Translate this page into:
Bilateral posterior shoulder dislocation secondary to seizure event
*Corresponding author: Omar F. Shatnawi, MD. Department of Emergency, International Medical Corps, Al-Zaatari Camp, Almafrag, Jordan. omarfshatnawi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ghabashneh MM, Jdeitawi LF, Khataybeh IM, Shatnawi ZF, Shdifat LH, Shatnawi OF. Bilateral posterior shoulder dislocation secondary to seizure event. J Musculoskelet Surg Res. 2024;8:71-4. doi: 10.25259/JMSR_161_2023
Abstract
This case report presents a rare bilateral posterior shoulder dislocation resulting from a seizure. Bilateral shoulder dislocations are uncommon, especially in a posterior direction. Diagnosing and managing posterior shoulder dislocation can be challenging due to the need for specialized imaging techniques and expertise. This report details a 34-year-old male patient with a remote history of epilepsy without any fits or attacks over the past 16 years. Following a seizure, he sustained bilateral posterior shoulder dislocation and other associated fractures. The patient underwent reduction under general anesthesia and was immobilized using an arm sling. The outcome was favorable, with the patient improving during the follow-up period. Bilateral shoulder dislocation is a rare injury that can be missed in clinical practice and needs expertise in diagnosis and management. A low threshold of suspicion should be kept, especially in cases of seizure or electrical shock.
Keywords
Bilateral
Dislocation
Epilepsy
Fracture
Greater tuberosity
Reduction
Shoulder
INTRODUCTION
Shoulder dislocation is a relatively common major joint dislocation with anterior dislocation being more prevalent. However, there are relatively few posterior shoulder dislocations accounting for <2–4% of all shoulder dislocations.[1] Bilateral posterior shoulder dislocation is rarer occurring in approximately 14.6% of posterior shoulder dislocation cases.[2] Diagnosing posterior shoulder dislocation can be challenging due to the complexity of the condition and the requirement for specialized examination techniques and imaging.[3] This case study provides a unique instance of bilateral posterior shoulder dislocation secondary to a seizure event involving a patient, who had been free of seizures for over 16 years. The purpose of sharing this case is to emphasize the significance of regular visits to a neurologist for patients with epilepsy. This patient experienced a seizure while driving underscoring the importance of clinicians maintaining a heightened awareness and consideration for such diagnoses in individuals with a history of seizures.
CASE REPORT
A 34-year-old male patient was received at the hospital following a car accident. The patient was driving when he experienced an abnormal jerky movement without a clear, provocative event resulting in the car crashing into a solid object. The patient had a history of epilepsy and had been treated with sodium valproate for over 10 years. However, the medication was discontinued at the age of 18, as the patient had been free of seizures for over five years. On arrival at the hospital, the patient complained of severe bilateral shoulder pain. Physical examination revealed muscle asymmetricity, scapular winging, bilateral shoulder tenderness, limited external rotation, and severe pain on attempting movement. In addition, a substantial movement of the humeral head, either forward or backward, within the glenoid fossa occurs when a force is exerted in the corresponding direction. The AP and lateral view radiographs showed bilateral posterior shoulder dislocation with right side non-displaced greater tuberosity fracture [Figure 1]. Additional imaging studies such as brain computed tomography (CT) and chest radiograph showed no abnormalities. Complete blood count, creatinine, blood urea nitrogen, electrolyte, and coagulation profile tests were performed, and all returned within the normal range.
The patient’s bilateral posterior shoulder dislocation was successfully corrected under general anesthesia. As advised by the neurologist, we initially opted for general anesthesia to facilitate the reduction process and minimize the risk of seizures. The reduction procedure involved applying axial traction to the adducted and flexed arm followed by internal rotation while maintaining the traction [Figure 2].
Following reduction, the patient’s shoulders were immobilized using arm slings. The patient was put in an arm sling stabilizer for three weeks and then started physiotherapy. The patient showed improvement with a good range of motion and experienced a good outcome. We have counseled the patient on the importance of maintaining a low threshold for recurrent dislocation according to his young age and seizure history. The patient was referred to the neurologist, and the decision was to restart the patient on levetiracetam in addition to other investigations and imaging studies.
