Translate this page into:
Can clinical tests show high diagnostic accuracy in the assessment of degenerative full-thickness rotator cuff tears?
*Corresponding author: Aditi Pandey, Chelsea and Westminster Hospital, London, United Kingdom. aditi.pandey4@nhs.net
-
Received: ,
Accepted: ,
How to cite this article: Pandey A, Adla DN, Pandey R. Can clinical tests show high diagnostic accuracy in the assessment of degenerative full-thickness rotator cuff tears? J Musculoskelet Surg Res, 2023;7:157-63.
Abstract
Objectives:
At present, the diagnosis of full-thickness rotator cuff tears (FTCTs) relies heavily on imaging. We suggest that clinical examination can reliably be used as a substitute for diagnostic imaging, particularly in relatively older patients who are undergoing conservative management. Our study evaluated the diagnostic value of five clinical tests in assessing FTCT in secondary care.
Methods:
One hundred and fifteen patients were examined by a consultant shoulder surgeon for suspected FTCT and underwent diagnostic imaging. Clinical examination included the empty-can test, resisted external rotation test, external rotation lag test, belly-press test, and lift-off test. Fifty two (45%) of these patients were referred for shoulder arthroscopy, while the rest were managed conservatively. The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of these tests were calculated, comparing clinical results with arthroscopic findings.
Results:
Our results showed that, in combination, these five special tests have high diagnostic values for FTCT, with an overall accuracy of 90%. Both the empty-can test and the resisted external rotation test had a sensitivity of 97%. While the external rotation lag test had poor accuracy, it was 100% successful at ruling in tears. The belly-press and lift-off tests were 100% sensitive and specific for full-thickness tears of the subscapularis.
Conclusion:
Clinical tests for diagnosing FTCT have high diagnostic value, comparable to imaging modalities explored in the literature. Overreliance on magnetic resonance imaging and ultrasonography may not be justified, particularly in a relatively older population when a rotator cuff tear repair is not scheduled.
Keywords
Arthroscopy
Clinical test
Predictive value
Rotator cuff
Rotator cuff injuries
Shoulder
INTRODUCTION
Rotator cuff disease is one of the four most common causes of shoulder pain in the community.[1] The correct diagnosis of full-thickness rotator cuff tears (FTCTs) would ensure prompt management of this condition, improving outcomes and reducing disability.[2] A comprehensive physical examination is essential as rotator cuff tears are difficult to diagnose based on history-taking alone.[3]
Special clinical tests have been developed to examine each component of the rotator cuff specifically.[3] Hermans et al. describe over 25 physical examination maneuvers, which have all been endorsed for this task. However, there is a sparsity of high-quality primary studies evaluating the diagnostic accuracy of these specific clinical examinations.[4] Systematic reviews comment on the heterogeneity of these primary studies, leading to difficulty in conducting a meta-analysis of the data.[5] At present, BMJ’s Best Practice suggests that a combination of four physical tests should be used to assess the rotator cuff. These include the empty-can test, the resisted external rotation test, the lift-off test, and the belly-press test.[6] Literature also suggests that the external rotation lag test is useful in assessing the rotator cuff.[7]
In light of this controversy, the current management approaches rely heavily on imaging, with magnetic resonance imaging (MRI) and ultrasonography becoming almost mandatory in diagnosing rotator cuff tears.[8] The use of diagnostic imaging may also be increasing because of the practice of defensive medicine and other medicolegal reasons.[9] Imaging requirements now form part of the rotator cuff repair criteria in medical coverage firms in North America.[10] Subsequently, reliance on clinical examination is decreasing. This is despite resources being wasted organizing imaging to assess rotator cuff tears even when no surgical management is planned.
We hypothesize that a thorough clinical examination is an accurate diagnostic tool for FTCT when it is carried out by an experienced orthopedic surgeon. Thus, heavy dependence on MRI and ultrasonography may not be justified, particularly when surgical repair is not scheduled. Primarily, we aimed to evaluate the diagnostic value of clinical examination for FTCT compared to arthroscopy. We also analyzed the data of patients who had FTCT but did not have an arthroscopy.
MATERIALS AND METHODS
This study retrospectively reviewed prospectively collected data from 2010 to 2013. It was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice.
