Translate this page into:
Comparison of musculoskeletal pain prevalence between medical and surgical specialty residents in a major hospital in Riyadh, Saudi Arabia
2 Department of Orthopedic Surgery, King Abdulaziz Medical City, National Guard Health Affairs, Riyadh, Saudi Arabia
Corresponding Author:
Salman Alahmed
College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh
Saudi Arabia
alahmed601@ksau-hs.edu.saAbdullah Alsultan
College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh
Saudi Arabia
alsultan086@ksau-hs.edu.sa
| How to cite this article: Alsultan A, Alahmed S, Alzahrani A, Alzahrani F, Masuadi E. Comparison of musculoskeletal pain prevalence between medical and surgical specialty residents in a major hospital in Riyadh, Saudi Arabia. J Musculoskelet Surg Res 2018;2:161-166 |
Abstract
Objectives: Musculoskeletal disorders are an occupational hazard between physicians. Physicians whose practice involves physical undertakings, such as surgeons, are prone to musculoskeletal pain, which can lead to decreased productivity. This study aimed to compare surgical and nonsurgical specialties musculoskeletal pain prevalence, as well as assess whether certain factors contribute to their pain. Methods: A cross-sectional study that utilized a self-administered questionnaire handed out to 140 conveniently selected surgical and nonsurgical residents at King Abdulaziz Medical City, Riyadh. The questionnaire included a demographics section and a section inquiring about nine anatomical areas derived from the Nordic Musculoskeletal Questionnaire. Results: The mean age was 27 years old, and 79% were male. Surgical residents comprised 39% (n = 55) of the participants. Of all the residents, 82.9% (n = 116) suffered from a musculoskeletal complaint, with the majority involving the lower back (53%). Surgical residents were more likely to take time off work (16% vs. 4%) and attributed their pain to their profession (38% vs. 15%). Lower back pain was related positively to body mass index (P = 0.04). Multivariate logistical regression revealed that being a surgeon (odds ratio [OR] = 5.08 and confidence interval [CI] = 0.27–94.14) and spending time doing interventional procedures (10 h; OR = 0.97 and CI = 0.05–18.61) are predisposing factors to musculoskeletal pain. Conclusion: Ergonomic changes are needed to enhance productivity and decrease time off work. Surgical residents need to be aware of the risk of experiencing musculoskeletal pain and be educated on ways to avoid or cope with their pain.
Introduction
Occupational risks are hazardous events encountered in the workplace. These may include chemical, biological, psychosocial, and physical hazards.[1] Musculoskeletal disorders a term defining complaints, symptoms, or pains to the musculoskeletal system, which can range from mild and intermittent to severe and chronic causing morbidity.[2],[3] To add, they are one of the most stressing issues faced by health-care workers, especially surgeons, that maintain a still posture for a prolonged time.[4],[5] A study conducted in 2011/2012 showed an estimated 1.1 million individuals suffered from occupational hazards with musculoskeletal disorders being the second most common cause of the following mental disorders.[6] Studies concerned with the epidemiology of musculoskeletal disorders in health-care providers showed that repetitive bending and twisting, manual handling, abnormal postures, and forceful movements are important predisposing factors to musculoskeletal disorders.[7],[8] A national cross-sectional study done in the United Kingdom by Babar-Craig et al. included 325 ear, nose, and throat physicians, 72% had back or neck pains or both inferring their pains to long microscopic work and bending forward while sitting.[9] Other risk factors, which were similar to general surgeons, included endoscopic procedures, frequent bending, and prolonged still postures.[10],[11] In comparison with medical specialties, a cross-sectional study was done in 2012 in India, which compared musculoskeletal pain prevalence in dentists, surgeons, and physicians. This study found that the highest rates of musculoskeletal pains were among dentists (61%), followed by surgeons (37%) and least in physicians (20%).[11] A study conducted by Auerbach et al. in 2011 revealed that spine surgeons scored higher levels of musculoskeletal pains (disk degenerative diseases and herniation, carpal tunnel syndrome, and lateral epicondylitis) when compared to the general public.[12]
