Translate this page into:
Advancing care for congenital pseudoarthrosis: A case series highlighting the combined use of an intramedullary device with either Ilizarov’s fixators or plating for the treatment of congenital pseudoarthrosis
*Corresponding author: Yazeed A. Alsehibani, MBBS., Department of Orthopedics, College of Medicine, King Saud University, Riyadh, Saudi Arabia. yazeed.a.s2011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Alhuzaimi FS, Alsubaie AA, Alshayhan FA, Alsehibani YA, Alrawaf RK. Advancing care for congenital pseudoarthrosis: A case series highlighting the combined use of intramedullary device with either Ilizarov’s fixators or plating for the treatment of congenital pseudoarthrosis. J Musculoskelet Surg Res. 2025;9:121-7. doi: 10.25259/JMSR_336_2024
Abstract
Congenital pseudarthrosis of the tibia (CPT) is a bone defect in which non-union occurs in a dysplastic segment of the tibial diaphysis following a fracture at the same site. Once a fracture occurs through a susceptible bone and pseudoarthrosis is formed, spontaneous healing is unexpected. Therefore, surgical intervention is essential for healing. This study aimed to compare the outcomes of using intramedullary nailing with either Ilizarove’s fixator or plating as a treatment method for CPT to other treatment methods described in the literature. This case series study included nine patients who presented to the Pediatric Orthopedic clinic with CPT from 2018 to 2021. All patients were previously diagnosed with Neurofibromatosis-1 by pediatric genetics and presented with unilateral CPT. The minimum follow-up duration was 12 months. Nine patients were diagnosed with neurofibromatosis. Of the nine patients, fixation was supplemented with an Ilizarov external fixator in 5 patients, and the plate was used in 4 patients. Most patients (88.9%) achieved union, except for one patient with an infection requiring multiple surgical debridement. The type of fixation was not significantly associated with the union rate. In conclusion, patients who underwent intramedullary nailing in conjugation with Ilizarov’s fixator or plating for the treatment of CPT and cross-union have achieved excellent union rates with no refracture in early outcomes.
Keywords
Congenital pseudarthrosis
Ilizarov
Neurofibromatosis
Tibia
Union
INTRODUCTION
Congenital pseudarthrosis of the tibia (CPT) is a bone defect in which non-union occurs in a dysplastic segment of the tibial diaphysis following a fracture at the same site. In most cases, CPT has been linked to neurofibromatosis type 1 (NF-1); however, no signs of neurofibromatosis tissue at the site of CPT have been found.[1] CPT is a rare condition with an incidence of 1:53,000 in Norway[2] ranging from 1:28,544 to 1:190,000 live births, according to two other studies conducted in Finland and Denmark, respectively.[3,4] CPT is usually preceded by bowing, where the risk of fracture and consequent pseudoarthrosis is higher with progressive bowing.[5]
Non-operative management should be started immediately once tibial bowing is observed in patients with a higher chance of CPT development using ankle-foot orthosis (AFO) and knee-AFO is recommended as non-operative measures depending on the patient’s age to extend the pre-operative period and minimize complications.[6]
Once a fracture occurs through a susceptible bone and pseudoarthrosis is formed, spontaneous healing is unexpected. Therefore, surgical intervention is essential for healing.[6] Healing potential through pseudoarthrosis of the tibia is challenging. Hence, multiple surgical options with different healing rates have been described in the literature.[7] For the last few decades, there has been much discussion on which surgical treatment is optimal to achieve bone union.[7]
This study aimed to compare the outcomes of using intramedullary nailing with either Ilizarove’s fixator or plating as a treatment method for CPT to other treatment methods described in the literature.
CASE SERIES
This study was approved by the Institutional Review Board (IRB). This case series study included nine patients who presented to the Pediatric Orthopedic clinic with CPT from 2018 to 2021. All patients were previously diagnosed with NF-1 by pediatric genetics and presented with unilateral CPT. The minimum follow-up duration was 12 months.
The inclusion criteria
All patients with CPT underwent resection of pseudoarthrosis and intramedullary tibia nailing supplemented with Ilizarov’s fixator or plating. In addition, iliac bone autografting was used over the site of pseudoarthrosis resection.