DISCUSSION
Shoulder dislocation can be defined as the clinical laxity of the glenohumeral joint. The symptomatic laxity can be in the anterior, posterior, inferior or multiple directions. This leads to instability of the humerus head within the glenoid fossa.[4] Bilateral posterior shoulder dislocation is a rare and challenging clinical condition. It frequently affects middle-aged males and is often misdiagnosed due to its rarity.[1] By examining the association between this case and the existing literature, we aimed to enhance our understanding of this condition and improve treatment planning. The pathogenesis of bilateral posterior shoulder dislocation involves muscle contractions that are involuntary and intense, particularly the internal rotators and adductors overpowering the external rotators and abductors.[5] An imbalanced contraction for a long time results in tension, which prompts excessive internal rotation and adduction at the shoulder joint’s level leading to posterior dislocation. This mechanism aligns with the findings reported by Shaw in 1971, who described the typical position of the shoulder joint during a seizure as flexion, adduction, and internal rotation.[6] In this position, excessive and unbalanced muscle contraction overwhelms the glenoid cavity. It forces the humeral head out leading to posterior and superior displacement. Prolonged pressure against the glenoid rim can result in complex proximal humeral fractures.[5] Epilepsy is the leading cause of bilateral posterior dislocations responsible for nearly 50% of such cases. However, uniqueness and concern arise when a patient, previously seizure free for over 16 years, suddenly experiences an attack. This underscores the importance of re-evaluating the duration and appropriate management of epilepsy-related conditions. Other rare causes such as electric shocks, extreme trauma, osteoporosis, stroke, and hypoglycemic episodes have also been reported in the literature.[2] Considering these rare causes, conducting a thorough clinical examination is crucial to avoid missed diagnoses and ensure appropriate treatment planning. Clinical manifestations of bilateral posterior shoulder dislocation typically include extreme discomfort, shoulder joint deformity, and limited external rotation. Diagnostic features include a rotational deformity with locked internal rotation, lost shoulder contour, increasing coracoid prominence, and humeral head protuberance that can be felt at the back of the shoulder.[6]
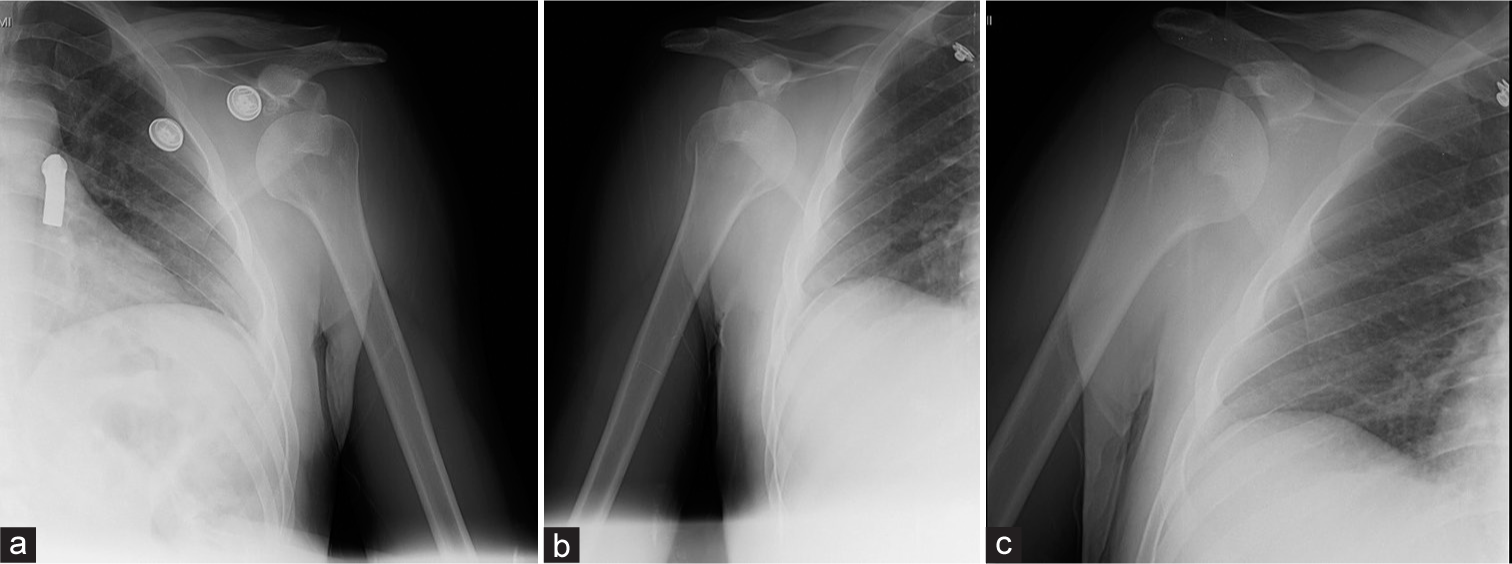
- (a-c) Pre-operative: AP and lateral view radiographs show bilateral posterior shoulder dislocation and right side non-displaced greater tuberosity fracture.