Physical discomforts can be disregarded or ignored by physicians to provide optimum patient care. Physicians are susceptible to bending, twisting, lifting heavy loads, and maintaining an awkward posture for a long time, which is all considered risk factors for musculoskeletal pains.[7],[8],[13] The societal burden of injuries to physicians will be inflicted through their decreased productivity, absence from work, and cost of treatment.[14],[15],[16] In the United Kingdom, 116 million working days were lost from the general population due to musculoskeletal disorders (lower back pain) between 1994 and 1995.[17] In addition, Mollazadeh and Saraei found that of 690 medical personnel in Tehran teaching hospital during 290 working days between 2014 and 2015, 180 participants had sick leaves with a sickness absence rate of 0.011/year and an absence frequency rate of 0.68/year, 18% of them were related to the musculoskeletal system.[18]
In Saudi Arabia, multiple articles were found in the literature on the prevalence of musculoskeletal pains in different specialties of the health-care system. However, studies comparing the prevalence of musculoskeletal pains in surgical to nonsurgical medical specialties were not found. In addition, the literature review did not show any similar local studies. This study would serve as a benchmarking tool for addressing and reducing the physical stressors experienced by both surgical and nonsurgical physician. We aimed to see the differences in the rates of musculoskeletal disorders, between only surgical and nonsurgical residents at King Abdulaziz Medical City due to the fact that consultants were fewer in number to meet the sample size, easier accessibility to residents as opposed to consultants, and vast differences between different consultants ages in comparison to resident during their training. Our results stress the importance of creating an ergonomically safe work environment for surgical and nonsurgical health professionals.
Materials and Methods
Setting
This study was conducted in King Abdulaziz Medical City, a government-funded tertiary hospital in Riyadh, Saudi Arabia.
Sample
This study was a cross-sectional design that utilized a self-administered questionnaire, which was handed out at wards, resident lounges, and resident activity rooms to conveniently selected surgical and nonsurgical residents. The sample size was calculated using PiFace[19] and was determined to be 85 nonsurgical and 55 surgical residents to achieve a 5% level of significance and to achieve a power of 80% in detecting the difference of at least 15% between surgical and nonsurgical residents.
Instruments
The questionnaire, which was developed by Knudsen et al.,[20] has two main parts: demographics and symptoms sections. The cover page of the questionnaire was an informed consent. The demographics section inquired about age, gender, weight, height, residency level, average number of hours spent doing interventional procedures/operating/week, handedness, most commonly used eyewear, and most commonly employed operating/procedural position. The symptoms section included nine different anatomical areas derived from the Nordic Musculoskeletal Questionnaire (NMQ). These areas are as follows: neck, shoulders, elbows, wrists/hands, upper back, lower back, hips/thighs, knees, and ankles/feet. In case a participant answers negatively toward a certain area, the questionnaire asks to skip to the next area; however, in case of a positive response, the participant was asked further questions about interference with work over the last year, difficulties over the past week, and description of the pain's character (pain, stiffness, weakness, paresthesia, or others). Participants were also asked to rate their pain's severity (mild, moderate, or severe) and whether the participants attributed their pain to their work. The demographic data served as a grouping variable for the study, while the NMQ results served as the outcome variables.
Data management and statistical plan
Data were entered into SPSS 20, IBM, Armonk, NY, United States of America. Categorical variables were described as frequencies and percentages. Chi-Square test and logistic regressions were used to assess the relationship between the outcome variable (categorical variables for musculoskeletal pain) and baseline characteristics.