Surgical technique
Before surgery, all patients had sufficient pre-operative imaging to locate the pseudoarthrosis site and quantify the resection margins. All patients received pamidronate injections 3 months preoperatively. A tourniquet was applied over the thigh and inflated before the skin incision. Starting with an anteromedial leg skin incision centered over the pseudoarthrosis segment. Dissection of fat till periosteum was reached. Medial and lateral flaps were created. The periosteum was incised and the hamartoma was resected completely. The bone was exposed and the planned resection part was marked. Resection was performed with the evaluation of the healthy part, and resection was done if no bleeding was seen.
The next step was a lateral skin incision over the fibula to perform osteotomy of the fibula just proximal to the pseudoarthrosis segment. Then, a drill was used to open the tibial canal for the proximal segment in a retrograde fashion and an antegrade fashion for the distal segment under fluoroscopy, aiming to drill in the center of the canal. A knee skin incision was made using a medial parapatellar approach and through the middle of the prepatellar fascia, exposing the pre-spinal area at the proximal tibia. A pre-bent 2.0 mm K-wire was inserted and confirmed under fluoroscopy, after which reduction of the proximal end was performed. Reduction of the distal segment was then performed through the osteotomy wounds. Appropriate care of the patellar tendon was ensured during the entire procedure. The male part of the nail was inserted in an antegrade direction and fixed to the lowest point possible in the distal epiphysis. Next, the female part was inserted over the male part until the proximal threads of the female part were flushed with the tibial plateau. An anteromedial or anterolateral locking plate size 3.5 or 2.7 aiming to control the rotation was supplemented to the nail by 2 screws proximal to the osteotomy and 2 distal. All were bicortical if possible or unicortical if it was not feasible. The Ilizarov fixator was utilized using two proximal olive wires and two distal wires as a supplementary fixation method aiming to control the rotation of plate application, which was not feasible due to low bone stock.
Next, iliac crest autografting was done using the Smith– Peterson approach of the pelvis. An osteotome was used to open the ilium and to deeply separate both sides of the iliac tables (open-book technique). Using a curette, sufficient cancellous bone graft was obtained from both tables of the ilium. In addition, periosteal sleeve grafting was performed from the medial side of the ilium.
Before autograft was used at the surgical site, prophylactic fasciotomy was performed on all patients. A tunnel was made for cross-union, and dissection was performed from the tibia under the structures of the anterior compartment and over the interosseous membrane till the fibula was reached to allow direct communication between the fibula and the tibia. The periosteal sleeve harvested from the iliac site was then split into two pieces. Bone morphogenic protein-2 was added to the cancellous autograft. It was additionally applied to the interosseous membrane between the tibia and fibula at both tibial edges. The periosteal sleeve was then wrapped around the osteotomy site and tibia. An intramedullary K-wire was inserted in a retrograde direction in the fibula for supplemental fixation. The closure started with only subcutaneous layers, followed by the skin using the subcuticular technique. A full above-the-knee cast was applied to all patients for 3 months in patients who underwent tibial plating to minimize the strain on the osteotomy site and to allow callus formation.
Post-operative protocol
All patients were kept in the hospital for 3 days after surgery for pain control. Due to poor bone quality in pseudoarthrosis patients, non-weight-bearing mobilization was started on day 1 under the supervision of physical therapy. Departmental radiographs were obtained for all patients during the hospital stay. The cast was kept until the bones were healed, and cross-union was achieved, similar to the Ilizarov frame. The first visit was 2 weeks to assess the wound and reapply the cast. The next visit was 6 weeks after the index surgery, with a radiograph to assess union. Then, the next visit was 3 months to remove the cast after taking the radiographs if sufficient callus was present and to apply patellar tendon bearing orthosis at the same visit. The patient was referred to physical therapy to start knee and ankle range of motion exercises and gait training at that time. The brace was kept for 1 year after the index surgery.
Radiological outcome
Initially, the patients’ data obtained included sex, age at diagnosis, age during surgery, and duration of follow-up. The location of CPT was documented. We defined union as a callus found in all four cortices around the osteotomy site without the presence of a fracture line. Further information was obtained, including time until union was achieved, presence of leg length discrepancy (LLD), tibial malalignment, refracture, and cross union if present. Tibial alignment was measured using proximal tibial and ankle alignments.
Clinical outcome
The ankle and knee range of motion were assessed at the final visit. The need for further surgery was also documented.
Data analysis
Data were analyzed using SPSS 24.0 version statistical software. Descriptive statistics (mean, standard deviation, frequencies, and percentages) were used to describe quantitative and categorical variables. A P-value of equal or <0.05 and 95% confidence intervals were used to report the statistical significance and precision of the results.
