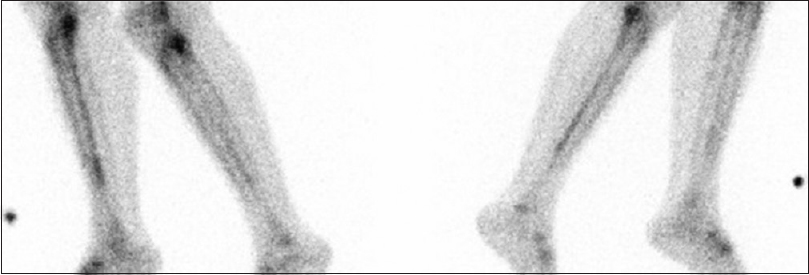 |
| Figure 2: A delayed phase of bone scintigraphy showing linear uptake along the posteromedial cortex of the left and right tibiae |
Prevention
Overstress avoidance has been described as a measure that can be used to prevent MTSS. This is of great importance since repetitive injuries usually accumulate before the appearance of symptoms.[35] It has been claimed that 50% of running-related injuries are secondary to training errors. Prevention can be accomplished by awareness and education about running-induced injuries, warm-up and stretching exercises, suitable footwear, and gradual exercise programs; however, the benefits of all these measures are controversy and carry limited evidence.[36],[37] Shoe modifications, such as shock absorbing insoles, help to prevent MTSS. Pronation-controlled insoles are also beneficial, especially to people with a navicular drop.
Treatment
The main goals of MTSS treatment are pain relieve and return to a pain-free activity. In the acute stage, rest along with ice application is shown to be the most effective treatment method.[38] Acetaminophen and nonsteroidal anti-inflammatory drugs can be used for analgesia. The evidence on injecting corticosteroids, platelet-rich plasma, or prolotherapy for MTSS is very limited.[4] Thus, it is believed that they should not be routinely administered.
Physical therapy, through heel cord stretching and calf muscle strengthening exercises, has been implemented for patients with MTSS.[39],[40] Furthermore, the extracorporeal shockwave therapy can be beneficial.[41],[42] It is not advised to use pneumatic leg braces as it has been shown that they are ineffective.[43]
Once pain has been relieved, the treatment should focus mainly on training modification. This can be achieved by 50% reduction in training frequency and intensity as well as the running distance.[4],[14]
Surgical options consist of posterior fasciotomy with or without cauterization of the posteromedial ridge of the tibia.[44],[45] According to Yates et al., surgery reduced pain in athletes by 72% on the visual pain analog scale.[44] A case series involving 34 MTSS patients showed an overall effectiveness of fasciotomy of the posterior compartment where 78% of the patients had either good or excellent outcome.[45] As the majority recover with conservative treatment, surgery is reserved for recalcitrant cases.[40]
Summary
MTSS is characterized by pain or discomfort of the leg secondary to repetitive stresses. The exact cause and pathophysiology behind MTSS are still unclear. Patients usually complain of pain in the lower half of the medial tibia. Diffuse tenderness over the posteromedial border of the tibia has been shown to be the most sensitive sign. Various imaging modalities can be utilized to either confirm the diagnosis of MTSS or rule out other causes of similar presentation. Overstress avoidance is the main preventive measure of MTSS. The main goals of MTSS treatment are pain relieve and return to pain-free activities. In the acute stage, rest along with ice application is shown to be the most effective method. As the majority recovers with conservative treatment, surgery is reserved for recalcitrant cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors contributions
SMA Drafting and submitting the manuscript, MLA Reviewing and editing the manuscript, AZA Designing, reviewing and editing the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Bates P. Shin splints – A literature review. Br J Sports Med 1985;19:132-7. [Google Scholar] |
| 2. | Moen MH, Tol JL, Weir A, Steunebrink M, De Winter TC. Medial tibial stress syndrome: A critical review. Sports Med 2009;39:523-46. [Google Scholar] |