Results
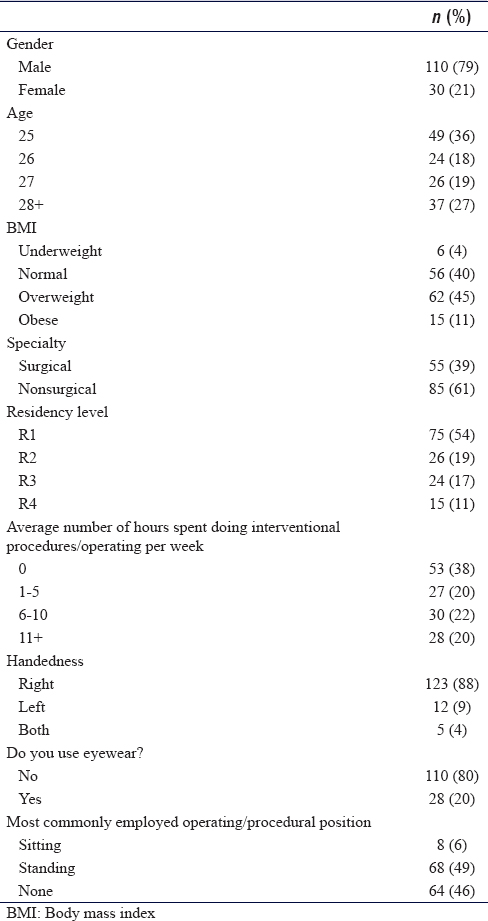
The demographic profile of all residents who participated in the study is shown in [Table - 1]. Gender distribution was 79% of male residents and 21% of female residents (3.7:1, male-to-female ratio). In the surgical group, there were 9 female residents (male residents: n = 46), and in the nonsurgical group, there were 21 female residents (male residents: n = 64). Residents' mean age was 27 years (range: 24–34). The majority of residents were overweight. Surgical and nonsurgical resident distribution was 39% and 61% (n = 55 and 85, respectively), in accordance with the sample size calculation.
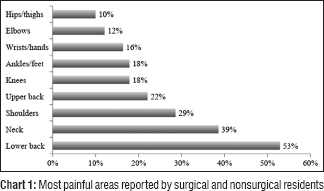
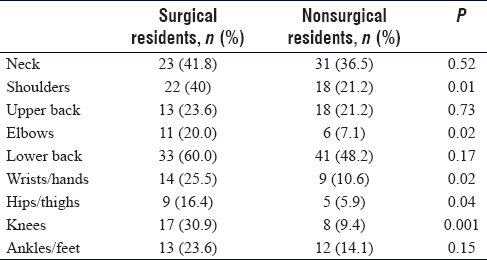
Reports of pain in all areas of interests are depicted in [Chart 1]. The majority of residents who suffer from pain suffered from either lower back (53%) or neck pain (39%). When asked to characterize exactly what they felt, 64% reported feeling general pain, and 18% felt stiffness in the affected areas. Only 26% had symptoms in the 12 months before their participation in the study and 24% had symptoms 7 days prior. While both groups complained of musculoskeletal pain in varying degrees, there was a significant difference when surgical and nonsurgical groups were compared, specifically in the complaint of knees (P = 0.001), shoulder (P = 0.01), wrists/hands (P = 0.02), elbow (P = 0.02), and hips/thighs (P = 0.04), as shown in [Table - 2].
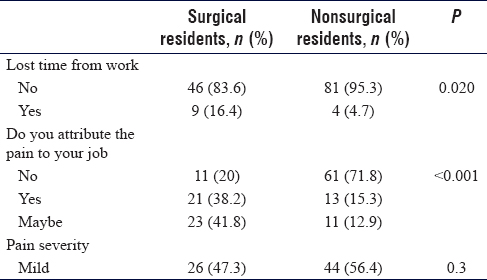
Surgical residents also seem to be more likely to lose time from work due to their pain (16% vs. 4%; P = 0.02) and were more likely to attribute their pain to their profession (38% vs. 15%; P ≤ 0.001). As for the severity of pain when comparing both groups, there is a noticeable, however statistically insignificant, higher or more painful rating reported by surgical residents. Body mass index (BMI), classified as underweight (BMI below 18.5), normal (BMI between 18.5 and 25), overweight (BMI between 25 and 29), and obese (BMI higher than 30), did not affect reports of pain, except when it came to participants' lower back (P = 0.04), with 40% (n = 25) of underweight/normal reported pain compared to 62.9% (n = 39) of overweight and 60% (n = 9) of obese residents. Reports of time lost, attribution of pain to the profession, and pain severity are shown in [Table - 3].
