Translate this page into:
Correlation between functionality and satisfaction index after total hip or knee replacement
Corresponding Author:
Alejandro Miravete-Galvez
ABC Medical Center, Mexico City
Mexico
dr.miravete@gmail.com
| How to cite this article: Miravete-Galvez A, Serrano-Ardila AM, Camacho-Galindo J. Correlation between functionality and satisfaction index after total hip or knee replacement. J Musculoskelet Surg Res 2020;4:213-217 |
Abstract
Objectives: The evaluation of a successful replacement surgery varies between physicians and patients. Approximately 1 in 5 patients undergoing this type of joint surgery are not satisfied with the result obtained 12 months after their surgery. The aim of this work is to find out the correlation between satisfaction and functionality in patients with either osteoarthritis (OA) or inflammatory joint disease (IJD) who had undergone knee or hip replacement surgery in our institution charity clinic, the satisfaction with program's surgery rate and to the patients' clinical improvement. Methods: This is a prospective cross-sectional study with patients who underwent surgery between 2015 and 2018. The Self-Administered Patient Satisfaction Scale (SAPS) questionnaire was applied at least 12 months after the procedure and correlated to the functional scales Harris hip score (HHS) or Knee Society Score (KSS). Results: The HHS and KSS functional scales had a good and statistically significant correlation with the SAPS of 0.44 (P < 0.001). The program's satisfaction index for surgery had a mean of 95%. Pre- and post-operative assessments (at least 12 months) of the HHS/KSS functional scales obtained an initial median of 39.14 points and a final result of 87 for IJD and 93 for OA with a mean of 90 points (P = 0.000). Conclusions: The correlation between SAPS and the functional scores (HHS/KSS) 0.44 is good/moderate and it is statistically significant. The satisfaction with the program's surgery rate based on SAPS had a mean of 95%. Functionality assessed with HHS/KKS had a mean of 90 points. Using SAPS and HHS/KSS scales, we can conclude that the patients had a favorable clinical outcome. According to SAPS, IJD patients have better satisfaction indices than OA even though they have worst functional end results.
Introduction
Total knee replacement (TKR) and total hip replacements (THR) are two of the most common orthopedic surgeries and are projected to increase in the upcoming decades. Joint replacement surgery aims to reduce pain and restore function to improve the quality of life for patients with end-stage arthritis. In this regard, TKR and THR are clinically proven and cost-effective procedures.[1],[2],[3]
The success or failure of joint replacement surgery is traditionally evaluated using hard endpoints such as infection, implant failure, the need for revision surgery, and functional scales (articular range of motion, strength, and performance of daily activities).[1],[4]
There is great disagreement between the results evaluated by surgeons and those reported by patients. In knee and hip joint replacement, between 9% and up to 30% of postoperative patients reported not being satisfied with the results of their surgery.[1],[5] Kahlenberg et al., in a systematic review found that the median reported percentage of satisfaction was over 88.9%. Because this is a well-documented discrepancy it is of utter importance to adequately measure satisfaction.[1],[4],[6],[7]
The meaning of satisfaction can vary from person to person, furthermore, the satisfaction measurement is complex, and that is why it is necessary to use standardized and reproducible scales to evaluate this parameter such as the New Knee Society Knee Scoring System (KSKSS) and the Self-Administered Patient Satisfaction Scale for Primary Hip and Knee Arthroplasty (SAPS).[1],[8],[9],[10],[11]
Our study's importance is to see if with the current available tools we can evaluate more thoroughly our outcomes not only based on hard end points and physician based scales, but including satisfaction as fundamental parameter.
The objectives of this study were to find out the correlation between satisfaction and functionality in patients with either osteoarthritis (OA) or inflammatory joint disease (IJD) who had undergone knee or hip replacement surgery in our institution charity clinic, the program's satisfaction with surgery rate and the patients' clinical improvement. To assess the level of satisfaction, a standardized scale was used (SAPS) and for functionality the Harris hip score (HHS) and the Knee Society Score (KSS) were applied as they are the standard scales used at the clinic.
