Translate this page into:
An iatropathic tibial nerve injury in a patient following total ankle replacement
2 Birmingham Hand Centre, Peripheral Nerve Injury Service, Queen Elizabeth Hospital, Birmingham, UK
Corresponding Author:
Dominic M Power
The Peripheral Nerve Injury Service, Department of Orthopaedic Surgery, University Hospitals Birmingham, NHS Foundation Trust, Birmingham
UK
dominic.power@uhb.nhs.uk
| How to cite this article: Jones RD, Turner LC, Jimulia DT, Power DM. An iatropathic tibial nerve injury in a patient following total ankle replacement. J Musculoskelet Surg Res 2019;3:169-172 |
Abstract
Ankle arthroplasty is an infrequent procedure, and there is a risk of injury to nearby neurovascular structures from direct injury and from traction. The risk of nerve injury is difficult to quantify due to low-procedure numbers, non-mandatory nerve injury reporting to the National Joint Registry in the UK and delayed recognition of nerve injury despite the British Orthopaedic Association Standards for Trauma 5 guidelines on the management of peripheral nerve injury. Neuropathic pain following a major joint procedure with disordered sensation, motor paralysis and alterations in autonomic function in the distal skin are suggestive of nerve injury. A Tinel's sign at the site of suspected injury is diagnostic and the nerve should be promptly explored by a surgeon familiar with the operative assessment and reconstruction options for nerve injury. Processed nerve allograft is a useful adjunct in the reconstruction algorithm in cases of non-critical nerve disruption and central sensitisation to avoid the harvest of an intact sensory autologous nerve and risking further exacerbation of neuropathic pain at another site. The case presented discusses an iatropathic tibial nerve injury in a 48-year-old man who underwent reconstruction using nerve allograft.
Introduction
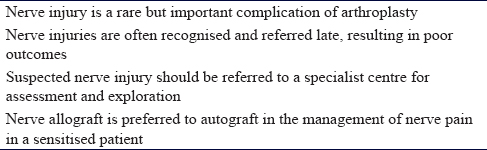
Over 230,000 arthroplasties were performed in England, Wales and Northern Ireland in 2017. Of these, ankle arthroplasty constituted 0.4%; although, their popularity is rising.[1] A rare but important complication of arthroplasty surgery is an injury to a peripheral nerve. During total ankle replacement (TAR), the superficial and deep peroneal nerves are at risk during the exposure, and the tibial nerve at the posteromedial ankle is at risk of direct or traction injury during instrumentation and manipulation of the ankle. Nerve injuries may become apparent in the early post-operative stage when neuropathic pain, sensory disturbance, motor paralysis and cutaneous autonomic changes (dry, warm, red skin from the loss of autonomic sudomotor and vasomotor function) should prompt a careful examination of the affected nerve. A strong Tinel's sign elicited by tapping over the course of the nerve may reveal the site of injury. Early referral to a peripheral nerve injury specialist will enable surgical inspection of the nerve and reconstruction when necessary. Commonly nerve injuries associated with joint arthroplasty are diagnosed and referred late after excluding other causes of the problematic, painful arthroplasty. Late diagnosis of a nerve injury is associated with opiate dependence and chronic pain syndromes, including central sensitisation. In late cases, regional anaesthetic blocks are essential in confirming that a nerve is the source of pain. Surgical techniques include neurolysis, nerve wrapping with collagen barriers, resection of neuromata and reconstruction using autologous sensory nerve graft or processed nerve allograft. Allograft is preferred for non-critical sensory reconstruction in a sensitised individual. Nerve transfers may be used for reinnervation of critical muscle targets distal to the site of injury. This case report highlights the risk of iatropathic nerve injury during arthroplasty and the importance of rapid clinical diagnosis and appropriate treatment.
Case Report
A 48-year-old man had traumatic osteochondral lesions of his talus that remained painful despite two microfracture treatment episodes. The ankle deteriorated with moderate post-traumatic osteoarthrosis and he was offered a TAR. Immediately postoperatively, he reported severe neuropathic pain over his medial malleolus radiating down into the sole of his foot. The pain persisted, and on outpatient review, a tibial nerve injury was suspected by the operating surgeon who referred the patient for an ultrasound of the tibial nerve. The scan demonstrated a bone fragment deep to the tibial nerve causing nerve compression 2 cm proximal to the medial malleolus.