Patient selection
One hundred and forty-one patients were referred by their general practitioners (GPs) to a tertiary shoulder unit with suspected rotator cuff pathology. Patients with a history of trauma to the concerned shoulder were excluded, including acute rotator cuff tears. This is because pain may have prevented a thorough physical examination. Other exclusion criteria included bilateral shoulder pain, previous surgery to the same shoulder, glenohumeral arthritis, shoulder instability, frozen shoulder, or a previous cuff tear diagnosed by ultrasonography or MRI. After these criteria were applied, 115 patients were included in our analysis.
Clinical examination
All patients were examined by a single fellowship-trained consultant shoulder specialist. These patients were clinically examined for FTCT using five tests: The empty-can test; the resisted external rotation test, the external rotation lag test for supraspinatus, infraspinatus, and teres minor tears;[7,11,12] the belly-press test; and the lift-off test for subscapularis tears.[7,13] Each test was recorded as positive or negative for FTCT. The tests were regarded as positive if weakness or weakness was associated with pain compared to the other shoulder. In accordance with the literature, pain alone was not taken as a positive test.[14] The test was first performed on the unaffected shoulder, followed by the affected shoulder.
Empty-can test
The shoulder was elevated to 90° in the scapula plane with the elbow fully extended and the shoulder internally rotated with the thumb pointing downward. The patient resisted a downward force on the distal forearm by the examiner.[6,7]
Resisted external rotation test
The patient’s arm was positioned by their side with the elbow flexed to 90°. The patient’s attempt at external rotation was resisted by the examiner.[6]
External rotation lag test
The patient’s arm was positioned by their side with the elbow flexed to 90°. The examiner moved the patient’s shoulder to the location of maximal external rotation passively. The patient was then asked to hold that position.[7]
Belly-press test
The patient was told to press the palmar surface of their hands on their abdomen and instructed to bring their elbows in front of their abdomen, keeping the arm in maximal internal rotation. The examiner applied gentle pressure on the elbows from the front.[6,7]
Lift-off test
The patient was instructed to put the dorsal surface of the hand on the ipsilateral buttock and then lift the hand off the buttock by a few inches. The examiner applied resistance to the hand from behind.[6,7]
All 115 patients had a radiograph following clinical examination, followed by an MRI (75 patients) or ultrasound scan (40 patients). After undergoing clinical examination and investigations, 52 patients required arthroscopic shoulder surgery. These patients had the five clinical tests repeated on the morning of their surgery. The rotator cuff findings on clinical examination were then compared with arthroscopic findings. The 63 patients who did not undergo arthroscopy formed the non-arthroscopy cohort. The rotator cuff findings on clinical examination were then compared with the diagnostic imaging results.
Shoulder arthroscopy
All shoulder arthroscopies were performed under general anesthesia and an interscalene block in a lateral position with traction by the consultant surgeon or under his supervision. The rotator cuff was thoroughly inspected and findings were recorded. An FTCT was diagnosed when a hole or defect in a part of a tendon insertion communicated through to the subacromial space. The subacromial space was then assessed for confirmation of the FTCT.
Statistical analysis
The data analysis included calculating sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy. These values were determined using a two by two table.[12,15] In our investigation, only FTCT was considered positive. Since both input and output variables were categorical variables, we chose Fisher’s exact test to complete the statistical analysis.[16-18] Our findings were regarded as statistically significant for P < 0.05. The prevalence of FTCT in our secondary care setting was between 50% and 60%. The required sample size for sensitivity analysis was 52, and the required sample size for specificity analysis was 38.[19]
RESULTS
The selection procedure for our patient sample is displayed in [Figure 1]. One hundred and forty-one patients were referred by their GP to a tertiary shoulder unit with suspected rotator cuff pathology. After the exclusion criteria were applied, 115 patients entered the study. Of the 52 patients requiring arthroscopic surgery, 33 (63%) had full-thickness tears, while 19 (37%) did not. However, on clinical examination, 36 (69%) patients were thought to have FTCT, indicating that there were three falsely positive clinical examinations in this cohort. Patient demographics are displayed in [Table 1]. The non-arthroscopy cohort had an older age range, reflecting clinical practice to refer younger patients for shoulder surgery while managing older patients conservatively.