SAPS is a previously Spanish translated validated index, which has a high internal consistency, which should make it a valid instrument for measuring satisfaction with the outcome of total joint replacement.[5] The functional scales in combination with SAPS were used to evaluate the clinical improvement of patients who underwent hip and knee replacement surgery between the years 2015 and 2018.
Subjects and Methods
This is a prospective cross-sectional study with patients treated at the clinic of the joint replacement surgery program of the “Amistad charity clinic” of the ABC Medical Center, who had undergone TKR or THR surgery between 2015 and 2018.
Patients were included in this study if they belonged to the joint replacements program of the ABC Amistad Clinic, had a follow-up of at least 12 months after surgical intervention and the base diagnosis was either osteoarthritis or IJD. Patients excluded from this study were those with a different diagnosis such as posttraumatic OA, fractures, Parkinson's disease and those who suffered from a severe postoperative complication (need for surgical reintervention for any cause: peri-implant infection, septic/aseptic loosening, fracture, and rupture of the extensor apparatus). Other simple complications such as wound infection, postoperative fever, and bleeding, neural deficits were all included.
The clinical information, demographic data, preoperative clinical status HHS/KSS (which was performed by a trained orthopedic surgeon) were obtained retrospectively directly from the ABC Medical Center digital medical records. All surgical procedures were performed by the same surgeon, who is an expert in joint replacement surgery. For the functional evaluation (HHS, KSS) and the completion of the satisfaction questionnaire (SAPS), the patients were contacted by telephone by the social worker staff of the ABC Amistad charity Clinic. The nature of their appointment was explained. Once in consultation, the patient's informed consent was obtained, and doubts were resolved prior to their participation in this study. All clinical evaluations (HHS, KSS) were performed by the first author who is not part of the joint replacement program.
The SAPS Survey was answered individually and anonymously by each patient. It consists of four specific questions aimed at knowing: the patient's overall satisfaction with the surgery, pain improvement, ability to do housework or gardening, and the ability to perform recreational activities. Each question had four possible answers: very satisfied (100 points), somewhat satisfied (75 points), somewhat unsatisfied (50 points), and very unsatisfied (25 points). The scale score is the unweighted average of the scores obtained in each question, ranging from 25 to 100 points.[5]
Statistical analysis
The data obtained were exported to the SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc. for statistical analysis. Initially, the frequency was estimated for diagnosis, gender, affected side, and involved joint, while the mean value was estimated for age. The median (Md) and percentile 25–75th were estimated for preoperative and 1-year postoperative HHS and KSS, as well as 1-year postoperative satisfaction questionnaire. Presurgical evaluation with HHS and KSS was compared with the 1-year evaluation using the Wilcoxon test. The postoperative 1-year HHS and KSS were compared to the satisfaction questionnaire through the Spearman correlation test. In both cases, a P < 0.05 was considered statistically significant.
Results
Within the established period, the records obtained indicate that a total of 67 surgeries (51 patients), 22 THR, and 45 TKR were performed. Patients' age ranged between 29 and 91 years, with an average of 62.5 years.
Five patients could not be contacted, and five patients were ruled out from the study. Two patients were ruled out as the diagnosis was different from those established for this study: one with Parkinson's disease, and the other one with sequelae of the developmental dysplasia of the hip. The other three patients were ruled out for presenting with postoperative severe complications; one for the rupture of the extensor apparatus post-TKR (involved in a car accident), another one for aseptic loosening of the femoral stem, and the last one for dehiscence of the surgical wound and patella fracture post-TKR (following a fall from her own height) [Figure - 1].