The surgeon re-explored the tibial nerve 11 weeks postoperatively. The tibial nerve was noted as being in continuity, although atrophic, and the bony fragment was removed. Unfortunately, the neuropathic pain worsened and he requested the second opinion. The second foot and ankle specialist referred him to the regional peripheral nerve injury service (PNIS) for an opinion.
On assessment at the regional PNIS, it was noted that the patient was opiate dependent using oral and patch medication and a maximum dose of an oral neuromodulatory agent. The neuropathic pain was severe with pseudoparalysis of the ankle due to neurostenalgia. There was a strong Tinel's sign over the tibial nerve above the ankle and foot intrinsic muscle paralysis. The medial calcaneal sensation (calcaneal branch) was dysaesthetic with anaesthesia in the medial and lateral plantar nerve territories and dry, erythematous and atrophic skin on the plantar surface. There was mild sensitivity in the superficial peroneal territory on the anterior ankle scar and in the saphenous nerve distribution.
An isolated block of the tibial nerve reduced his pain by 80% and settled the marginal hypersensitivity in the superficial peroneal and saphenous nerve territories. The tibial nerve was surgically explored starting proximal to the original exposure in normal tissue. There was an extensive scar around the tibial neurovascular structures with the loss of normal epineurium in the lateral and posterior aspects of the tibial nerve, which was firm without normal architecture. The scar caused tethering to the posterior ankle capsule, which was breached with synovial fluid tracking deep to the Achilles tendon, partial injury to the flexor hallucis longus tendon with surrounding synovitis and a large bone fragment was identified tethering the nerve at the site of arthroplasty. The lack of muscle contraction at maximum stimulation of 6 mA showed no conduction across the damaged segment of the nerve. The medial calcaneal branch was intact after neurolysis [Figure - 1]. The bone fragment was removed, and the damaged tendon was debrided. The tibial nerve was dissected free from the posterior ankle scar and an external neurolysis performed. There was still no stimulation across the