Translate this page into:
An author’s guide to mastering academic writing skills: Discussion of a medical manuscript
-
Received: ,
Accepted: ,
How to cite this article: El-Sobky TA. An author’s guide to mastering academic writing skills: Discussion of a medical manuscript. J Musculoskelet Surg Res 2021;5:227-34
Abstract
Skilled scientific or academic writing is of great importance to research communication and journal publication ultimately. The four fundamental sections of a scholarly manuscript are introduction, methods, results and discussion. The discussion serves to interpret and analyze the study results in view of the existing body of evidence. Moreover, it serves to transform the usually rigid numerical statistical data of the results section into practical and clinically utilizable information. A well-formulated discussion can provide readers with informed decisions on the validity of the results and their exact generalizability to the broader community. It can also isolate shortcomings of the existing literature. Despite the extensive growth in biomedical publications lately, little attention has been paid to the importance of medical writing in general and to the discussion section of a medical manuscript in specific. This applies to curricular education and medical literature. The implications of well-executed studies with important findings can go unnoticed if authors are less skilled at writing a comprehensive discussion and conclusion among other manuscript sections. I intended to convey the experience I have accumulated in authoring and peer-reviewing for leading society journals and supervising in-house academic theses and dissertations. The objective of this article was to help authors present and communicate their research findings methodically, efficiently and impartially. Orthopedic research was taken as a practical example.
Keywords
Academic writing skills
Scholarly communication
Medical writing
Research report
Teaching
MEDICAL WRITING: NATURE AND EXTENT OF CHALLENGES
According to the National Library of Medicine https://www.nlm.nih.gov/bsd/stats/cit_ added.html, 952,919 biomedical publications worldwide have been indexed and added to MEDLINE during the fiscal year 2020. Despite this enormous number of publications, relatively insufficient literature exists on how to systematically prepare and critically appraise a medical journal manuscript, including the discussion section [Figure 1].[1,2] The scholarly community is becoming aware of the importance of teaching scientific writing and research presentation or communication skills in various undergraduate and postgraduate curricula of medical schools worldwide.[3-9] The use of English as the language of instruction among non-native students and faculty has been blamed for reduced academic performance, increased levels of plagiarism in scientific writing[10,11] the increased need for professional medical writing services[12-16] and prompted educational approaches to overcome these challenges.[14-18] Likewise, publication pressures and hyper-competitive work environments have been blamed for reduced academic performance in terms of quality and integrity of reporting research findings in the discussion and conclusion sections of medical manuscripts [Figure 2].[19,20] All previous remarks call for more efforts to prioritize curricular and extra-curricular education to enhance research presentation and communication skills among authors and peer reviewers alike. And call for efforts to overcome barriers to efficient and professional research communication.[21] The objective of this review was to highlight the basic pitfalls occurring during the preparation of the discussion section of a medical manuscript. Another objective was to provide basic tips on how to write a comprehensive and scientifically insightful discussion with orthopedics as a practical example.

- Principal phases of the research process.
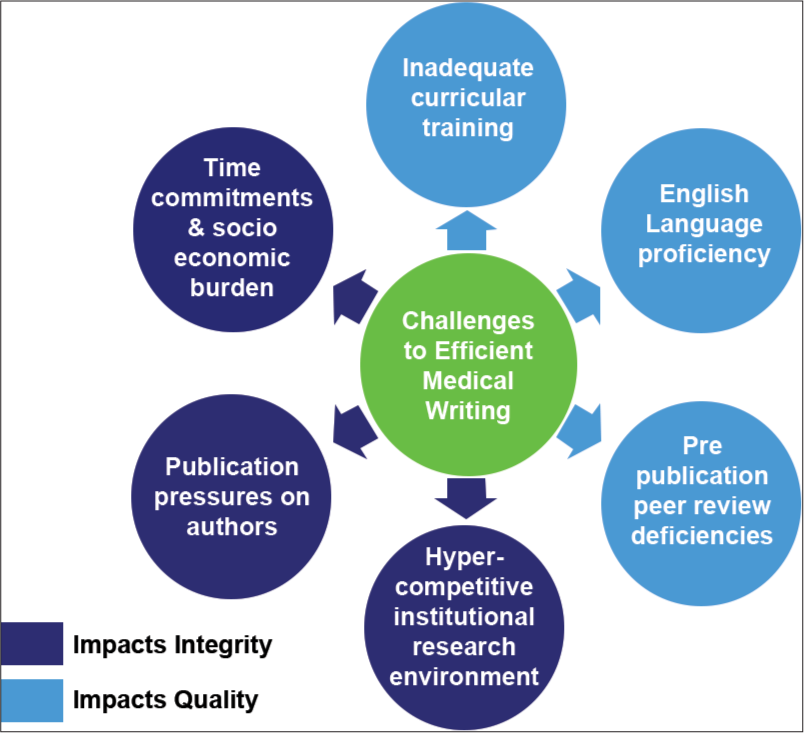
- Challenges to efficient medical writing.