RESULTS
Nine patients were previously diagnosed with NF-1 in the Pediatric Orthopedic Clinic for CPT. Male sex was predominant 5/9 (55.6%) and the mean age of the affected population at the index surgery was 6.11 ± 3.41. The mean follow-up duration after surgery was 17.33 months, with a minimum of 12 months. The characteristics of each patient are shown in Table 1.
| Patients | Gender | Age at the surgery (Years) | Follow-up duration (Months) | Fixation type | Union | Union duration (Months) | LLD (cm) | Proximal tibia valgus | Ankle valgus | Distal tibia hemi- epiphysiodesis |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 3 | 26 | FD+I | Yes | 3 | 2 | 94.5° | 122.5° | Yes |
| 2 | Female | 9 | 24 | FD+I | Yes | 6 | - | 93.4° | 84.9° | Yes |
| 3 | Male | 1 | 16 | FD+I | Yes | 4 | 3 | 90.5° | 107.0° | No |
| 4 | Male | 2 | 12 | FD+P | Yes | 4 | - | 95.6° | 116.4° | No |
| 5 | Female | 10 | 20 | FD+P | Yes | 6 | 4 | 89.9° | 84.2° | No |
| 6 | Female | 7 | 12 | FD+P | No | - | - | 84.3° | 113.8° | No |
| 7 | Male | 6 | 12 | FD+I | Yes | 7 | - | 88.3° | 115.9 | Yes |
| 8 | Male | 10 | 12 | FD+P | Yes | 6 | - | 91.6° | 110.5 | No |
| 9 | Female | 7 | 22 | FD+I | Yes | 3 | 4 | 93.2° | 89.3 | No |
FD: Fassier-Duval nail, I: Ilizarov fixator, P: Tibia plating, LLD: Leg length discrepancy, cm: Centimeters.
All patients underwent resection of the pseudoarthrotic segment, Fassier-Duval (FD) nailing, cross-tibia-fibula union, and iliac autograft. The fixation was supplemented with an Ilizarov external fixator in five patients [Figure 1], and the plate was used in four patients [Figure 2]. Most patients (88.9%) achieved a union of 4 cortices and cross-union with a mean of 4.88 ± 1.55 months from the surgery. The patient who did not achieve union had an infection requiring multiple surgical debridements, and healing was not achieved until the date of writing this paper. There were no reported refractures until the last visit of each patient to the clinic. The Chi-squared test showed no statistically significant difference between the age at the first surgery and bone union. The type of fixation was not significantly associated with the union rate.
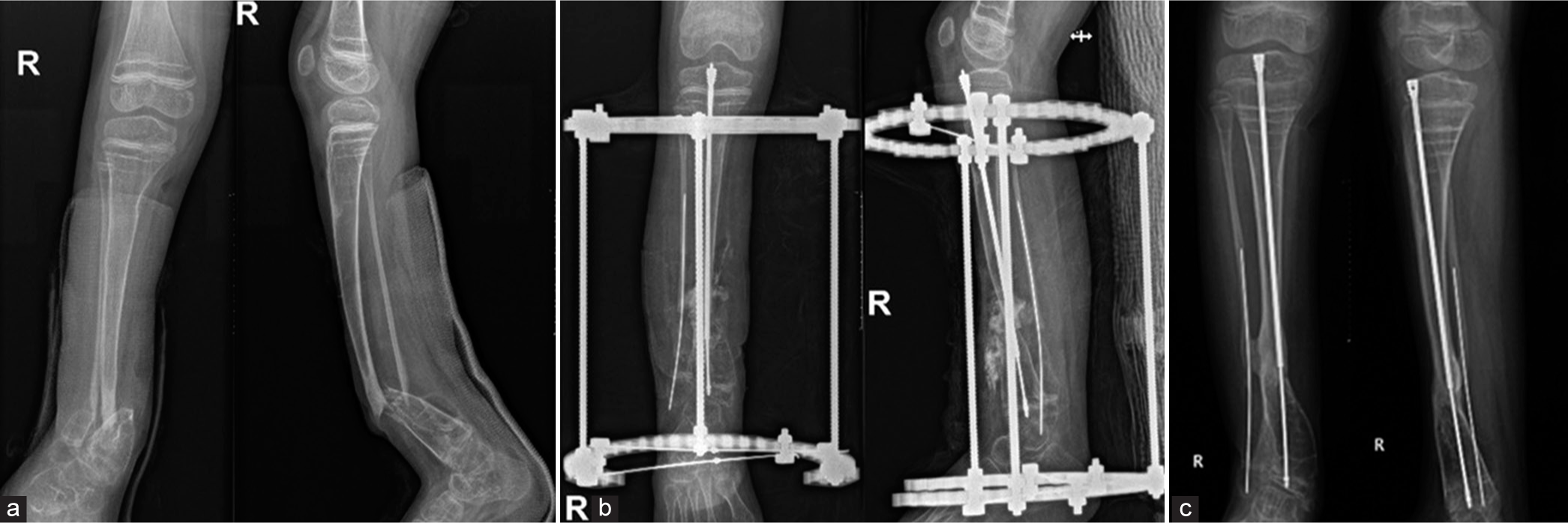
- Radiological images of a patient with congenital pseudoarthrosis of the tibia who was treated with Fassier-Duval nail and Ilizarov fixator, (a) shows a pre-operative radiograph, (b) was taken 1 day postoperatively, and (c) shows complete union after 4 months from surgery.