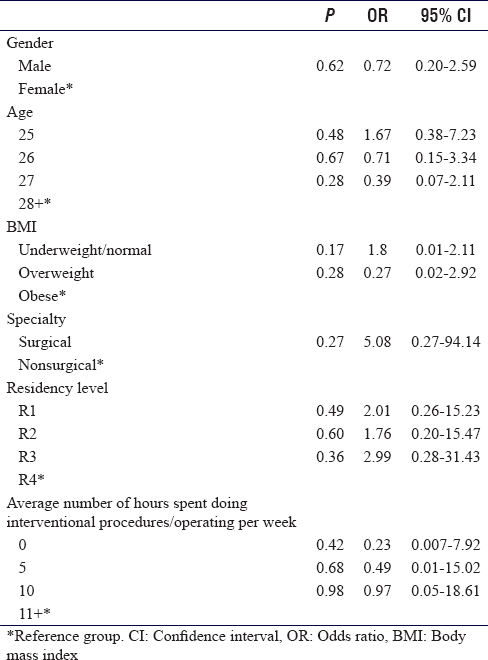
Univariate logistical regression was done to determine the likelihood of experiencing musculoskeletal pain with each baseline characteristic, as depicted in [Table - 4]. While there was no significant result with any of the characteristics analyzed, surgical residents were more likely to report musculoskeletal pain than nonsurgical residents (odds ratio [OR] = 5.08 and confidence interval [CI] = 0.27–94.14). Moreover, residents who spent more time doing interventional procedures or in the operating room reported having musculoskeletal pain more often (10 h; OR = 0.97 and CI = 0.05–18.61).
Discussion
Work-related musculoskeletal complaints are a prevalent issue among health-care providers. Previous literature has identified high rates of musculoskeletal disorders among surgeons, physicians, and dentists.[13],[21],[22] This study found that musculoskeletal complaints are similarly high among nonsurgical specialty and surgical residents. When asked whether the musculoskeletal complaints were related to the nature of their profession, a significant difference was noted between surgical and nonsurgical specialty residents where more surgical specialty residents attributed their occupation as a cause for their musculoskeletal complaints.
In our cross-sectional study, we found that 83% of the study population had at least one painful or stressing musculoskeletal complaint with lower back and neck pain being the most common complaints, respectively. Compared with a previous article on a similar population, elbow pain and back pain were the main complaints, respectively.[23] Our population's most common musculoskeletal complaints (lower back and neck) were similar to Rambabu and Suneetha's reports in both surgical and nonsurgical medical professions.[11]
Nonsurgical residents reported less musculoskeletal complaints than the surgical resident in our study. While both groups complained of musculoskeletal pain in varying degrees, there was a significant difference when surgical and nonsurgical groups were compared, and surgical specialty residents scored higher musculoskeletal complaints specifically in the complaints of the shoulder, elbow, wrists/hands, hips/thighs, and knees.
Our survey results were comparable to previous studies, notably in our surgical population. Knudsen et al. reported that orthopedic surgeons complained of musculoskeletal pains specifically in the neck (59.4%), lower back (54.8%), upper back (35.5%), and shoulders (34.4%), whereas our surgical residents reported pains in the lower back (60%), neck (41.8%), shoulders (40%), and upper back (23.6%).[20] Auerbach et al. found comparable results when surveying spine surgeons' musculoskeletal complains as follows: lower back (62.2%), neck (59.4%), and shoulders (48.5%). These results are of concern due to our population being younger residents in their early career stages.
