Translate this page into:
Birth-related distal humerus epiphyseal separation: Outcome following surgical management
2 King Saud University, College of Medicine and King Khalid University Hospital, Riyadh, Saudi Arabia
Corresponding Author:
Bander S Alrashedan
Department of Orthopedic Surgery, Ministry of Health, King Saud Medical City, Ulaishah, 7790 Al Imam Abdul Aziz Ibn Muhammad Ibn Saud, Riyadh 12746 3617
Saudi Arabia
b.alrashedan@gmail.com
| How to cite this article: Aldossari AM, Alsagr GA, Alotaibi RA, Shogair MM, Alharbi H, Alrashedan BS. Birth-related distal humerus epiphyseal separation: Outcome following surgical management. J Musculoskelet Surg Res 2020;4:232-235 |
Abstract
Distal humerus epiphyseal separation is a rare entity that can present as a birth-related injury. It commonly presents in children younger than 2 years of age and can be a result of a fall or forceful manipulation during delivery. It commonly presents with elbow swelling and decreased movement in newborns. It can be misinterpreted as elbow dislocations due to the lack of ossification in the distal part of the humerus on plain radiographs. Several treatment approaches have been reported in the literature including surgical and nonsurgical treatment modalities. We present a 2-day-old girl with a right distal humerus epiphyseal separation following spontaneous vaginal delivery. An anatomical and a stable reduction of the fracture was the aim in the management of this injury and was achieved using an arthrogram-assisted closed reduction and a single percutaneous Kirschner wire fixation. The patient was followed for 12 months and showed a satisfactory outcome.
Introduction
The incidence of birth-related injuries in the ultrasound (US) was 2.45/1000 live births.[1] Among 34,946 live-born babies, clavicle fractures were found to be the most common among other bones involved (45.7%), followed by the humerus (20%) and femur (14.3%) with bone injuries found in one of every 1000 live births.[2] Birth-related humerus fractures were found in 0.09/1000 births, and the distal part of the humerus was involved less commonly than the proximal and diaphyseal parts.[3] Distal humerus epiphyseal separation is a relatively rare entity among other elbow injuries and is usually seen in children younger than 2 years of age.[4] It is the fourth (10%) after distal radius (28%), phalanges (15%), and distal tibia (13.5%) among epiphyseal separation fractures.[5] They can present following a fall or due to a forceful manipulation of the limb during labor.[4] They tend to present with elbow swelling and decreased movement. Some cases are missed on the 1st day of the injury in newborns and can be misinterpreted as elbow dislocations due to the lack of ossification in the distal part of the humerus on plain radiographs.[4],[6],[7] The diagnosis of distal humerus epiphyseal separation must be suspected in cases when the ulno-humeral and radiocapitellar articulations are disrupted on plain radiographs.[6],[7] Elbow dislocations in young children are rare as the cartilaginous physis is weaker than the bone-ligament interface.[6],[7] US and magnetic resonance imaging (MRI) have been used in the diagnosis of such injuries due to immature osseous anatomy that cannot ideally be evaluated on plain radiographs.[3],[4],[6] Careful and prompt diagnosis and treatment of these injuries must be taken to prevent malunion, which is commonly varus deformity and the subsequent need for aggressive surgical treatment.[7],[8] Cubitus varus deformity was found to be a common complication following both surgical (open or closed reduction and internal fixation) and nonsurgical treatment for these injuries and is commonly mild and nonprogressive.[4],[9],[10] Anatomical reduction in these injuries is important to prevent cubitus varus deformity and residual displacement.[4],[10] Since there is controversy regarding the treatment of choice of distal humerus epiphyseal separation in the literature, we present a rare case of a 2-day-old female with a right distal humerus epiphyseal separation treated with an arthrogram-assisted closed reduction and a single Kirschner wire (K-wire) fixation, who is followed for 12 months and showed a satisfactory outcome.