FUNCTIONS OF THE DISCUSSION
The discussion section of a medical manuscript aims at putting the results into meaningful clinical practice and public health context.[22] In other words, a properly presented discussion can help readers understand the implications and limitations of the study results when applied to both the specific patient population studied and to the wider array of patient populations. The discussion section is the right place to draw relevant correlations between one’s work and similar works in a contextual manner. In addition, make leading inferences from the results and provide credible reasoning, especially behind any seemingly unexpected results a study may yield.[22-24]
Generally speaking, busy clinicians are most interested in the discussion section and its implications for their clinical practice than the typically sophisticated details of a study methodology. Likewise, busy academics are most interested in contrasting the results with their previous research findings and implications for future research topics. A robust discussion is the only available tool to simplify and transform the results section’s rigid and complex statistical data into scientifically meaningful and clinically utilizable information.[22] An efficient discussion should also caution readers against the routine generalization of the study results to the broader disease population and warn readers of absolute and unjustified belief in the validity of the results. On the other hand, an inaccurately written discussion could distort the true implications of research and intended messages to readers.[22] This particular scenario can occur despite an otherwise well-designed, well-performed, and bias-controlled research work. This happens because the academic skills needed to design and perform research differ from those needed to present and communicate research.
STRUCTURING THE DISCUSSION
Designing a general framework of ideas is indispensable to the production of a relevant and informative discussion. The first subsection of the discussion should present a summary of evidence and key points of the study’s results. The focus of this subsection should pivot on answering the research question. The authors are required to comment on, compare and correlate their results with similar works but not repeat and detail them. In addition, the authors’ own inferences from the results, suggestions and any novelty of findings should appear in this subsection. The second subsection can include the study’s limitations and strengths and its implications for upcoming research designs. A final subsection should be dedicated to writing a carefully curated conclusion that is in line with study results.[22] In addition, relevant recommendations that include future research plans should appear in this subsection. The clarity of English is ultra-important to conveying the true scientific meaning. Ambiguous and low-quality language can cause reader confusion and distraction. Tips for writing a purposeful discussion are presented in Table 1.
|
ESTABLISHING STUDY ASSOCIATIONS
Authors are advised not to restrict the discussion to comparing study results with others totally. Although important, this is not the only function of the discussion section. The notion that the discussion section is mainly restricted to comparing one’s study results with other published literature rests on a misconception. Rather, authors should draw inferences from these studies based on evidence, scientific reasoning and careful review of their methodological robustness. Authors should also indicate possible avenues for future research and focus on study limitations and strengths and so forth.[22-24]
Do not discuss each author/article separately and extensively rather, discuss similar or contrasting concepts or findings collectively and concisely. Instead, a manuscript can group relevant authors/articles sharing common findings or providing similar messages, write a single paragraph about their viewpoint and reference it accordingly. This represents a more organized, efficient and reader-friendly mode of scientific writing. It also presents a logical flow of scientific ideas. Each manuscript requires more attention to word economy and journals’ specific requirements.[22-24]
Authors should avoid comparing the results with similar studies in an absolute manner. When comparing one’s study results with similar studies, one should draw correlations contextually and within the confinements of these studies’ limitations and strengths. For example, similar studies with apparently similar findings may still exhibit scientifically relevant discrepancies regarding various research settings as authors’ level of expertise -especially in interventional studies-, environmental, racial, socioeconomic, and health-policy related factors. Failure to compare studies contextually and not absolutely might lead to overstatements or understatements and subsequent misleading conclusions.[22-24] Authors are required to avoid drawing comparisons based exclusively on numerical parities or disparities between their study and the literature. Such comparisons are often devoid of practical clinical context. For example, if the prevalence of cerebral palsy in a low-resource country equates to that of a rich/developed country, one has to look into the infant mortality rate and epidemiological research methodology used to calculate this prevalence in each study.[25]
SEARCHING FOR STUDY IMPLICATIONS