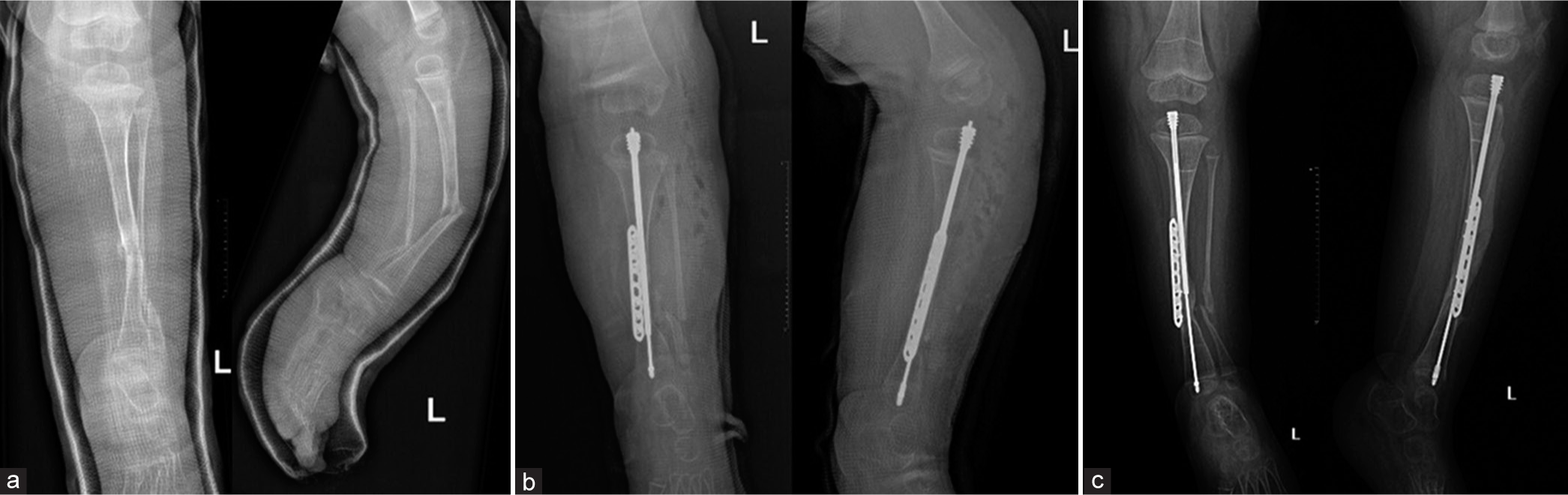
- Radiological images of a patient with congenital pseudoarthrosis of the tibia who was treated with Fassier-Duval nail and tibial plating. (a) shows a pre-operative radiograph, (b) was taken 1 day postoperatively, and (c) shows complete union after 4 months from surgery.
There were no reported immediate post-operative complications or donor-site morbidities. Superficial pin site infection at either half pin or wire entry site was noted in some patients. All patients who demonstrated pin site infection during follow-up were treated with oral antibiotics and daily dressing using wet gauze with normal saline covered by dry gauze.