Occupational musculoskeletal comorbidities are a prevalent issue as reported in our study and numerous other articles. It is also the cause of chronic pains, loss of working days, and care seeking. Even though no resident suffered a potentially career-ending injury in our study, which can be explained by the young age of our study population, it was the cause of multiple absenteeism from work. Of all the surgical residents, 16% had days lost from work and more than a third of surgeons attributed their complaints to their occupation compared to 4.7% of nonsurgical residents. The nonsurgical population were similar to Rambabu and Suneetha's medical population regarding time lost from work, 6% versus our population's 4.7%; however, the surgical population was almost double of ours, 29% versus 16%.[11]
In the current study, we found no association between BMI, musculoskeletal pain, and associated symptoms after the univariate logistic regression was done. This was similar to what Al-Mohrej et al. found when assessing musculoskeletal pain complaints and its association with BMI among dental practitioners working in Riyadh.[24] Rambabu and Suneetha, on the other hand, found that being overweight or obesity was a significant risk factor for musculoskeletal pain when assessing dentists, surgeons, and physicians.[11] In addition, when compared to nonmedical specialties, there was a clear association between BMI and musculoskeletal complaints. For example, Moreira-Silva et al. found a clear association between weight and musculoskeletal complaints when assessing Portuguese factory workers. Overweight/obese factory workers in Portugal reported more frequent pains in their shoulders and wrist/hand in the past 12 months compared with their normal-weight counterparts.[25]
Previous literature has suggested that female surgeons have a higher prevalence of musculoskeletal pains than male surgeons. However, these reports had a limited number of female surgeons participating.[5],[26] Adam et al. reported that female gender was associated with approximately double the risk of reported pain in common anatomical sites when assessing the prevalence of musculoskeletal pain among gynecologic surgeons, where female surgeons were nearly 50% of the population.[27] This was very similar to Alsiddiky et al. reporting where female dental practitioners had double the risk of lower back pain.[24] This was also evident across health professionals in general where female health professionals had 1.9 times higher risk for developing musculoskeletal disorders than their male counterparts.[23] However, in our population being a male proved to be not statistically significant protective factor from musculoskeletal pain.
Even though no association was evident between age, prolonged working hours, and musculoskeletal pain in our population, which could be explained by the fact that they are a younger age group. Previous literature linked age with increased risk of general musculoskeletal pains.[23],[24],[28] Furthermore, the prevalence of musculoskeletal pain significantly increased with the increase of age over 50 years.[29] Studies have also identified extended working hours in ergonomically challenging positions as a prominent risk factor for musculoskeletal pains.[30],[31]
Limitations of the study
As with all convenient sampling studies, this study is highly vulnerable to have biases that both over- and under-represent the overall population as well as selection bias. The sample studied represents residents from one institute; King Abdulaziz Medical City, this may affect the generalizability of our results and may not be representative of other institutes. Finally, equal gender distribution was not achieved in the sample studied and thus might have affected female residents' representation.
Recommendations
Care and ergonomic changes need to be done to the environment in which health-care professionals practice in an effort to enhance productivity and decreased time off work. Surgical residents need to be more aware of the potential risk of experiencing musculoskeletal pain over time and should be educated on ways to avoid or to cope with muscular pain due to work. We recommend that audits, education, and training programs on prevention and coping strategies for musculoskeletal pains should be implemented and compulsory for all health-care providers, as well as providing physical mobility and stretching facility for health-care workers.
Conclusion
Health-care workers are subject to musculoskeletal pain in their work environment. Hence, care needs to be paid to the environment in which health-care professionals practice. Long-term studies combating the limitations of this study may give a better estimate of risk factors and methods of eliminating them to provide a safer work environment, bearing in mind the societal investment put in the health-care systems. Furthermore, expanding on this study by inquiring about other specialties working in the hospital and the areas, they occupy such as wards, laboratories, and clinics.