Case Report
A 2-day-old baby girl born at full term (39 weeks) by an uncomplicated spontaneous vaginal delivery to a primigravida mother with cephalic presentation. The mother's pregnancy course was uncomplicated with no pre- and peri-natal abnormalities detected on follow-up. The neonate's weight was 3.5 kg with an acceptable Apgar score on delivery and no apparent dysmorphic features. The patient had an unremarkable family history of chronic or congenital diseases. On the 2nd day after birth, the neonatologist noticed that the baby had swelling in the right elbow with decreased movement compared to the left side. Therefore, she was referred to orthopedic surgery staff on duty after obtaining plain radiographs, which were interpreted as an elbow dislocation by the neonatologist. Upon examination, the right elbow was noticed to have a diffuse swelling with a varus deformity and no associated ecchymosis. There was no active spontaneous movement at the elbow, but some spontaneous movements at the right shoulder, wrist, and hand were observed. Radial pulse was intact, and passive movement of the right upper limb caused crying. Skin temperature was comparable with the other limb, and systemic examination was unremarkable. Infection workup was ordered to rule out a septic joint and/or osteomyelitis and was negative.
Radiographs of the right elbow showed soft-tissue swelling and posteromedial displacement of the right ulna and radius in relation to the humerus [Figure - 1].
 |
| Figure 1: Preoprerative image: anteroposterior radiograph of right elbow showed posterior-medial displacement of the right forearm in relation to the humerus |
The child's age and the findings seen on radiographs made distal humerus epiphyseal separation the likely diagnosis. After discussion with the parents regarding the diagnosis, management, and possible complications, the family agreed for operative intervention with closed or open reduction and K-wire fixation under general anesthesia with the use of arthrogram. On the next day, the patient underwent the planned surgical intervention. She was placed on a radiolucent table under general anesthesia, and upon the first trial of closed reduction, an anatomic reduction was attained and was confirmed with an arthrogram. The dye was injected through posterior olecranon fossa using a 20-gauge needle (iohexol 300 mg/mL), diluted 1:1 with normal saline utilizing a very minimal amount under radiographic guidance. Fixation was achieved using a single laterally placed bicortical percutaneous K-wire size 1.6 mm. The K-wire was placed in the center of the nonossified capitellum aiming cranially to the medial cortex of the distal humerus. The fracture was found to be stable, and the reduction was maintained on elbow flexion and extension and forearm rotation under fluoroscopy, which made us decide not to use another K-wire [Figure - 2].
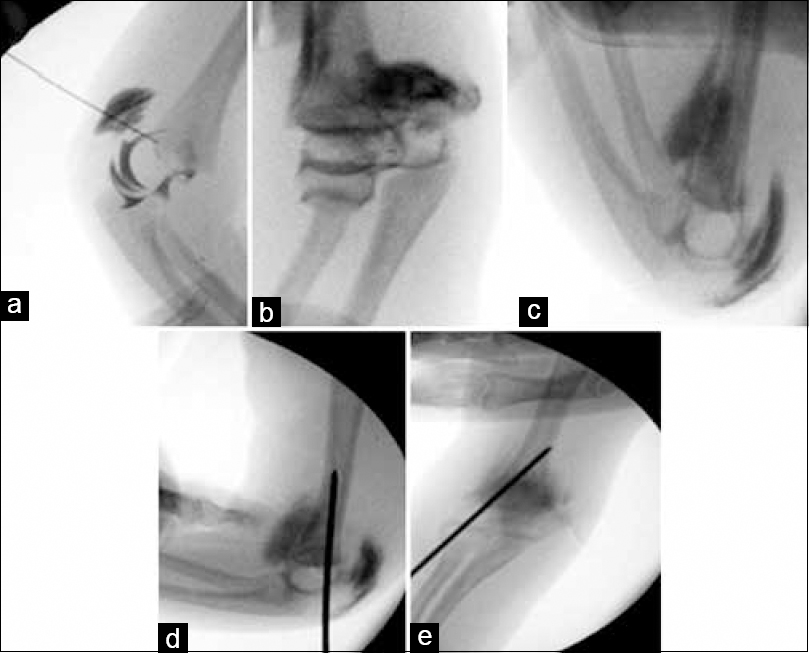 |
| Figure 2: Intraoperative images: anteroposterior (b, c, and e) and lateral views (a and d) with arthrogram injected to the right elbow joint under GA. With (a and b) prereduction films showing displacement of the distal humeral epiphysis. Closed reduction was done as seen in (c). In (d and e), a bicortical K-wire was introduced through lateral humeral condyle to maintain the reduction |
An above elbow backslap was applied, and the child was seen in the later day and examination was unremarkable, so she was discharged home.