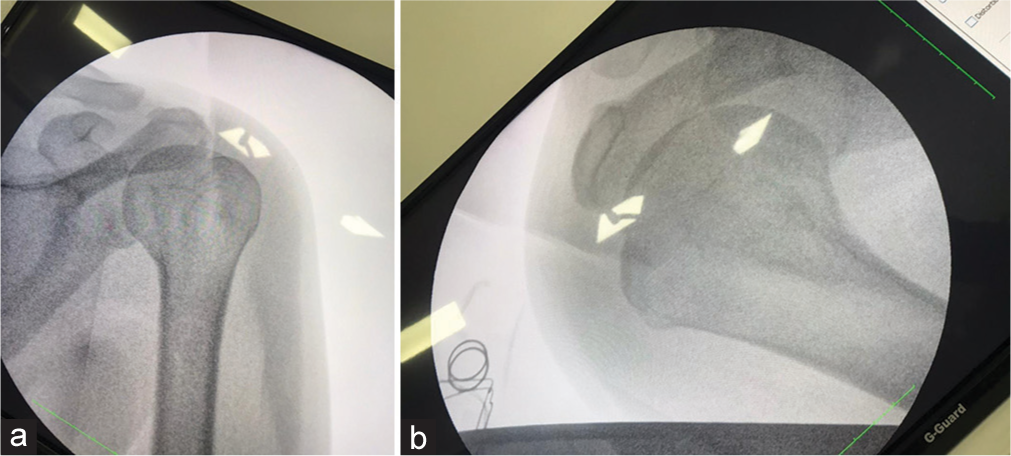
- (a and b) Post-operative: After the reduction procedure, the humerus head was back in the glenoid fossa, which involved applying axial traction to the adducted and flexed arm, followed by internal rotation while maintaining the traction.
Radiologic examinations play a vital role in confirming the diagnosis of bilateral shoulder dislocation. Anteroposterior radiographs can show only a few uncommon aberrant symptoms such as the light bulb or double shadow line sign or they can appear normal. Axillary views are essential for accurate diagnosis. However, pain and limited external rotation can make it challenging to obtain axillary views in acute situations. Apart from technical challenges, we encountered limitations such as the unavailability of an x-ray device supporting these specific views and a need for more expertise among radiology technicians in performing these particular views.[3] Under these circumstances, altered axillary perspectives such as the Velpeau or Wallace view can be helpful. The CT scans provide detailed information about fractures and about the relationship between the humeral head and glenoid making them valuable for treatment planning.[3]
The effective management of bilateral posterior shoulder dislocation requires the expertise of a skilled physician and is contingent on various factors. These factors encompass the extent of the humeral head defect, the duration of dislocation, the patient’s age, occupation, physical condition, and preferences.[7] Patients who present with unstable vital signs or substantial bony fractures are considered contraindicated for immediate reduction in an emergency setting. The presence of infection or open wounds further adds to the list of contraindications.[7,8]
Treatment options range from closed or open reduction to surgical interventions such as hemiarthroplasty or total shoulder arthroplasty. Open reduction with internal fixation is frequently required in scenarios where associated fractures are present, when closed reduction attempts fail or in cases of irreducible dislocations often due to anatomical obstacles or significant tissue entanglement. Furthermore, this approach may be deemed necessary for recurrent dislocations, substantial humeral head defects, and instances of neurovascular compromise. It is crucial to emphasize that the tailored treatment plans should consider these critical factors.[9]
Rehabilitation and physiotherapy are pivotal components in the management of shoulder dislocation. Typically, it is advised to restrict shoulder movement for the initial three weeks following reduction, often achieved by utilizing an immobilizer. During this period, gentle Codman exercises involving subtle shoulder movements with the arm suspended are encouraged. In the subsequent weeks, a progressive approach to a range of motion exercises is recommended, both actively and with assistance. It is crucial to avoid engaging in active exercises before the 12-week mark and consider returning to active sports no earlier than 16 weeks post-reduction, gradually increasing activity as tolerated.[10]
The management of shoulder dislocation should extend beyond just emergency situations. Patients should also receive counseling regarding the significant risk of recurrent dislocation episodes. Existing literature highlights various factors that influence the likelihood of recurrence with age and treatment type ranking at the top.[11] A younger age at the time of dislocation is associated with a markedly higher recurrence risk. For instance, patients under the age of 20 face a recurrence risk ranging from 72% to 100% while those aged 50 and above experience a significantly lower risk of only 10–22%.[12] In terms of treatment, one study demonstrated that repairing the labrum reduces the risk of future dislocation by an impressive 85% compared to a 47% risk among patients treated conservatively.[13] Apart from the risk of recurrence, there is the possibility of neurovascular injuries such as axillary nerve damage, rotator cuff tears, and fractures. Furthermore, it may lead to long-lasting problems such as joint stiffness and the onset of osteoarthritis.[8]