Do not forget to consider the applicability of research methodologies and outcomes to different disease and patient populations. Discussing the remote and broad implications of scientific concepts and principles is just as trustworthy as discussing specific details, for example, of a specific technique or methodological approach. Research concepts apply by default to a wider area of knowledge, which can be extrapolated to diverse clinical scenarios.[22,25] Therefore, it is crucial to discuss the implications of research findings for practice beyond the specific settings in which one’s research originated. For example, the concept or premise behind a certain surgical technique or drug therapy protocol in a carefully selected pediatric patient population may be potentially relevant to an adult patient population with a similar disease. Likewise, the validation and adaptation of a new assessment tool on a specific pediatric orthopedic patient population as cerebral palsy may be potentially relevant to other subtypes of the same disease or even to different disease populations like those with other forms of childhood-onset motor developmental delays.[26]
Further, it may be relevant to draw broad correlations between similar methodological approaches in spite of the fact that they are implemented on two entirely different disease populations. For example, it may be scientifically insightful to discuss the implications and potential limitations of survey research aimed at demonstrating surgeons’ preferences and perspectives on the diagnosis and management of developmental dysplasia of the hip[27] and ankle equinus in cerebral palsy children.[28] In that regard, the point of interest would be how survey research can uncover knowledge to practice gaps in pediatric orthopedics? Authors must not forget to make personal inferences from the study results and suggestions or recommendations for decent future research points. This is likely a commonly overlooked aspect of the discussion, especially among early career researchers. Authors are encouraged to make relevant inferences from the study’s data and provide scientifically sound and new assumptions, especially for unexplained and unexpected study findings.[22] This becomes a strategy of critical importance to the discussion when rare diseases with insufficiently understood underlying pathoetiologies are studied. Authors are equally encouraged to suggest future research avenues. This can be based upon accommodating for limitations of their own study or on suggesting new research questions or designs that the study’s results may have dictated. A future research design may include studying a relevant correlation between two factors that have not been addressed in one’s study because of its scope. It may also be wise to suggest a research question that accommodates for bias control of an important confounding variable that has not been accommodated for in one’s study. For example, survey research aimed to compare the general orthopedic versus pediatric orthopedic surgeons’ preferences for managing ankle equinus in cerebral palsy children.[28] In the discussion of the previous study, it may be insightful to suggest a new research question, namely, comparing the preferences of pediatric orthopedic surgeons with in-depth clinical experience in cerebral palsy and pediatric orthopedic surgeons without such an experience.
CITING THE LITERATURE
Authors must not underestimate the importance of reference selection. Credible references are essential to support the claims the manuscript presents. A comprehensive and updated literature search is paramount to promoting the research question and providing due justification of its importance or novelty. Citation/reference irrelevance, outdatedness, and low-quality and low-level evidence references can undermine the trustworthiness of an otherwise systematically conducted research.[29-33] In addition, quotation errors can produce a similar effect.[33,34] Beware, old references are not necessarily outdated. However, references reporting information that has been surpassed in terms of scientific validity and reliability are regarded as such and should be used in a historical or chronological context only. Citing studies based solely upon reading the conclusion section or abstract only can result in an inconclusive and counterproductive discussion. This is because the conclusion of any particular study may occasionally misrepresent the true findings of the study.[33,35] Authors are advised to self-revise the methodology and results of any cited study to verify the claims stated in the conclusion or abstract. Authors should avoid citing quoted references and are urged to read the original references thoroughly. Relatedly, assertions made by authors of review articles about certain references should not be taken for granted. Authors should also avoid writing a biased discussion. Therefore, they should be keen to present all conflicting or controversial viewpoints on the research question in a scientifically impartial manner.[19,36] Note that initially captured references may need to be updated by the time one starts writing the discussion section. The unwary inclusion of references from predatory journals to support statements made in the discussion can be counterproductive in many ways. It can lead to the production of inaccurate or baseless study conclusions and contaminate the scientific literature in general.[37-39]
STUDY LIMITATIONS AND STRENGTHS
Elaborating on study limitations helps readers to interpret the research findings within a proper scientific context and plan their future research accordingly.[22,24] Failure to do so may devalue an otherwise high-quality study. For example, limitations may be related to various factors as optimal appropriateness of the chosen research design or study type for the study objectives, sample numbers, degree of sample homogeneity, methodological performance bias, the validity of a scoring system, post-intervention follow-up period and logistic barriers and so forth. Authors should also make a distinction between study limitations arising from the above-mentioned research-related factors and those arising from an inherent patient- or disease-related factor as disease rarity or lack of definitive and recognized disease diagnostic tools and so forth. If study limitations are deemed critical to the interpretation of the study findings, present them under a separate subtitle. Noteworthy, serious and preventable methodological flaws that fundamentally affect the validity and reliability of the study’s conclusions are not considered study limitations, for example, failure to recognize or develop a methodological strategy to deal with confounding variables of significance. These flaws are generally irreparable, incompatible with sound science. Any discussion or conclusions based on such serious flaws are groundless.[40]