She was seen in the outpatient department 3 weeks after the intervention with an intact distal neurovascular examination. Plain radiographs showed proper implant position, good alignment, and apparent callus formed at the fracture site. The K-wire was removed, and the elbow had a full range of passive motion with a carrying angle comparable to the uninjured side, which was around 10° of valgus [Figure - 3].
 |
| Figure 3: Radiographs taken 3 weeks postoperatively at the outpatient clinics. Anteroposterior (a) and lateral (b) views of radiographs of the right elbow, showing an acceptable alignment immediately following the K-wire removal |
She was seen after 3, 8, and 12 months from surgical intervention, and the child had a full painless symmetrical to the other side range of motion with no deformity, and milestones were proper to her age. A plain radiograph of the limb was obtained at the last follow-up and was satisfactory [Figure - 4].
 |
| Figure 4: Anteroposterior (a) and lateral (b) radiographs of the elbow joint taken 12 months postoperative treatment showing capitellum ossification |
Discussion
Birth-related distal humerus epiphyseal separation is an uncommon entity encountered by pediatric–orthopedic surgeons.[3],[4] Diagnosing such injuries can be challenging at the time of neonatal examination immediately following delivery since, in this age group, localization of pain or discomfort is difficult.[6] Difficult or instrumented deliveries have been reported as risk factors for distal humerus epiphyseal separation, and such cases have been seen following both vaginal delivery and cesarean section.[4],[6],[11] Most of the cases in one study presented with complicated vaginal deliveries.[4] In the same study, the main presenting sign in delayed diagnosis cases was decreased movement of the affected limb, as was seen in our patient.[4] Another study has found that all cases were delivered with a cesarean section.[6] Fortunately, the diagnosis in our case was on the 2nd day of life. The delivery was not complicated, and no instrumentation was used. Diagnosing these cases using plain radiographs is difficult due to the immature bone anatomy.[6] For this reason, the US, arthrogram, and MRI have been described in evaluating such injuries.[6] Kay etal. have found that three of the four cases included in their study initially diagnosed as elbow dislocation based on plain radiographs and were further investigated with US, MRI, or arthrogram.[6] We elected to do an arthrogram under general anesthesia due to the high likelihood of needing surgical treatment as it can be used as a diagnostic tool and an adjunctive modality for an accurate reduction. Care must be taken when injecting the contrast in the joint as injecting it into the soft tissue might distort the quality of the images making the procedure more difficult.[6] Zhou et al. found that the functional outcome was generally good regardless of the surgical procedure chosen for the treatment of these injuries.[6] Surgical treatment of this case is chosen to provide an accurate reduction. Varus malunion has been commonly reported secondary to an inadequate reduction, with variable prevalence following all treatment modalities.[10],[12],[13],[14] Avascular necrosis (AVN) of the medial condyle of the humerus can result in cubitus varus deformity following open surgical treatment.[15] Cubitus varus deformity has also been found due to distal humerus growth plate arrest.