Ethical considerations
Ethical approval was granted by King Abdullah International Medical Research Center's institutional review board. All willing participants were given a summary of the study's aim attached to the consent sheet. Complete confidentiality was ensured, and participants were informed that they could withdraw themselves at any given time. Participants also received a faculty member's contact information in case they had any questions regarding the study later on.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contributions
AS and SA contrived the idea and designed this study, did the literature review, assembled the questionnaires, gathered the data needed, entered the data on SPSS, wrote the proposal and manuscript. AZ and FZ offered guidance and mentorship, and shared their expertise in the field of orthopedics and musculoskeletal pain. EM did the statistical analysis and aided in interpretation of data. All authors have reviewed and approved the manuscript and are responsible for the content and similarity index of the manuscript.
| 1. | Farlex. Mosby's Dental Dictionary. 2nd ed. 2008. Available from: https://www.medical-dictionary.thefreedictionary.com/occupational+risk. [Last accessed on 2018 Jun 16]. [Google Scholar] |
| 2. | Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: Prevalence and associated risk factors among hospital staff. J Adv Nurs 2009;65:516-24. [Google Scholar] |
| 3. | United States: Department of labour; 2005. Labour Statistics Workplace Injuries and Illnesses in 2005. Available from: https://www.bls.gov/news.release/archives/osh_10192006.pdf. [Last accessed on 2018 Jun 15]. [Google Scholar] |
| 4. | Stomberg MW, Tronstad SE, Hedberg K, Bengtsson J, Jonsson P, Johansen L, et al. Work-related musculoskeletal disorders when performing laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 2010;20:49-53. [Google Scholar] |
| 5. | Szeto GP, Ho P, Ting AC, Poon JT, Cheng SW, Tsang RC. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil 2009;19:175-84. [Google Scholar] |
| 6. | The Health and Occupational Research Network (THOR). University of Manchester Centre for Occupational and Environmental Health (COEH). Available from: http://www.research.bmh.manchester.ac.uk/epidemiology/COEH/research/thor/. [Last accessed on 2018 Jun 21]. [Google Scholar] |
| 7. | Engels JA, van der Gulden JW, Senden TF, van't Hof B. Work related risk factors for musculoskeletal complaints in the nursing profession: Results of a questionnaire survey. Occup Environ Med 1996;53:636-41. [Google Scholar] |
| 8. | Burdorf A, Sorock G. Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health 1997;23:243-56. [Google Scholar] |
| 9. | Babar-Craig H, Banfield G, Knight J. Prevalence of back and neck pain amongst ENT consultants: National survey. J Laryngol Otol 2003;117:979-82. [Google Scholar] |
| 10. | Soueid A, Oudit D, Thiagarajah S, Laitung G. The pain of surgery: Pain experienced by surgeons while operating. Int J Surg 2010;8:118-20. [Google Scholar] |
| 11. | Rambabu T, Suneetha K. Prevalence of work related musculoskeletal disorders among physicians, surgeons and dentists: A comparative study. Ann Med Health Sci Res 2014;4:578-82. [Google Scholar] |
| 12. | Auerbach JD, Weidner ZD, Milby AH, Diab M, Lonner BS. Musculoskeletal disorders among spine surgeons: Results of a survey of the scoliosis research society membership. Spine (Phila Pa 1976) 2011;36:E1715-21. [Google Scholar] |