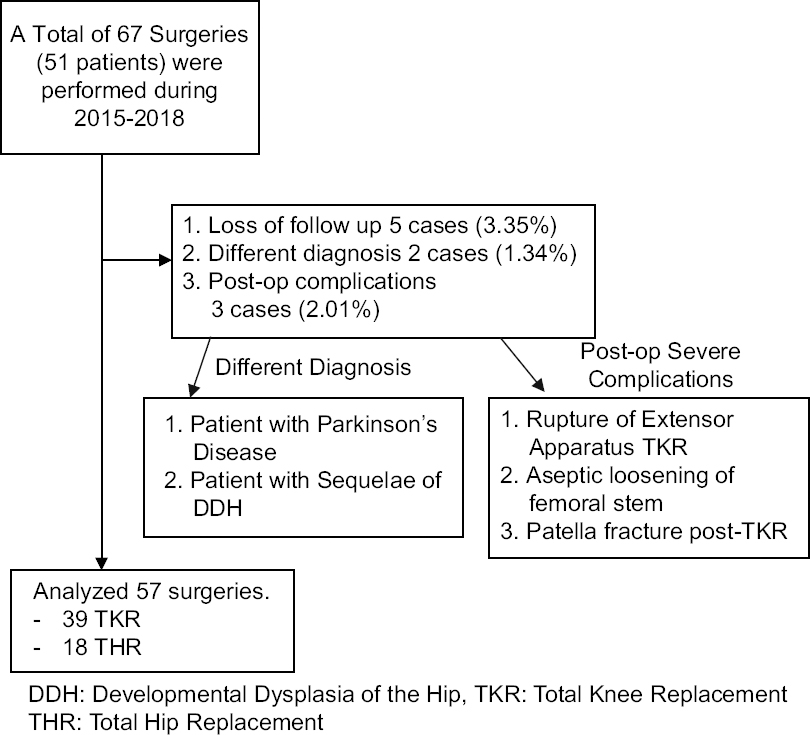 |
| Figure 1: Flowchart for patient selection |
Characteristics of the population studied
OA was the most common base diagnosis in our population, representing 59.6% of cases. The right lower extremity was the most affected with (59.6%). The most prevalent gender was female, with 91.3% of the total, and the most commonly affected joint was the knee (68.42%) [Table - 1].

The satisfaction index evaluated by SAPS obtained a mean score of 95% ± 7.7% (median and 25–75th percentile). Of the total number of patients, 5 (8.77%) reported being somewhat satisfied with all the items evaluated by SAPS, that is, 75 out of 100 possible points on the scale. One was a post-THR patient and 4 post-TKR patients.
Eleven patients: 3 post-THR patients and 8 post-TKR patients obtained a score of 93.75 points. All of them agreed that they were “somewhat satisfied” with the results of the surgery to improve their ability to perform recreational activities. All the 23 patients diagnosed with IJD, scored 100% in the SAPS index. Pre- and post-operative assessments (at least 12 months after surgery) of the HHS and KSS functional scales obtained an initial median of 39.14 points (25–75 percentile, 32–45). The final result was 90 points (82–94.5) with P = 0.000 applying the U of Mann–Whitney [Table - 2].

The correlation between patient satisfaction evaluated using the SAPS questionnaire and the HHS and KSS functional scales obtained a Spearman coefficient of 0.44, with a 95% confidence interval of 0.31–0.56 (P < 0.001).
Discussion
The way the success or failure of a hip and knee joint replacement results are evaluated has evolved from solely focusing on functional clinical results to being complemented by self-applicable satisfaction surveys, this with the intention of evaluating the process of provided medical care more fully.[5]
For the evaluation of the correlation, we considered a Spearman coefficient >0.3 to be clinically significant. This was based on a study by Kwong etal.[8] where the result was interpreted as follows a) almost perfect: 0.81–1.00, excellent 0.61–0.80, good (moderate) 0.41–0.60, accep[table “” not found /]
.21–0.40, and low 0.00–0.20.