[16] For this reason, we used a single K-wire as it was sufficient to hold the reduction, avoiding the use of another one that can possibly cause trauma to the growth plate. Tharakan etal. reported a similar case to ours in terms of the age at presentation and treatment, and they recommended the use of US for the diagnosis and arthrogram-assisted closed reduction and K-wire fixation with a good outcome.[14] The difference in our case is that, instead of using two 0.9 mm K-wires, we used a single 1.6 mm bicortical K-wire, which made the reduction stable intraoperatively on flexion and extension of the elbow and rotation of the forearm. Gigante et al. reported five newborns with distal humerus epiphyseal separation in their series with all initially treated conservatively with closed reduction and immobilization.[17] Only one case needed closed reduction and pinning due to loss of reduction on follow-up in their study.[17] They highlighted the importance of the US in diagnosing these cases and the remodeling protentional in this age group making closed reduction and immobilization as a good treatment option as suggested by other studies.[3],[17],[18] Surgical and nonsurgical treatment of these injuries has been reported in the literature with good outcomes.[10] Varus deformity is believed to be caused by inadequate reduction in the absence of AVN of the medial humerus condyle.[10],[12] For this reason, surgical treatment under general anesthesia was chosen to ensure an accurate and stable reduction with the use of a K-wire fixation. Supakul et al. have found that 5 out of 16 patients (31%) had residual displacement on follow-up and were all treated nonsurgically with immobilization, while the patients who were treated surgically had no residual displacement.[4] They suggested that nonoperative treatment with casting in cases with mild displacement is acceptable as the outcome is generally good.[4] Rui-Lan et al. reported a preterm newborn with a distal humerus epiphyseal separation following cesarean section treated at the 10th day of life. They managed their case with an open reduction and two crossing percutaneous K-wires (each sized 1.0 mm) fixation due to the difficulty of accurately reducing the fracture by a closed mean.[9] Medial and lateral K-wire fixation (crossing) of supracondylar humerus fractures in pediatrics has an advantage of increased torsional resistance compared with a laterally placed K-wires with an increased risk of ulnar nerve injury in the crossing technique.[19] We avoided placing a medial K-wire to avoid the risk of injuring the ulnar nerve, and we found that the lateral K-wire was sufficient to stabilize the fracture during elbow movement under fluoroscopy. To the best of our knowledge, a single lateral K-wire fixation in distal humerus epiphyseal separation has not been reported in literature. However, Kish and Hennrikus found that the use of a single lateral K-wire fixation in Wilkins type 2A fracture provided sufficient stability.[20] Although distal humerus epiphyseal separation is a rare entity as a traumatic birth injury, several cases have been reported in the literature but with different treatment and diagnosis approaches used. We are reporting this case as it is rare with the consideration of the treatment used with a satisfactory outcome.
Conclusion
Distal humerus epiphyseal separation can present as a birth trauma following vaginal delivery. A decrease in limb movement can be the only sign of this injury and prompt evaluation is necessary to avoid delay in diagnosis. Several treatment approaches have been reported in the literature. Arthrogram-assisted closed reduction and a single percutaneous lateral bicortical K-wire fixation with the goal of achieving a stable reduction showed a good outcome.