| 13. | Alsiddiky AM, Algarni N, Alluhaidan A. Prevalence and associated factors of low back pain among clinicians of A major referral hospital. Med J Malaysia 2015;70:12-7. [Google Scholar] |
| 14. | Hadler NM, Tait RC, Chibnall JT. Back pain in the workplace. JAMA 2007;297:1594-6. [Google Scholar] |
| 15. | Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Back pain exacerbations and lost productive time costs in United States workers. Spine (Phila Pa 1976) 2006;31:3052-60. [Google Scholar] |
| 16. | Mohseni-Bandpei MA, Ahmad-Shirvani M, Golbabaei N, Behtash H, Shahinfar Z, Fernández-de-las-Peñas C, et al. Prevalence and risk factors associated with low back pain in Iranian surgeons. J Manipulative Physiol Ther 2011;34:362-70. [Google Scholar] |
| 17. | Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95-103. [Google Scholar] |
| 18. | Mollazadeh M, Saraei M. Sickness absenteeism of Healthcare Workers in a Teaching Hospital; 2018. Available from: http://www.jhpr.ir/article_57054_ab9bdae815bd13de8b2575f30e0792a4.pdf. [Last accessed on 2018 Aug 07]. [Google Scholar] |
| 19. | Iowa R. Java Applets for Power and Sample Size; 2018. Available from: https://www.homepage.divms.uiowa.edu/~rlenth/Power/. [Last accessed on 2018 Jun 07]. [Google Scholar] |
| 20. | Knudsen ML, Ludewig PM, Braman JP. Musculoskeletal pain in resident orthopaedic surgeons: Results of a novel survey. Iowa Orthop J 2014;34:190-6. [Google Scholar] |
| 21. | Narayan A, Ottayil Z, Bhaskaran U, Lahoti S. Prevalence of musculoskeletal disorders among doctors in Mangalore: A cross-sectional survey. Int J Health Allied Sci 2014;3:204. [Google Scholar] |
| 22. | Alsiddiky AM, Alatassi R, Altamimi SM, Alqarni MM, Alfayez SM. Occupational injuries among pediatric orthopedic surgeons: How serious is the problem? Medicine (Baltimore) 2017;96:e7194. [Google Scholar] |
| 23. | Yasobant S, Rajkumar P. Work-related musculoskeletal disorders among health care professionals: A cross-sectional assessment of risk factors in a tertiary hospital, India. Indian J Occup Environ Med 2014;18:75-81. [Google Scholar] |
| 24. | Al-Mohrej OA, AlShaalan NS, Al-Bani WM, Masuadi EM, Almodaimegh HS. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: A cross-sectional study. BMJ Open 2016;6:e011100. [Google Scholar] |
| 25. | Moreira-Silva I, Santos R, Abreu S, Mota J. Associations between body mass index and musculoskeletal pain and related symptoms in different body regions among workers. SAGE Open 2013;3:215824401349195. [Google Scholar] |
| 26. | Capone AC, Parikh PM, Gatti ME, Davidson BJ, Davison SP. Occupational injury in plastic surgeons. Plast Reconstr Surg 2010;125:1555-61. [Google Scholar] |
| 27. | Adams S, McKinney J, Rosenblatt P. Musculoskeletal pain and disorders among gynecologic surgeons. J Minim Invasive Gynecol 2012;19:S29. [Google Scholar] |
| 28. | Dragioti E, Larsson B, Bernfort L, Levin LÅ, Gerdle B. A cross-sectional study of factors associated with the number of anatomical pain sites in an actual elderly general population: Results from the PainS65+ cohort. J Pain Res 2017;10:2009-19. [Google Scholar] |
| 29. | Woolf AD, Akesson K. Understanding the burden of musculoskeletal conditions. The burden is huge and not reflected in national health priorities. BMJ 2001;322:1079-80. [Google Scholar] |
| 30. | Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord 2004;5:16. [Google Scholar] |
| 31. | Phedy P, Gatam L. Prevalence and associated factors of musculoskeletal disorders among young dentists in Indonesia. Malays Orthop J 2016;10:1-5. [Google Scholar] |
Fulltext Views
3,620
PDF downloads
1,484





