Translate this page into:
Low back pain
Corresponding Author:
Nizar Abdulaziz Al-Nakshabandi
Professor of Radiology, Department of Radiology, College of Medicine, King Saud University, Riyadh
Saudi Arabia
nizar97@hotmail.com
| How to cite this article: Al-Nakshabandi NA. Low back pain. J Musculoskelet Surg Res 2018;2:180-181 |
History
A 27-year-old female presented with low back pain and weight loss, but no fever.
On physical examination, there was lower back tenderness, but no neurological deficit.
- What are the findings?
- What is the differential diagnosis?
- What are the causes?
- What is the diagnosis?
Findings
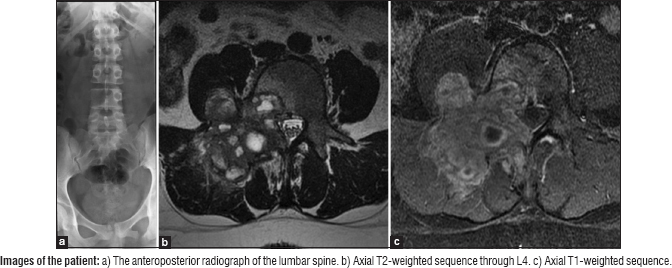
The anteroposterior radiograph of the lumbar spine (a) shows absence of the right pedicle of L4, with a possible lytic lesion seen.
Axial T2-weighted sequence through L4 (b) confirms an expansile lytic lesion involving the posterior elements of L4, namely the facet, pedicle, transverse process, and posterior one-third of the body of L4 measuring 3 cm × 3.5 cm. Notice the fluid/fluid levels (see arrow in b) within the possible central necrotic lesion.
Axial T1-weighted sequence (c) with intravenous infusion of gadolinium demonstrates a peripheral enhancement, with no compression on the spinal canal seen.
Differential Diagnosis
The differential diagnosis is that of FEGNOMASHIC. (This word has no meaning. It is a mnemonic to remember the differential diagnosis.) It is FEGNOMASHIC or FOG MACHINES
- F: Fibrous dysplasia or fibrous cortical defect
- E: Enchondroma or eosinophilic granuloma
- G: Giant cell tumor
- N: Nonossifying fibroma
- O: Osteoblastoma
- M: Metastasis(es)/myeloma
- A: Aneurysmal bone cyst (ABC)
- S: Simple (unicameral) bone cyst
- H: Hyperparathyroidism (brown tumor)
- I: Infection (osteomyelitis)
- C: Chondroblastoma or chondromyxoid fibroma.
However, since there is evidence of fluid/fluid level on magnetic resonance imaging, this should limit the differential diagnosis to ABC, giant cell tumor, osteoblastoma, fibrous dysplasia, chondroblastoma, and telangiectatic osteosarcoma. Since it is in the spine in a relatively young patient and due to the nonaggressive appearance on plain film, the ABC is strongly considered.
Diagnosis
The diagnosis is of ABC of the fourth lumbar vertebra based on computed tomography-guided biopsy.
Pearls and Discussion
The differential diagnosis of fluid level is ABC, simple bone cyst, or telangiectatic osteosarcoma. Rare causes such as metastasis, synovial sarcoma, synovial hemangioma, or myositis ossificans can be implemented.
On a pathological level, ABCs are blood-filled spaces of variable sizes with an interconnecting connective tissue. These can be primary; however, they could be secondary in an underlying lesion such as chondroblastoma, fibrous dysplasia, giant cell tumor, or osteosarcoma.
Treatment of these lesions is with curettage and bone grafting. However, there is a risk of recurrent straight up to 20%. Percutaneous image-guided treatment with fibrosing agents can be an option or surgical excision. Interventional embolization is another treatment option that can be used depending on the location and extent of the lesion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Further Readings
- Murphey MD, Andrews CL, Flemming DJ, Temple HT, Smith WS, Smirniotopoulos JG, et al. From the archives of the AFIP. Primary tumors of the spine: Radiologic pathologic correlation. Radiographics 1996;16:1131-58.
- Meyers SP. MRI of Bone and Soft Tissue Tumors and Tumor like Lesions, Differential Diagnosis and Atlas. Thieme Publishing Group, New York 2008.
- Ilaslan H, Sundaram M, Unni KK. Solid variant of aneurysmal bone cysts in long tubular bones: Giant cell reparative granuloma. AJR Am J Roentgenol 2003;180:1681-7.
Fulltext Views
1,448
PDF downloads
400