damaged segment. The nerve was evaluated using an operating microscope and the scar opened at the site of epineurial loss. There was no internal fascicle structure. The nerve was transected and serially debrided until a fascicle structure was identified and then further debridement proximally and distally until interfascicular scar was minimal. The resultant gap in full ankle dorsiflexion was 45 mm [Figure - 2]. The nerve gap was reconstructed using a 4–5 mm × 45 mm AVANCE® processed nerve allograft (AxoGen Inc., Alachua, Florida, USA) with interrupted 8'0 nylon sutures and supported with Tisseel™ fibrin glue (Baxter UK) [Figure - 3]. An indwelling nerve catheter was sited surgically proximal to the repair and removed after 48 h.
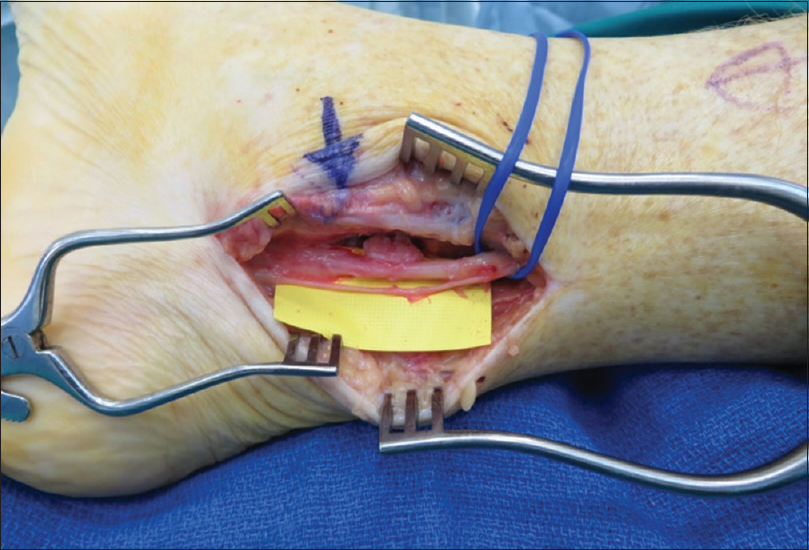 |
| Figure 1: Tibial nerve and medial calcaneal branch following neurolysis |
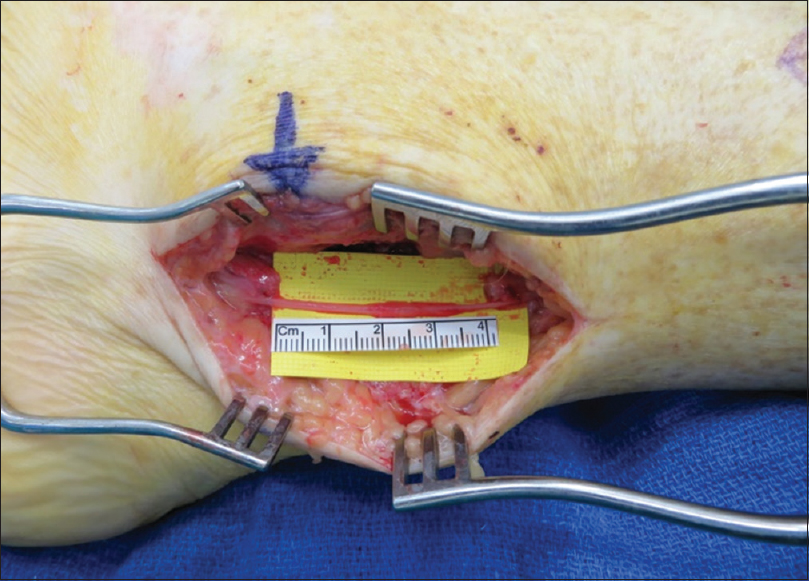 |
| Figure 2: 45-mm tibial nerve gap in full ankle dorsiflexion |
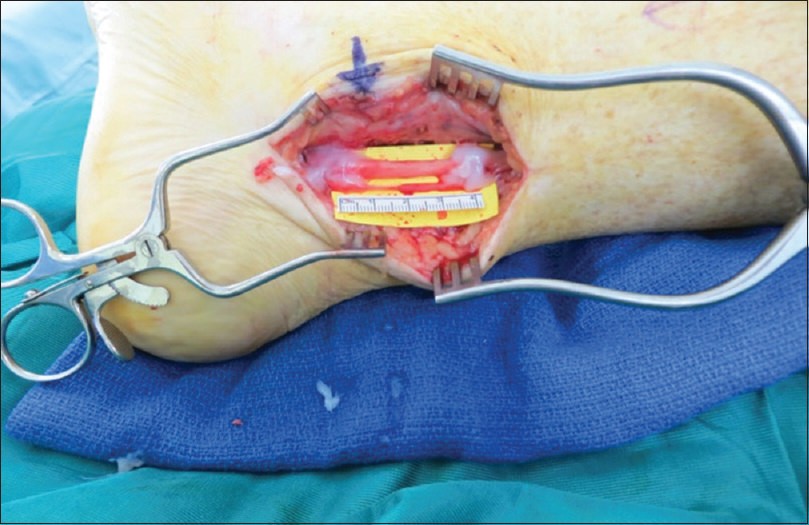 |
| Figure 3: Co-aptation of allograft supported with fibrin glue |
At 4 months postoperatively, there was evidence of reinnervation within the nerve allograft and sensory improvement in the calcaneal branch territory of the tibial nerve. A progressive Tinel's sign was detected at the tarsal tunnel indicating nerve regeneration through the allograft.
At 1-year follow-up, the patient reported visual analogue scale pain of 99/100, which showed no improvement from his pain pre-operatively although he has been able to decrease the dose of his opiate medications. There is a Tinel's sign into the tarsal tunnel; although, it is strongest at the distal co-aptation site. There is an excellent active and passive range of motion in the ankle and subtalar joint (20° dorsiflexion and 30° plantar flexion) and no neurostenalgia pain limiting active motion. As his ankle movement has improved, he can walk without walking aides. However, his continued pain means stairs and long distances prove difficult. He continues to experience numbness and tingling on the sole of his foot, with allodynia on walking barefoot. The skin has some sweating at the heel, but distal atrophy and dry skin persist at this stage. Protective sensation has returned to the heel.