Ethical consideration
The authors certify that they have obtained all appropriate patient consent forms. In the form the parents have given their consent for their daughter images and other clinical information to be reported in the journal. The parents understand that their daughter's name and initials will not be published and due efforts will be made to conceal their daughter's identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contribution
AMA and BSA conceived the study. AMA, RAA, GAA, MMS, and HA collected, provided, and organized materials and data of the patient. BSA and AMA wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Moczygemba CK, Paramsothy P, Meikle S, Kourtis AP, Barfield WD, Kuklina E, et al. Route of delivery and neonatal birth trauma. Am J Obstet Gynecol 2010;202:361.e1-6. [Google Scholar] |
| 2. | Bhat BV, Kumar A, Oumachigui A. Bone injuries during delivery. Indian J Pediatr 1994;61:401-5. [Google Scholar] |
| 3. | Sherr-Lurie N, Bialik GM, Ganel A, Schindler A, Givon U. Fractures of the humerus in the neonatal period. Isr Med Assoc J 2011;13:363-5. [Google Scholar] |
| 4. | Supakul N, Hicks RA, Caltoum CB, Karmazyn B. Distal humeral epiphyseal separation in young children: An often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR Am J Roentgenol 2015;204:W192-8. [Google Scholar] |
| 5. | Peterson HA. Physeal injuries of the distal humerus. Orthopedics 1992;15:799-808. [Google Scholar] |
| 6. | Kay M, Simpkins C, Shipman P, Whitewood C. Diagnosing neonatal transphyseal fractures of the distal humerus. J Med Imaging Radiat Oncol 2017;61:494-9. [Google Scholar] |
| 7. | Abzug J, Ho CA, Ritzman TF, Brighton B. Transphyseal distal humerus fracture. Instr Course Lect 2016;65:379-84. [Google Scholar] |
| 8. | Oh CW, Park BC, Ihn JC, Kyung HS. Fracture separation of the distal humeral epiphysis in children younger than three years old. J Pediatr Orthop 2000;20:173-6. [Google Scholar] |
| 9. | Rui-Lan L, Zhen-Jiang L, Li-Jun Z. Neonatal distal humeral physeal separation during caesarean section: A case report and review of a literature. Int J Clin Exp Med 2016;9:6882-9. [Google Scholar] |
| 10. | Zhou W, Canavese F, Zhang L, Li L. Functional outcome of the elbow in toddlers with transphyseal fracture of the distal humerus treated surgically. J Child Orthop 2019;13:47-56. [Google Scholar] |
| 11. | Malik S, Khopkar SR, Korday CS, Jadhav SS, Bhaskar AR. Transphyseal injury of distal humerus: A commonly missed diagnosis in neonates. J Clin Diagn Res 2015;9:SD01-2. [Google Scholar] |
| 12. | de Jager LT, Hoffman EB. Fracture-separation of the distal humeral epiphysis. J Bone Joint Surg Br 1991;73:143-6. [Google Scholar] |
| 13. | DeLee JC, Wilkins KE, Rogers LF, Rockwood CA. Fracture-separation of the distal humeral epiphysis. J Bone Joint Surg Am 1980;62:46-51. [Google Scholar] |
| 14. | Tharakan SJ, Lee RJ, White AM, Lawrence JT. Distal humeral epiphyseal separation in a newborn. Orthopedics 2016;39:e764-7. [Google Scholar] |
| 15. | Yoo CI, Suh JT, Suh KT, Kim YJ, Kim HT, Kim YH. Avascular necrosis after fracture-separation of the distal end of the humerus in children. Orthopedics 1992;15:959-63. [Google Scholar] |
| 16. | Abe M, Ishizu T, Nagaoka T, Onomura T. Epiphyseal separation of the distal end of the humeral epiphysis: A follow-up note. J Pediatr Orthop 1995;15:426-34. [Google Scholar] |
| 17. | Gigante C, Kini SG, Origo C, Volpin A. Transphyseal separation of the distal humerus in newborns. Chin J Traumatol 2017;20:183-6. [Google Scholar] |
| 18. | Catena N, Sénès FM. Obstetrical chondro-epiphyseal separation of the distal humerus: A case report and review of literature. J Perinat Med 2009;37:418-9. [Google Scholar] |
| 19. | Lee SS, Mahar AT, Miesen D, Newton PO. Displaced paediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop 2002;22:440-3. [Google Scholar] |
| 20. | Kish AJ, Hennrikus WL. Fixation of type 2a supracondylar humerus fractures in children with a single pin. J Pediatr Orthop 2014;34:e54-7. [Google Scholar] |
Fulltext Views
4,016
PDF downloads
1,512