Study strengths and limitations are equally crucial to the interpretation of the results and conclusions. Study strengths may relate to the same above-mentioned factors for study limitations. Study strengths are likely to impact the validity, generalizability of conclusions positively. Pinpointing the study strengths can help readers rank the level of evidence and trustworthiness of a study’s results and its conclusions. They may represent a form of innovation in research that should be explicitly revealed to readers. For example, compensating for a methodological deficiency of a previous study performed on the same patient population and that addressed the same research question is one form of innovation and strength in research. Similarly, the study of a certain research point employing a different research type, for example, a randomized control trial instead of a previously reported non-randomized trial may help build evidence on the same research point. Alternatively, employing a different research methodology, for example, a subjective physician survey study instead of an objective patient interventional study may constitute another form of innovation and study strength. Likewise, redoing a research topic while overcoming inconsistencies of the previously implemented assessment tool or applying the same surgical technique to treat the same orthopedic deformity in an unexplored patient population are other forms of innovation and strength in research. For example, reusing the already established guided growth technique to correct angular knee deformities in an unexplored population as children with nutritional rickets is worthy of emphasis in the discussion.[41]
PREPARING FINAL STUDY CONCLUSIONS
The conclusion is usually the most eye-catching part of a manuscript, especially among busy clinicians. However, a scientifically inaccurate or poorly worded conclusion can be misleading and put patients at risk of complications. Therefore, caution should be exercised when phrasing the conclusion, especially regarding undue generalizations beyond the confinements of the studied patient population or the subtype of the investigated disorder and so forth. The same applies to the undue or full justification of the validity of the results. Likewise, conclusions should be articulated in light of the follow-up period in interventional studies, even if results were correctly generalizable to a larger population. Shortly said, one should keep an eye on the study limitations and avoid concluding remarks that are not substantiated by the study results. Moreover, avoid writing overinflated or exaggerated study conclusions.
The conclusion of a manuscript and summary of the results is occasionally used interchangeably by some early career researchers. Actually, they represent two distinct entities of a medical manuscript. The summary of the results represents a brief description of the overall results and statistical analysis. Contrastingly, the conclusion represents the inferences drawn from these occasionally complex numerical/statistical results and their linguistic interpretation in view of the existing academic and clinical evidence.[22] Thus, authors should not simply write a summary of study results as concluding remarks, rather interpret or write down the implications of the results to both clinical practice and public health. Failing to do so can deprive readers of a practical take-home message and limits the clinical utility of research. Beware to avoid misinterpreting the results and writing discrepant conclusions. Never equate statistical significance to clinical significance.[42]
Authors are required to make a clear distinction between statistical significance and clinical significance when formulating their final conclusions. This is because the statistical significance of results calculated according to P-value may not parallel the clinical significance or relevance of a given patient outcome. This is particularly important for quantitative research, be it primary or secondary as meta-analysis. A well-performed meta-analysis cannot compensate for the inherent methodological flaws of the included studies. For example, a correctly calculated P-value for plain radiologic or functional outcome measure in an interventional (pre-post) study may reveal a statistically significant improvement of the measured outcome. However, despite the difference, the improvement remains clinically irrelevant or does not reach the minimum clinically important difference to be considered of value by patients. In such scenario, basing one’s conclusions on the statistical significance is misleading and clinically meaningless. Consequently, conclusions based solely on statistical values without contextual clinical interpretation can lead to unverified and erroneous interpretations. Dissemination of such erroneous take-homes among unwary or busy medical practitioners may put patients at risk of harm and practitioners at risk of malpractice. Authors must ensure that the conclusions at the end of the main manuscript are in complete agreement with those written in the abstract section. Common pitfalls of writing study conclusions are shown in Figure 3. Practical tips for improving the academic writing skills of early-career authors are presented [Table 2]. Authors who resort to medical writing services must acknowledge that in their manuscript. Unacknowledged medical writing services are usually referred to as ghostwriting, which is ethically concerning.[47-49]

- Common pitfalls of writing study conclusions.