| 3. | Hreljac A, Marshall RN, Hume PA. Evaluation of lower extremity overuse injury potential in runners. Med Sci Sports Exerc 2000;32:1635-41. [Google Scholar] |
| 4. | Galbraith RM, Lavallee ME. Medial tibial stress syndrome: Conservative treatment options. Curr Rev Musculoskelet Med 2009;2:127-33. [Google Scholar] |
| 5. | Chomiak J, Junge A, Peterson L, Dvorak J. Severe injuries in football players. influencing factors. Am J Sports Med 2000;28:S58-68. [Google Scholar] |
| 6. | Spiker AM, Dixit S, Cosgarea AJ. Triathlon: Running injuries. Sports Med Arthrosc 2012;20:206-13. [Google Scholar] |
| 7. | Franklyn M, Oakes B, Field B, Wells P, Morgan D. Section modulus is the optimum geometric predictor for stress fractures and medial tibial stress syndrome in both male and female athletes. Am J Sports Med 2008;36:1179-89. [Google Scholar] |
| 8. | Hamstra-Wright KL, Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: A systematic review and meta-analysis. Br J Sports Med 2015;49:362-9. [Google Scholar] |
| 9. | Franklyn M, Oakes B. Aetiology and mechanisms of injury in medial tibial stress syndrome: Current and future developments. World J Orthop 2015;6:577-89. [Google Scholar] |
| 10. | Winters M, Veldt H, Bakker EW, Moen MH. Intrinsic factors associated with medial tibial stress syndrome in athletes: A large case-control study. S Afr J Sports Med 2013;25:63-7. [Google Scholar] |
| 11. | Newman P, Witchalls J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: A systematic review and meta-analysis. Open Access J Sports Med 2013;4:229-41. [Google Scholar] |
| 12. | Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc 2004;36:845-9. [Google Scholar] |
| 13. | Reshef N, Guelich DR. Medial tibial stress syndrome. Clin Sports Med 2012;31:273-90. [Google Scholar] |
| 14. | Beck BR. Tibial stress injuries. An aetiological review for the purposes of guiding management. Sports Med 1998;26:265-79. [Google Scholar] |
| 15. | Mubarak SJ, Gould RN, Lee YF, Schmidt DA, Hargens AR. The medial tibial stress syndrome. A cause of shin splints. Am J Sports Med 1982;10:201-5. [Google Scholar] |
| 16. | Carr K, Sevetson E, Aukerman D. Clinical inquiries. how can you help athletes prevent and treat shin splints? J Fam Pract 2008;57:406-8. [Google Scholar] |
| 17. | Beck BR, Osternig LR. Medial tibial stress syndrome. The location of muscles in the leg in relation to symptoms. J Bone Joint Surg Am 1994;76:1057-61. [Google Scholar] |
| 18. | Saxena A, O'Brien T, Bunce D. Anatomic dissection of the tibialis posterior muscle and its correlation to medial tibial stress syndrome. J Foot Surg 1990;29:105-8. [Google Scholar] |
| 19. | Anderson MW, Ugalde V, Batt M, Gacayan J. Shin splints: MR appearance in a preliminary study. Radiology 1997;204:177-80. [Google Scholar] |
| 20. | Michael RH, Holder LE. The soleus syndrome. A cause of medial tibial stress (shin splints). Am J Sports Med 1985;13:87-94. [Google Scholar] |
| 21. | Detmer DE. Chronic shin splints. Classification and management of medial tibial stress syndrome. Sports Med 1986;3:436-46. [Google Scholar] |
| 22. | Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med 2004;32:772-80. [Google Scholar] |
| 23. | Yagi S, Muneta T, Sekiya I. Incidence and risk factors for medial tibial stress syndrome and tibial stress fracture in high school runners. Knee Surg Sports Traumatol Arthrosc 2013;21:556-63. [Google Scholar] |
| 24. | Moen MH, Bongers T, Bakker EW, Zimmermann WO, Weir A, Tol JL, et al. Risk factors and prognostic indicators for medial tibial stress syndrome. Scand J Med Sci Sports 2012;22:34-9. [Google Scholar] |
| 25. | Sobhani V, Shakibaee A, Khatibi Aghda A, Emami Meybodi MK, Delavari A, Jahandideh D, et al. Studying the relation between medial tibial stress syndrome and anatomic and anthropometric characteristics of military male personnel. Asian J Sports Med 2015;6:e23811. [Google Scholar] |