The mean proximal and distal tibial angles were 91.26° and 104.94°, respectively. Five patients had proximal tibial valgus from the last visit radiographs, and most patients (6 out of 9) demonstrated ankle valgus. Three patients with ankle valgus required distal tibial medial epiphysiodesis. Significant LLD was reported in four patients, with a mean of 3.25 cm. The patient and his family were aware that the patient would require future lengthening surgeries.
At the last visit to the clinic, all patients could bear weight without pain, except for one patient with non-union. Knee stiffness was not reported in any patient, but ankle stiffness was reported in four patients. All the patients were instructed to use a clamshell orthosis until skeletal maturity.
DISCUSSION
CPT is a challenging disease that can present but not exclusively to patients with NF.[8] Achieving union and preserving the limb from refracture, LLD, and residual malalignment is difficult.[9] Most of the patients were exposed to many surgeries aiming to achieve union, which can complicate things, ending with large bone defects.[8,10] The optimal goal of CPT treatment is to achieve a united tibia, well-aligned leg, and functional limb without significant limb length discrepancy.[11]
Different surgical approaches are currently being used to achieve union and decrease the risk of complications. Most surgical techniques follow the same principles, including complete excision of pseudoarthrosis, rigid fixation, and bone grafting. The achievement of favorable outcomes has improved dramatically in recent years. Union has been achieved in 70% of cases after a single intervention, and amputation is rarely needed nowadays.[12] The traditional surgical method worldwide is the surgical excision of diseased segments and intramedullary rodding or circular external fixation using the Ilizarov frame. In a study by Akaro et al.,[5] intramedullary rodding or circular external fixation using the Ilizarov frame was used in 54.7% and 18.8% of cases, respectively. Of 54.7% who underwent intramedullary rodding, approximately 8.3% had a solid tibial union that used no external support or splint. In another study, the Charnley-Williams procedure was used, and full weight-bearing and unequivocal union was achieved in 48% of cases.[8] Plating as a fixation method is uncommon; according to a multicenter study that involved 73 patients in 32 different hospitals, plating and bone grafting were used in 5 patients, of whom 3 achieved union.[13] While the research field in CPT is growing, Paley described the cross-union method by creating a tunnel in the interosseous membrane between the tibia and fibula.[14] The union rate using this method reached 100% without any refracture cases.[14] This method has accelerated research to assess the efficacy of this technique. Shannon et al. found that using Paley’s technique, dual fixation and cross-union reached 100% union.[14] An “Eiffel Tower” double titanium elastic nailing and telescopic intramedullary rod have been tried as a method of fixation in combined surgical management for CPT, which has the advantage of less injury to the metaphysis and facilitating normal ankle functions.[11,15] A combination of intramedullary nailing and Ilizarov fixation has also been tried, showing higher effectiveness in treating CPT[9,10] and achieving initial union in 89.2% of patients with Crawford type-4 CPT.[16] Liu et al. showed that telescoping nails (FD nails), Ilizarov fixators, cross-union, and iliac bone grating had achieved a 100% union rate without refracture.[15] In patients who demonstrated good bone stock at the pseudoarthrosis site and to avoid Ilizarov fixator complications, a locking plate was used instead of an Ilizarov fixator in combination with a telescoping nail, which showed a similar union rate.[17]
Different techniques for bone grafting aiming to achieve union have been tried. In one study, an autogenous cortical bone graft was wrapped around the osteotomy site where the bone union was observed in 89.2% of patients.[10] A similar union rate was achieved in 88.9% of patients where an autogenous periosteal sleeve bone graft was used to wrap the osteotomy site in our study, given that an autogenous cancellous bone graft was placed in the osteotomy site in both procedures.