CONCLUSION
In this particular case, we highlight an instance of bilateral posterior dislocation, a frequently missed condition. Our aim in presenting this case is to increase awareness and maintain a low threshold for diagnosis. This includes emphasizing the need for radiological training in identifying bilateral dislocations and collecting comprehensive medical histories correlating with suspected injuries.
AUTHOR’S CONTRIBUTIONS
MMG and OFS were responsible for designing the study protocol. Updating reference lists and writing the manuscript draft. LFJ, IAK, ZFS, and LHS contributed to reviewing and proofreading the final manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
Institutional Review Board approval was waived.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patient’s consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Bilateral posterior shoulder dislocations. Am J Emerg Med. 1995;13:331-2.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of associated injury in posterior shoulder dislocation: Systematic review of the literature. J Orthop Trauma. 2012;26:246-51.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral posterior shoulder dislocation: The importance of the axillary radiographic view. Eur J Emerg Med. 2001;8:161-3.
- [CrossRef] [PubMed] [Google Scholar]
- Multidirectional instability of the shoulder. UpToDate Available from: https://www.uptodate.com/contents/multidirectional-instability-of-the-shoulder?search=biliteralposteriorshoulderdislocationdefinition&source=search_result&selectedtitle=1~150&usage_type=default&display_rank=1 [Last accessed on 2023 Oct 04]
- [Google Scholar]
- Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg. 2002;11:339-44.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J Bone Joint Surg Am. 1971;53:1437-40.
- [CrossRef] [PubMed] [Google Scholar]
- Sports trauma In: A case-based approach to shoulder pain a pocket guide to patholology diagnosis and management. Cham: Springer; 2022. p. :87-105.
- [CrossRef] [Google Scholar]
- Shoulder dislocation and reduction. UpToDate Available from: https://www.uptodate.com/contents/shoulder-dislocation-and-reduction?search=biliteralposteriorshoulderdislocationcomplication§ionrank=1&usage_type=default&anchor=h22&source=machinelearning&selectedtitle=1~150&display_rank=1#h22 [Last accessed on 2023 Oct 04]
- [Google Scholar]
- Posterior shoulder dislocation associated with fracture of the humeral anatomic neck: Treatment guidelines and long-term outcome. J Trauma. 1999;46:318-23.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: Long-term evaluation. Arthroscopy. 2005;21:55-63.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment and management of shoulder dislocation. BMJ. 2020;371:m4485.
- [CrossRef] [PubMed] [Google Scholar]
- What are the risks of a second shoulder dislocation-Dr. Bill Sterett. Available from: https://drsterett.com/sports-medicine-blog/second-shoulder-dislocation [Last accessed on 2023 Oct 04]
- [Google Scholar]
- Treatment after traumatic shoulder dislocation: A systematic review with a network meta-analysis. Br J Sports Med. 2018;52:1498-506.
- [CrossRef] [PubMed] [Google Scholar]