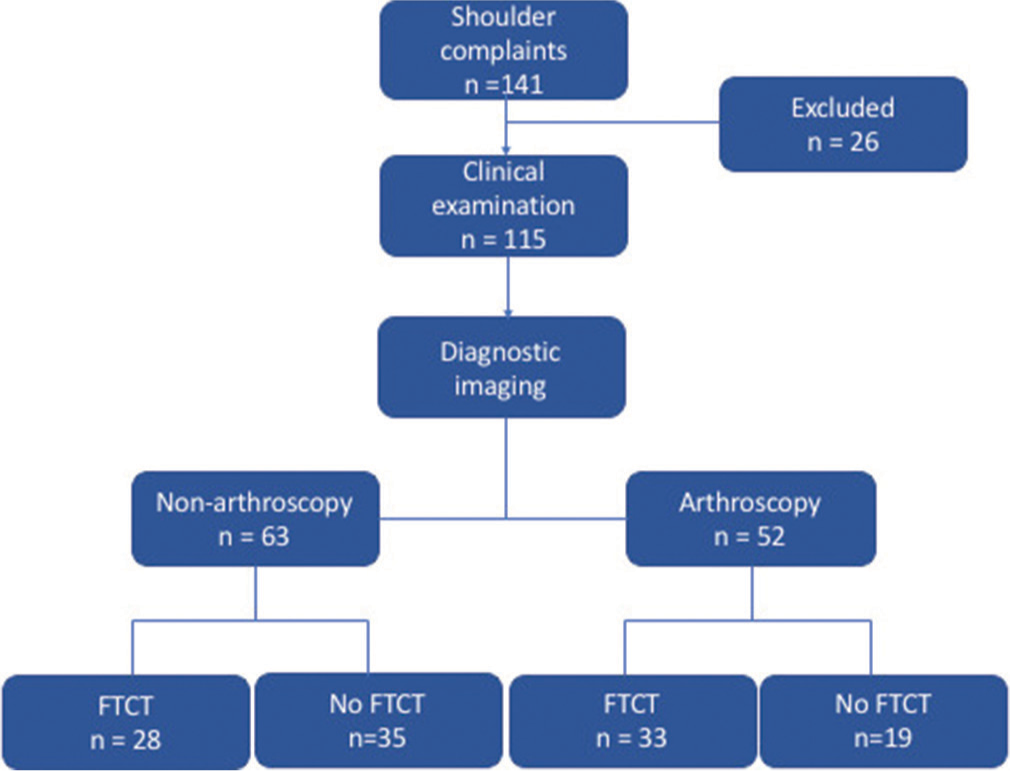
- Diagram demonstrating the selection procedure of our study. n: The number of patients assessed at each stage.
| Arthroscopy cohort | Non-arthroscopy cohort | |
|---|---|---|
| Number of patients | 52 | 63 |
| Age range (years) | 40–68 (Mean=51) | 62–79 (Mean=68) |
| Gender | 33 Males 19 Females | 39 Males 24 Females |
| Duration of symptoms (months) | 6–18 (Mean=9) | 6–24 (Mean=10) |
The results show that, as a whole, the clinical examination has statistically significant diagnostic value in the diagnosis of FTCT. Furthermore, with very high sensitivity and NPV, clinical examination was particularly successful at ruling-out FTCT in our sample population. Overall, the physical examination has a diagnostic accuracy of 90% [Table 2].
| Test | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | P value |
|---|---|---|---|---|---|---|
| Overall clinical examination | 0.97 | 0.79 | 0.89 | 0.94 | 0.90 | <0.00001 |
FTCT: Full-thickness rotator cuff tears. The P value was calculated using Fisher’s exact test comparing clinical test results to arthroscopic findings.