| 26. | Noh B, Masunari A, Akiyama K, Fukano M, Fukubayashi T, Miyakawa S, et al. Structural deformation of longitudinal arches during running in soccer players with medial tibial stress syndrome. Eur J Sport Sci 2015;15:173-81. [Google Scholar] |
| 27. | Akiyama K, Noh B, Fukano M, Miyakawa S, Hirose N, Fukubayashi T, et al. Analysis of the talocrural and subtalar joint motions in patients with medial tibial stress syndrome. J Foot Ankle Res 2015;8:25. [Google Scholar] |
| 28. | Clanton TO, Solcher BW. Chronic leg pain in the athlete. Clin Sports Med 1994;13:743-59. [Google Scholar] |
| 29. | Patel DS, Roth M, Kapil N. Stress fractures: Diagnosis, treatment, and prevention. Am Fam Physician 2011;83:39-46. [Google Scholar] |
| 30. | Gaeta M, Minutoli F, Scribano E, Ascenti G, Vinci S, Bruschetta D, et al. CT and MR imaging findings in athletes with early tibial stress injuries: Comparison with bone scintigraphy findings and emphasis on cortical abnormalities. Radiology 2005;235:553-61. [Google Scholar] |
| 31. | Gaeta M, Minutoli F, Vinci S, Salamone I, D'Andrea L, Bitto L, et al. High-resolution CT grading of tibial stress reactions in distance runners. AJR Am J Roentgenol 2006;187:789-93. [Google Scholar] |
| 32. | Swischuk LE, Jadhav SP. Tibial stress phenomena and fractures: Imaging evaluation. Emerg Radiol 2014;21:173-7. [Google Scholar] |
| 33. | Moen MH, Schmikli SL, Weir A, Steeneken V, Stapper G, de Slegte R, et al. A prospective study on MRI findings and prognostic factors in athletes with MTSS. Scand J Med Sci Sports 2014;24:204-10. [Google Scholar] |
| 34. | Bhatt R, Lauder I, Finlay DB, Allen MJ, Belton IP. Correlation of bone scintigraphy and histological findings in medial tibial syndrome. Br J Sports Med 2000;34:49-53. [Google Scholar] |
| 35. | Wilder RP, Sethi S. Overuse injuries: Tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med 2004;23:55-81, vi. [Google Scholar] |
| 36. | James SL, Bates BT, Osternig LR. Injuries to runners. Am J Sports Med 1978;6:40-50. [Google Scholar] |
| 37. | Clement DB, Taunton JE. A guide to the prevention of running injuries. Can Fam Physician 1980;26:543-8. [Google Scholar] |
| 38. | Johnston E, Flynn T, Bean M, Breton M, Scherer M, Dreitzler G, et al. A randomized controlled trial of a leg orthosis versus traditional treatment for soldiers with shin splints: A pilot study. Mil Med 2006;171:40-4. [Google Scholar] |
| 39. | Andrish JT, Bergfeld JA, Walheim J. A prospective study on the management of shin splints. J Bone Joint Surg Am 1974;56:1697-700. [Google Scholar] |
| 40. | Brewer RB, Gregory AJ. Chronic lower leg pain in athletes: A guide for the differential diagnosis, evaluation, and treatment. Sports Health 2012;4:121-7. [Google Scholar] |
| 41. | Moen MH, Rayer S, Schipper M, Schmikli S, Weir A, Tol JL, et al. Shockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled study. Br J Sports Med 2012;46:253-7. [Google Scholar] |
| 42. | Rompe JD, Cacchio A, Furia JP, Maffulli N. Low-energy extracorporeal shock wave therapy as a treatment for medial tibial stress syndrome. Am J Sports Med 2010;38:125-32. [Google Scholar] |
| 43. | Moen MH, Bongers T, Bakker EW, Weir A, Zimmermann WO, van der Werve M, et al. The additional value of a pneumatic leg brace in the treatment of recruits with medial tibial stress syndrome; a randomized study. J R Army Med Corps 2010;156:236-40. [Google Scholar] |
| 44. | Yates B, Allen MJ, Barnes MR. Outcome of surgical treatment of medial tibial stress syndrome. J Bone Joint Surg Am 2003;85-A: 1974-80. [Google Scholar] |
| 45. | Järvinnen M, Aho H, Niittymäki S. Results of the surgical treatment of the medial tibial syndrome in athletes. Int J Sports Med 1989;10:55-7. [Google Scholar] |
Fulltext Views
12,746
PDF downloads
2,157