Complications for surgical management of CPT, such as refracture and LLD, are common, and a study showed that refracture occurred in nearly half of the patients who underwent intramedullary nailing and Ilizarov’s fixation technique. Refracture also occurred in 9 of the 52 patients who underwent vascularized fibular transfer.[12] With the Charnley-Williams method, persistent non-union or refracture was observed in only 3 of the 21 patients.[8] Two other studies reported that LLD was the predominant complication.[5,6]
Limb alignment should be preserved during treatment to avoid refracture.[8] In addition, an intramedullary nail device should be used as an internal splint.[8] Various surgical methods have been described in the literature and are debatable for treating CPT.[11] Historically, amputation was the treatment of choice for CPT patients because of the high rate of non-union to avoid repeated surgeries[18] and is now reserved for cases where failure of union occurred after multiple surgeries or in cases of significant LLD in a nonfunctional limb.[18] All the following surgical options are supplemented by resection of the pseudoarthrosis segment and bone graft use. The Ilizarov fixator alone provides the advantage of compressing the osteotomy site, which can help achieve union and allow the limb to be aligned properly during the healing phase.[16] The drawback of this method is risking refracture in almost 50% of patients after the hardware removal.[16] An intramedullary rod, or William’s rod, spans the ankle joint using a rod to provide further rigidity to the construct.[15] This technique increases the risk of ankle stiffness, but the union rate previously reported in this technique alone reached 50%.[8,15] Telescoping nails, where nails slide over each other during the growth of the long bone, are designed to avoid spanning ankle joints.[15] The disadvantage of this construct is that it might require exchange if the overlap between both parts of the nail is small, which might be separated during bone growth.[15]
Zhu et al. found that the union rate could reach 90% with a refracture rate of 26% by combining the intramedullary rod and Ilizarov fixator.[16] The authors’ technique was tested in a small series of patients for mid-term outcomes. The technique includes resection of the pseudoarthrosis segment, telescoping nail insertion, and iliac bone grafting supplemented with an Ilizarov fixator or locked plate, demonstrating an 88.9% union rate without refracture from the mid-term outcome. Union was encountered in one case due to deep infection, which required multiple procedures to eradicate the infection. Akaro et al. showed that patients who underwent index surgery before the age of 3 years had the worst outcomes.[5] This study did not find an association between age at initial surgery and the final outcome.
LLD is a well-recognized complication of CPT treatment. Nicolaou et al. demonstrated LLD with a mean of 2.5 cm using intramedullary rodding and Ilizarov’s fixation in 11 patients.[19] In addition, other studies have evaluated the amount of LLD after Ilizarov’s fixation and intramedullary nailing, which showed a mean of 3.34 cm and 1.7 cm, respectively.[9,11] In line with previous studies, LLD in our study was observed in 4 patients, of whom 3 were treated with intramedullary nailing and Ilizarov’s fixator. These results indicate a higher risk of LLD in patients with intramedullary nailing and Ilizarov’s fixator compared to intramedullary nailing and tibial plating as a fixation method. A significant LLD >2 cm requires further surgical procedures in the future for lengthening.
In another study, pin-site infections were as high as 23.5%.[11] In contrast to our study and that of Eamsobhana et al., pin-site infection was a minor complication.[9] In line with previous studies, pin-site infection was successfully treated in all patients using regular dressing and oral antibiotics.[9,11,16,20] In previous studies, the incidence of deep infection that required surgical debridement was 5.9% and 11.1%, respectively, in which Ilizarov’s fixator with intramedullary nailing was used as a fixation method.[11,21] In contrast, we had one patient with a deep infection in which intramedullary nailing and tibial plating were used. Ilizarov’s fixator and intramedullary nailing were used in which pin-site infection was observed only. Our study’s low incidence of deep infection could be attributed to the early recognition of pin-site infection and effective treatment to prevent further spread and subsequent devastating outcomes.
Yalikun et al. reported an incidence of proximal tibial valgus deformity and ankle valgus deformity of 22.2% and 38.9%, respectively.[20] Proximal tibial valgus deformity was seen in five of our patients; 3 of them underwent Ilizarov’s fixation with intramedullary nailing as a fixation method, and ankle valgus deformity was equally seen in three patients in both groups. Weight-bearing was achieved in all patients except for one in whom non-union occurred due to deep infection. In general, the final outcome was similar in both techniques in terms of achieving union and incidence of complications.
One important factor in decreasing the risk of refracture is using a brace postoperatively. In our study, a brace was applied to all patients at 3-month follow-up, and subsequently, refracture was not observed. This finding was in accordance with those of other studies that highlighted the role of postoperative orthosis in decreasing the risk of refracture.[7,8]
Limitations
Due to the rarity of the disease, we had a limited number of patients. In addition, the authors acknowledge the shortage of follow-up in this study and will consider long-term follow-up in a future study. Including two surgical techniques in this study compared to studies with one surgical technique has weakened our conclusion; thus, each technique should be studied separately to reach a more conclusive outcome in the future.
CONCLUSION
Patients who underwent intramedullary nailing in conjugation with Ilizarov’s fixator or plating to treat CPT and cross-union have achieved excellent union rates with no refracture in mid-term follow-up. A deep infection was noticed in one case, which was managed surgically with debridement. Residual deformities in the patient have been noticed and will require corrective surgery.