The diagnostic value of the five different clinical tests for FTCT is displayed in [Table 3]. The empty-can test, resisted external rotation test, and external rotation lag test assess the integrity of the supraspinatus, infraspinatus, and teres minor. The belly-press test and lift-off test assess the subscapularis. Both the resisted external rotation test and empty-can test were very accurate when ruling-out FTCT: They both have a sensitivity of 97%. However, the resisted external rotation test had a higher specificity and PPV than the empty-can test, indicating it was more capable of ruling-in tears. The external rotation lag test had the highest specificity of the three tests (100%). However, it had a sensitivity of 17% and poor diagnostic accuracy. A combination of tests had higher specificity (P < 0.0237) and PPV (P < 0.0121) than the empty-can test individually.
| Test | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | P value |
|---|---|---|---|---|---|---|
| Empty-can test | 0.97 | 0.83 | 0.86 | 0.95 | 0.90 | <0.00001 |
| Resisted external rotation test | 0.97 | 0.91 | 0.93 | 0.95 | 0.94 | <0.00001 |
| External rotation lag test | 0.17 | 1.00 | 1.00 | 0.49 | 0.54 | 0.0586 |
| Lift-off test | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | <0.00001 |
| Belly-press test | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | <0.00001 |
FTCT: Full-thickness rotator cuff tears. The reference standard was shoulder arthroscopy. The P value was calculated using Fisher’s exact test comparing clinical test results to arthroscopic findings
Our results show that full-thickness tears of the subscapularis are less common; only four (12%) out of the 33 FTCTs diagnosed on arthroscopy were tears of the subscapularis. However, all four patients with clinical full-thickness subscapularis tears were confirmed to have full-thickness subscapularis tears arthroscopically. In this respect, the belly-press and lift-off tests are highly accurate at screening for full-thickness subscapularis tears.
Of the 63 patients in the non-arthroscopy cohort, 28 (44%) had full-thickness tears, while 35 (56%) did not. However, on clinical examination, 25 (40%) patients were thought to have FTCT, indicating that there were three falsely negative clinical examinations in this cohort [Table 4].
| Test | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | P value |
|---|---|---|---|---|---|---|
| Overall clinical examination | 0.89 | 1.00 | 1.00 | 0.92 | 0.95 | <0.00001 |
Full-thickness rotator cuff tears. The P value was calculated using Fisher’s exact test comparing clinical examination findings to the results of diagnostic imaging
DISCUSSION
Our results show that clinical examination (using the combination of special tests described in our methods) is an accurate diagnostic tool for diagnosing FTCT compared to arthroscopy. Furthermore, this remained true in the non-arthroscopy cohort when our reference standard was diagnostic imaging.
As the current literature stands, there is little evidence recommending one special test over another in assessing rotator cuff disease. Key systematic reviews have worked to identify the most accurate individual clinical test, but variation in their methods alongside poor quality primary studies has prevented a consensus.[4,5,20-23] In agreement with our findings, the empty-can test, external rotation lag test, and belly-press test have been shown to have diagnostic utility by these systematic reviews.
Individually, our results show that the resisted external rotation test was the best test to use as a screening tool for FTCT. Alternatively, if any one of the external rotation lag test, belly-press test, or lift-off test was positive, we were likely to find a tear on arthroscopy. Although highly specific, the external rotation lag test showed poor sensitivity and NPV in our study. Notably, the five patients in the arthroscopic cohort with a positive external rotation lag test all had large cuff tears. Similarly, 11 patients with a positive external rotation lag test in the non-arthroscopic cohort all had large cuff tears on MRI. Therefore, it is possible that this test is particularly sensitive in detecting large to massive rotator cuff tears. As only four (12%) out of the 33 FTCTs diagnosed on arthroscopy were tears of the subscapularis, the belly-press and lift-off tests on their own may have limited utility as screening tools for FTCT due to the low incidence of subscapularis tears.[13]
While individual tests may fall short, our results show that a thorough clinical examination by an experienced orthopedic surgeon still provides a highly accurate diagnosis. Moreover, an experienced clinician is unlikely to rely on merely one maneuver to assess the shoulder. The diagnostic process involves amalgamating several clinical tests to arrive at a conclusion. Sgroi et al. demonstrated that diagnostic capability increased when three or more clinical tests were used to identify tears in the supraspinatus muscle. The authors went on to establish the same when two or more clinical tests were used to identify tears in the infraspinatus muscle.[11,12] In agreement with our findings, the literature demonstrates that combining multiple clinical tests improve their diagnostic value in assessing rotator cuff disease.[24,25]
A combination of three clinical features, weakness in abduction, weakness in external rotation, and impingement, had a PPV of 98% when predicting rotator cuff tears reported by Murrell and Walton.[26] Notably, patients had the same PPV if they had two out of three of these clinical features and were also over the age of 60 years.