Discussion
Neurologic injuries are uncommon but significant complications of arthroplasty. The incidence of nerve injury with TAR is not known although Primadi et al. reported a rate of 15.3%, with the tibial nerve the most frequently damaged.[2] Cadaveric dissection by Reb et al. demonstrated the tibial neurovascular structures to be at risk during TAR,[3] with McAlister et al. finding the superficial peroneal nerve to also be at risk.[4] As TAR rates increase, the prevalence of these neurologic complications will also increase. Prompt diagnosis of nerve injuries improves the chance of a successful outcome.
Neurologic injuries often present late, with a mean interval of 10 months between injury and appropriate treatment.[5] Delayed presentation results in more axon cell death, scar that impedes axonal regeneration, motor target deterioration and tropism. Nerve debridement will be more extensive, the nerve gap longer and a good outcome will be unlikely. A delay to diagnosis also increases the risk of central pain mapping (central sensitisation) and other chronic pain syndromes.
Early recognition of a potential nerve injury should prompt referral to a specialist who will determine through clinical examination whether surgical exposure of the nerve is warranted, will be more familiar with operative assessment of injured nerves and will be able to perform the most appropriate intervention or reconstruction. The British Orthopaedic Association Standards for Trauma 5 (BOAST5) guidelines emphasise the key signs and symptoms of a nerve injury and the neuropathic pain associated with a degenerative nerve lesion.[6] Tinel's sign and dry, red skin with sensory disturbance and motor weakness or paralysis are suggestive of axonal injury as opposed to a conduction block (neurapraxia).
Cadaveric allogenic nerve tissue (processed nerve allograft) now provide a practical alternative to autologous nerve grafts (autografts) and are supplied frozen and available in a range of sizes between 1–2 mm and 4–5-mm diameters and 15 mm–70 mm lengths. Allograft processing using enzymatic decellularisation leaves an endoneurial tube scaffold depleted of basement membrane neuro-inhibitory glycoproteins and mitigates the need for systemic immunosuppression.[7] The use of allografts negates donor site morbidity from autograft harvesting, including neuroma formation, paraesthesia, cold intolerance and allodynia.[8] AVANCE® processed nerve allograft (AxoGen Inc., Alachua, Florida, USA) was used in this case due to lateral plantar sensory preservation from the ipsilateral sural nerve and the unacceptably high risk of neuroma pain associated with contralateral sural nerve harvest in an already sensitised patient. The aforementioned learning points are summarised in [Table - 1].
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contributions
LCT, RDJ, DTJ and DMP conceived and designed the study and conducted the literature search. LCT, RDJ and DTJ wrote the initial draft supported by DMP's critical input. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | National Joint Registry. NJR Stats Online: Summary of Annual Statistics. Available from: http://www.njrcentre.org.uk/njrcentre/Healthcare-providers/Accessing-the-data/StatsOnline/NJR-StatsOnline. [Last accessed on 2018 Jan 15]. [Google Scholar] |
| 2. | Primadi A, Xu HX, Yoon TR, Ryu JH, Lee KB. Neurologic injuries after primary total ankle arthroplasty: Prevalence and effect on outcomes. J Foot Ankle Res 2015;8:55. [Google Scholar] |
| 3. | Reb CW, McAlister JE, Hyer CF, Berlet GC. Posterior ankle structure injury during total ankle replacement. J Foot Ankle Surg 2016;55:931-4. [Google Scholar] |
| 4. | McAlister JE, DeMill SL, Hyer CF, Berlet GC. Anterior approach total ankle arthroplasty: Superficial peroneal nerve branches at risk. J Foot Ankle Surg 2016;55:476-9. [Google Scholar] |
| 5. | Khan R, Birch R. Latropathic injuries of peripheral nerves. J Bone Joint Surg Br 2001;83:1145-8. [Google Scholar] |
| 6. | British Orthopaedic Association. The Management of Nerve Injuries: A Guide to Good Practice. London Google: British Orthopaedic Association; 2011. [Google Scholar] |
| 7. | Moore AM, MacEwan M, Santosa KB, Chenard KE, Ray WZ, Hunter DA, et al. Acellular nerve allografts in peripheral nerve regeneration: A comparative study. Muscle Nerve 2011;44:221-34. [Google Scholar] |
| 8. | Hallgren A, Björkman A, Chemnitz A, Dahlin LB. Subjective outcome related to donor site morbidity after sural nerve graft harvesting: A survey in 41 patients. BMC Surg 2013;13:39. [Google Scholar] |
Fulltext Views
3,798
PDF downloads
1,462