AUTHORS’ CONTRIBUTIONS
FH conceived and designed the study, conducted research, and provided research materials. YS and RR collected and organized data. AS and FS analyzed and interpreted data. FS and YS wrote the initial and final draft of the article. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The Institutional Review Board (IRB) at King Saud university, Riyadh, Saudi Arabia, approved the research on December 28, 2021, reference number 21/01232/IRB. Confidentiality of patient identities was maintained by converting the patient’s record number to coded numbers without names.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients’ legal guardians have given their consent for the patients’ images and other clinical information to be reported in the journal. The legal guardians understand that the patients’ names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Congenital pseudarthrosis of the tibia: The outcome of a pathology-oriented classification system and treatment protocol. J Pediatr Orthop B. 2020;29:337-47.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and treatment outcome of congenital pseudarthrosis of the tibia. J Child Orthop. 2013;7:157-66.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital pseudarthrosis of the tibia. Treatment and outcome at skeletal maturity in 10 children. Acta Orthop Scand. 1999;70:275-82.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital angulation of the lower leg and congenital pseudarthrosis of the tibia in Denmark. Acta Orthop Scand. 1972;43:539-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment outcomes of congenital pseudarthrosis of the tibia at Beit Cure International Hospital in Blantyre, Malawi. East Cent Afr J Surg. 2019;23:109-18.
- [CrossRef] [Google Scholar]
- Management of congenital pseudoarthrosis of the tibia and fibula. Curr Rev Musculoskelet Med. 2019;12:356-68.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstructive approaches in surgical management of congenital pseudarthrosis of the tibia. J Clin Med. 2020;9:4132.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital pseudarthrosis of the tibia: Results of technical variations in the Charnley-Williams procedure. J Bone Joint Surg Am. 2002;84:1799-810.
- [CrossRef] [PubMed] [Google Scholar]
- Combined Ilizarov fixation and intramedullary nailing for treatment of congenital pseudarthrosis of the tibia. J Med Assoc Thai. 2016;99:1086-93.
- [Google Scholar]
- Ilizarov fixator combined with an intramedullary nail for tibial nonunions with bone loss: Is it effective? Clin Orthop Relat Res. 2014;472:3892-901.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of the “Eiffel Tower” double titanium elastic nailing in combined management of congenital pseudarthrosis of the tibia: Preliminary outcomes of 17 cases with review of literature. BMC Musculoskelet Disord. 2021;22:490.
- [CrossRef] [PubMed] [Google Scholar]
- Controversies in the management of congenital pseudarthrosis of the tibia and fibula. Bone Joint J. 2013;95B:1027-34.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of congenital pseudarthrosis of the tibia: A multicenter study in Japan. J Pediatr Orthop. 2005;25:219-24.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-union surgery for congenital pseudarthrosis of the tibia. Children (Basel). 2021;8:547.
- [CrossRef] [PubMed] [Google Scholar]
- Application of the “telescopic rod” in a combined surgical technique for the treatment of congenital pseudarthrosis of the tibia in children. J Orthop Surg Res. 2021;16:532.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of intramedullary rod, wrapping bone grafting and Ilizarov's fixator for the treatment of Crawford type IV congenital pseudarthrosis of the tibia: Mid-term follow up of 56 cases. BMC Musculoskelet Disord. 2016;17:443.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital pseudarthrosis of the tibia: Biological and biomechanical considerations to achieve union and prevent refracture. J Child Orthop. 2019;13:120-33.
- [CrossRef] [PubMed] [Google Scholar]
- Amputation for congenital pseudarthrosis of the tibia. Indications and techniques. Clin Orthop Relat Res. 1982;166:58-61.
- [CrossRef] [Google Scholar]
- Congenital pseudarthrosis of the tibia: The results of an evolving protocol of management. J Child Orthop. 2013;7:269-76.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of the Ilizarov method and intramedullary fixation for the treatment of congenital pseudarthrosis of the tibia in children: A retrospective observational study. Front Surg. 2022;9:901262.
- [CrossRef] [PubMed] [Google Scholar]
- Association of Ilizarov's technique and intramedullary rodding in the treatment of congenital pseudarthrosis of the tibia. J Child Orthop. 2008;2:449-55.
- [CrossRef] [PubMed] [Google Scholar]