The literature has limited exploration of the diagnostic value of patient information for rotator cuff tears. However, increasing age and night pain are examples of patient characteristics and history, which have significant diagnostic value in this condition.[15,27] In future research, evaluating the diagnostic accuracy of history-taking and physical examination in combination would be interesting.
Clinicians rely heavily on MRI and ultrasonography for the diagnosis of rotator cuff disease. However, there are disadvantages to this diagnostic approach. Due to the high prevalence of asymptomatic rotator cuff tears in the population, interpreting diagnostic imaging can be complex. This is particularly true in older patients; over 50% of asymptomatic individuals have rotator cuff tears on diagnostic imaging when they are over 65 years of age.[28] Furthermore, MRI is expensive and cannot be used in obese, claustrophobic patients, or patients with devices such as pacemakers. In comparison with MRI, ultrasonography is an inexpensive and convenient method of evaluating the shoulder. However, the type of ultrasound equipment as well as operator experience affect its accuracy in identifying tears.[29]
In light of these disadvantages, we suggest that elderly patients who are being scheduled for surgical rotator cuff repair should only have diagnostic imaging after failing conservative management. Patients with tears in the non-arthroscopic cohort were treated nonoperatively as they were relatively older than patients scheduled for arthroscopy [Table 1]. Nevertheless, regardless of the age difference, the clinical examination had a high overall diagnostic accuracy in both cohorts. Our results show that an accurate diagnosis for FTCT can be made clinically by a skilled orthopedic surgeon in secondary care. Therefore, organizing imaging to assess rotator cuff tears may not be justified, particularly when surgical repair is not scheduled. There were three falsely negative patients who displayed FTCT on imaging but not examination. However, these were small full-thickness tears in relatively older patients and were treated non-operatively, leading to asymptomatic patients.
Both MRI and ultrasonography have been shown to have similar levels of efficacy in identifying rotator cuff tears. A Cochrane review commented that MRI had an estimated sensitivity of 98% and specificity of 79%.[30] This is nearly identical to our results for the sensitivity and specificity of overall clinical examination, which were 97% and 79%, respectively. However, ultrasonography can have a sensitivity and specificity as low as 66% and 54%, respectively.[31]
Similar to clinical examination, both imaging modalities are poorer at identifying partial-thickness tears than full-thickness tears.[8,29] However, the majority of the time partial- thickness tears do not need surgical management. For these reasons, we aimed to diagnose only full-thickness tears on clinical examination.
Hanchard et al. expand on the merits of having sensitive and specific physical maneuvers for the diagnosis of musculoskeletal conditions.[5] They do not require additional time and resources to organize and they can be completed during routine secondary care consultation with an orthopedic consultant, yielding immediate results. Since they rely on reproducing symptoms, they will not superfluously detect asymptomatic tears. As one author eloquently says, “Respect must be shown for the physical exam.”[10]
Like primary studies, which have come before us, our methods have some key limitations. First, we acknowledge that the diagnostic value of a test transforms with changes in disease prevalence.[32] Since our sample size was highly selective, the prevalence of FTCT was likely higher than in the general population.[33] Second, our shoulder surgeon was not blinded to the results of the clinical tests, which may have led to bias when the arthroscopy was performed. However, the clinical examination was performed before arthroscopy, so the surgeon did not know the diagnosis when carrying out the clinical examination.
CONCLUSION
Clinical tests for the diagnosis of FTCT have high sensitivity and specificity, comparable to imaging modalities explored in the literature. Overreliance on MRI and ultrasonography may not be justified, particularly in a relatively older population when a rotator cuff tear repair is not scheduled.