TAKE-HOME MESSAGE
The discussion section of a medical manuscript is a principal means to convey the importance and relevance of a study’s outcomes to clinical practice and public health issues. Without adequate academic skills to present an intellectual discussion and conclusion, the clinical utility of research findings may go largely unknown to readers. This may also lead to wasteful, misleading and occasionally harmful research outputs. Therefore, academic skills required to conceptualize, design and implement research should go hand in hand with skills required to present and communicate research.
|
AUTHOR’S CONTRIBUTION
The author has critically reviewed and approved the final draft and is responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The author confirms that this review had been prepared in accordance with COPE roles and regulations. Given the nature of the review, the IRB review was not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
This review did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
There is no conflict of interest.
References
- Scientific medical writing in practice: The “IMR@ D®” format. Tunis Med. 2019;97:407-25.
- [Google Scholar]
- Tips for charting the course of a successful health research career. J Multidiscip Healthc. 2013;6:163-8.
- [CrossRef] [PubMed] [Google Scholar]
- Critical thinking and scientific writing skills of non-anglophone medical students: A model of training course. J Korean Med Sci. 2019;34:e18.
- [CrossRef] [PubMed] [Google Scholar]
- Fostering critical thinking and collaborative learning skills among medical students through a research protocol writing activity in the curriculum. Korean J Med Educ. 2018;30:109-18.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching students how to read and write science: A mandatory course on scientific research and communication in medicine. Acad Med. 2003;78:1235-9.
- [CrossRef] [PubMed] [Google Scholar]
- Supporting the writing productivity of biomedical graduate students: An integrated, structured writing intervention. CBE Life Sci Educ. 2018;17:ar45.
- [CrossRef] [PubMed] [Google Scholar]
- Scientific writing workshop improves confidence in critical writing skills among trainees in the biomedical sciences. J Microbiol Biol Educ. 2020;21:21.
- [CrossRef] [PubMed] [Google Scholar]
- Going beyond “not enough time” Barriers to preparing manuscripts for academic medical journals. Teach Learn Med. 2020;32:71-81.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review highlights a knowledge gap regarding the effectiveness of health-related training programs in journalology. J Clin Epidemiol. 2015;68:257-65.
- [CrossRef] [PubMed] [Google Scholar]
- Plagiarism in the context of education and evolving detection strategies. J Korean Med Sci. 2017;32:1220-7.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching science subjects in Arabic: Arab university scientists' perspectives. Language Learn Higher Educ. 2015;5:105-23.
- [CrossRef] [Google Scholar]
- Barriers to publishing in biomedical journals perceived by a sample of French researchers: Results of the DIAzePAM study. BMC Med Res Methodol. 2017;17:96.
- [CrossRef] [PubMed] [Google Scholar]
- Navigating scholarly writing and international publishing: Individual agency of Taiwanese EAL doctoral students. J Engl Acad Purposes. 2017;27:1-13.
- [CrossRef] [Google Scholar]
- Chinese academics writing for publication: English teachers as text mediators. J Second Lang Writ. 2016;33:43-55.
- [CrossRef] [Google Scholar]
- How to incorporate academic writing pedagogy in undergraduate and postgraduate medical education. Wiad Lek. 2018;71:261-5.
- [Google Scholar]
- Introducing scientific writing as mandatory topic in bachelor nursing program experience of the university of Dubrovnik, Croatia. Acta Clin Croat. 2016;55:195-202.
- [CrossRef] [PubMed] [Google Scholar]
- Language of written medical educational materials for non-English speaking populations: An evaluation of a simplified bi-lingual approach. BMC Med Educ. 2019;19:418.
- [CrossRef] [PubMed] [Google Scholar]
- Mother tongue as the medium of instruction at developing country universities in a global context. S Afr J Sci. 2015;111:5.
- [CrossRef] [Google Scholar]
- Individual, institutional, and scientific environment factors associated with questionable research practices in the reporting of messages and conclusions in scientific health services research publications. BMC Health Serv Res. 2020;20:828.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived publication pressure in Amsterdam: Survey of all disciplinary fields and academic ranks. PLoS One. 2019;14:e0217931.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to conduction or completion of research projects among orthopedic surgeons in Saudi Arabia. J Musculoskelet Surg Res. 2021;5:103-8.