AUTHORS’ CONTRIBUTIONS
AP and RP did the literature search, analyzed, and interpreted the data and wrote the manuscript. DNA and RP did the study design and collected and analyzed the data. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
ETHICAL APPROVAL
The study was conducted in accordance with the Declaration of Helsinki. No patient identifiable information is included. This study was a departmental audit so the ethical approval was waived by the local ethical committee.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Shoulder pain: Diagnosis and management in primary care. Br Med J. 2005;331:1124-8.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed repair of tendon to bone injuries leads to decreased biomechanical properties and bone loss. J Orthop Res. 2005;23:1441-7.
- [CrossRef] [PubMed] [Google Scholar]
- A review of the special tests associated with shoulder examination part I: The rotator cuff tests. Am J Sports Med. 2003;31:154-60.
- [CrossRef] [Google Scholar]
- Does this patient with shoulder pain have rotator cuff disease? The rational clinical examination systematic review. JAMA. 2013;310:837-47.
- [CrossRef] [PubMed] [Google Scholar]
- Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;2013:CD007427.
- [CrossRef] [Google Scholar]
- Rotator Cuff Injury - Symptoms. Diagnosis and Treatment. 2018. BMJ Best Practice. Available from: https://bestpractice.bmj.com/topics/en-gb/586 [Last accessed on 2020 Dec 28]
- [Google Scholar]
- Rotator cuff tear: Physical examination and conservative treatment. J Orthop Sci. 2013;18:197-204.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg. 2002;11:219-24.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic imaging practice guidelines for musculoskeletal complaints in adults-an evidence-based approach: Introduction. J Manipulative Physiol Ther. 2007;30:617-83.
- [CrossRef] [PubMed] [Google Scholar]
- Editorial commentary: Where's the respect? Physical exam of the shoulder. Arthroscopy. 2018;34:2334-6.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of clinical tests for infraspinatus tendon tears. Arthroscopy. 2019;35:1339-47.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic value of clinical tests for supraspinatus tendon tears. Arthroscopy. 2018;34:2326-33.
- [CrossRef] [PubMed] [Google Scholar]
- Subscapularis tendon tears. J Am Acad Orthop Surg. 2005;13:353-63.
- [CrossRef] [PubMed] [Google Scholar]
- Which is more useful the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27:65-8.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J Orthop Surg Res. 2014;9:70.
- [CrossRef] [PubMed] [Google Scholar]
- Study Design and Choosing a Statistical Test. 2019. United Kingdom: BMJ Publishing Group Ltd; Available from: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/13-study-design-and-choosing-statisti [Last accessed on 2021 Jan 01]
- [Google Scholar]
- How to choose the right statistical test. Indian J Ophthalmol. 2011;59:85-6.
- [CrossRef] [PubMed] [Google Scholar]
- Statistical Methods in Diagnostic Medicine. Hoboken NJ, USA: John Wiley and Sons, Inc.; 2011.
- [CrossRef] [Google Scholar]
- Requirements for minimum sample size for sensitivity and specificity analysis. J Clin Diagn Res. 2016;10:YE01.
- [CrossRef] [PubMed] [Google Scholar]
- Physical examination tests of the shoulder: A systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42:80-92.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of clinical tests for subacromial impingement syndrome: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2012;93:229-36.
- [CrossRef] [PubMed] [Google Scholar]
- Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46:964-78.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: A systematic review. Health Technol Assess. 2003;7:iii, 1-166
- [CrossRef] [Google Scholar]
- Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446-55.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90:1898-903.
- [CrossRef] [PubMed] [Google Scholar]
- Returning to the bedside: Using the history and physical examination to identify rotator cuff tears. J Am Geriatr Soc. 2000;48:1633-7.
- [CrossRef] [PubMed] [Google Scholar]
- The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-704.
- [CrossRef] [PubMed] [Google Scholar]
- Detection and quantification of rotator cuff tears: Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708-16.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;2013:CD009020.
- [CrossRef] [Google Scholar]
- Diagnostic ultrasound of the rotator cuff: Sensitivity and specificity in a district general hospital. Shoulder Elbow. 2012;4:22-4.
- [CrossRef] [Google Scholar]
- The development of QUADAS: A tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
- [CrossRef] [PubMed] [Google Scholar]
- User's guide to the surgical literature: How to use an article about a diagnostic test. J Bone Joint Surg Am. 2003;85:1133-40.
- [CrossRef] [PubMed] [Google Scholar]