- [CrossRef] [Google Scholar]
- The principles of biomedical scientific writing: discussion. Int J Endocrinol Metab. 2019;17:e95415.
- [CrossRef] [Google Scholar]
- How to write a scientific manuscript for publication. Blood Transfus. 2013;11:217-26.
- [Google Scholar]
- Preparing manuscript: Scientific writing for publication. Indian J Anaesth. 2016;60:674-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of early childhood disability in a rural district of Sind, Pakistan. Dev Med Child Neurol. 2013;55:357-63.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring outcomes in children with cerebral palsy In: Miller F, Bachrach S, Lennon N, O'Neil M, eds. Cerebral Palsy. Cham: Springer; 2019.
- [CrossRef] [Google Scholar]
- Diagnostic and treatment preferences for developmental dysplasia of the hip: A survey of EPOS and POSNA members. J Child Orthop. 2018;12:236-44.
- [CrossRef] [PubMed] [Google Scholar]
- Current practice and preferences to management of equinus in children with ambulatory cerebral palsy: A survey of orthopedic surgeons. SICOT J. 2019;5:3.
- [CrossRef] [PubMed] [Google Scholar]
- The Principles of biomedical scientific writing: Citation. Int J Endocrinol Metab. 2020;18:e102622.
- [CrossRef] [Google Scholar]
- Accuracy of citation and quotation in foot and ankle surgery journals. Foot Ankle Int. 2013;34:949-55.
- [CrossRef] [PubMed] [Google Scholar]
- MyCites: A proposal to mark and report inaccurate citations in scholarly publications. Res Integr Peer Rev. 2020;5:13.
- [CrossRef] [PubMed] [Google Scholar]
- How accurate are citations of frequently cited papers in biomedical literature? Clin Sci (Lond). 2021;135:671-81.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of cited “facts” in medical research articles: A review of study methodology and recalculation of quotation error rate. PLoS One. 2017;12:e0184727.
- [CrossRef] [PubMed] [Google Scholar]
- Reference accuracy in peerreviewed pediatric orthopaedic literature. J Bone Joint Surg Am. 2010;92:1155-61.
- [CrossRef] [PubMed] [Google Scholar]
- Manuscript referencing errors and their impact on shaping current evidence. Am J Pharm Educ. 2020;84:ajpe7846.
- [CrossRef] [PubMed] [Google Scholar]
- Financial conflicts of interest of United States-based authors in neurology journals: Cross-sectional study using the open payments database. Neurology. 2021;96:e1913-20.
- [CrossRef] [PubMed] [Google Scholar]
- The perils of predatory journals and conferences. Malays Orthop J. 2020;14:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Predatory journals: a major threat in orthopaedic research. Int Orthop. 2019;43:509-17.
- [CrossRef] [PubMed] [Google Scholar]
- Predatory journal preference in the field of Orthopaedics and Traumatology in Turkey. Acta Orthop Traumatol Turc. 2019;53:390-3.
- [CrossRef] [PubMed] [Google Scholar]
- Growth modulation for knee coronal plane deformities in children with nutritional rickets: A prospective series with treatment algorithm. J Am Acad Orthop Surg Glob Res Rev. 2020;4:e19.00009.
- [CrossRef] [PubMed] [Google Scholar]
- Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31:337-50.
- [CrossRef] [PubMed] [Google Scholar]
- Essential components of educational programs on biomedical writing, editing, and publishing. J Korean Med Sci. 2015;30:1381-7.
- [CrossRef] [PubMed] [Google Scholar]
- Integrating research into the undergraduate curriculum: 1 Early research experiences and training. J Undergrad Neurosci Educ. 2020;19:A52-63.
- [Google Scholar]
- Peer review of manuscripts: A valuable yet neglected educational tool for early-career researchers. Educ Res Int. 2019;2019:1359362.
- [CrossRef] [Google Scholar]
- Co-reviewing and ghostwriting by early-career researchers in the peer review of manuscripts. Elife. 2019;8:e48425.
- [CrossRef] [PubMed] [Google Scholar]
- Author attitudes to professional medical writing support. Curr Med Res Opin. 2014;30:2103-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ghostwriters in the scientific world. Pan Afr Med J. 2018;30:217.
- [CrossRef] [PubMed] [Google Scholar]
- Professional medical writing support: The need of the day. Perspect Clin Res. 2018;9:111-2.
- [CrossRef] [PubMed] [Google Scholar]