With this information, we can affirm that the correlation found between the functional scales (HHS/KSS) and the SAPS index (0.44) (P < 0.001) is good/moderate and that it is clinically and statistically significant.[8]
According to SAPS, the program's satisfaction with surgery rate has an average of 95% these differs to that found by Kahlenberg in its revision of the literature (88.9%); nevertheless, this must be interpreted carefully because their results are based on a great heterogeneity of studies where out of 208 studies only 27 used “validated” scales.[1]
We attribute the program's satisfaction with surgery results to three main maneuvers, first the implementation of a multimodal analgesia as proposed by Halawi et al.[12] In this program, all patients undergoing joint replacement surgery have a previous consultation with the surgeon where expectations, fears and limitations of the surgery are extensively discussed. One hour before the surgery, 1000 mg of intravenous paracetamol/acetaminophen and 40 mg of intravenous parecoxib are administered, once in the operating room the surgery is performed under sedation and a combined spinal anesthesia using a combination of hyperbaric bupivacaine and morphine for the subarachnoid space and ropivacaine 7.5% for the epidural space, in the case of TKR a series of ultrasonography guided peripheral nerve blocks are performed including femoral and the adductor canal using ropivacaine 7.5% plus clonidine. For both hips and knees before first incision is made, we infiltrate both the subcutaneous and joint space with a combination of xylocaine/epinephrine and morphine with the intent of blocking directly nociceptors before they are stimulated. In the postoperative phase, the peridural catheter is used for continuous administration of ropivacaine 0.15% for 24 h, parecoxcib is continued every 12 h and paracetamol/acetaminophen every 8 h. After discharge, patients are instructed to use acetaminophen/tramadol tablets every 6–8 h as needed for 1 week. The rehabilitation program starts the same day of the surgery and patients are assigned to a specific rehabilitator who is in charge for each individual through hospitalization (2–3 days) and after discharge, patients are seen at least once a week for the 1st month by this personal physiotherapist. In agreement with the surgeon, it is decided when the sessions can be made at home and without further supervision. Although this a social assistance program, patients have access to one of the group physicians at every time for any doubts. Consultations are made at 10 days, then 2 weeks, 6 and 12 weeks, at any point if needed the patient is explored between these intervals, making the doctor–patient relationship a priority probably resulting in better satisfaction scores.[1],[10],[12]
Because all surgeries were performed by the same orthopedic surgeon, we avoided a possible performance bias. The SAPS and postoperative HHS/KSS were evaluated by the first author who is not part of the reconstruction team and did not participate in any of the surgeries; as such, he is not influenced in the veracity of the results published.
The heterogeneity in the base diagnoses of the patients' OA and IJD usually involves different age groups. The former being elderly patients while the latter are usually younger. It should be noted that patients with the diagnosis of IJD obtained a satisfaction rate of 100% (95% confidence interval from 86 to 100%) regardless of the joint operated on, and despite having a lower average score on the functional scales pre- and post-operatively than OA patients. These results concur with those found by Minator etal. where after 12 months of surgery, they concluded that satisfaction indices were not different between these groups. Although Minator etal. did not use validated scales to evaluate satisfaction as they only compared the Oxford Knee Score and the Knee Injury and OA Outcome Score, which are not specific satisfaction measurement tools.[13],[14]
It was hard to understand our results, as we expected that patients with IJD would have worst satisfaction indices compared to those with OA. This presumption was based on the fact that IJD patients usually have worst functional outcomes, stiffness and more propensity to present with postoperative complications. We thought this should reflect in worst satisfaction indices. Yet in our study they are more satisfied than those with OA. A possible explanation for this result is that patients' expectations were addressed before surgery, and because of the type of patient our clinic attends to, they usually have severe disease. The severity of their preoperative conditions may have led to a perception of wellness even though their range of motion (ROM) and functional scales were not ideal.[15],[16]
For the correct interpretation of this study, it is important to take into account several limitations. Although patients with simple complications such as wound infection, postoperative fever, bleeding, and neural deficit were all included, there were three patients with severe complications that were excluded from this study, this could lead to a bias in the results. When running the statistical analysis giving these three excluded patients, the worst possible outcome of surgery was 91.84 satisfaction rate. There could be an “interviewer” bias, even though satisfaction surveys were answered anonymously; if there was any doubt about the questionnaire, the same researcher was in charge of solving them. Another possible bias is that patients responded what the researcher wanted to hear. Attempts to control these biases were made by explaining the anonymous nature of their responses and that no one but the main researcher and themselves would know the answers. At all times, the importance of the veracity of their responses was emphasized so that this would help the program's continuous improvement.
The characteristics of the studied population must be analyzed before attempting to extrapolate to other populations. This sample presents a wide dominance of the female gender (91.2%) and patients with an average age of 62.5 years. It is worth mentioning that the average age of our patients is lower than other international records which varies between 69 and 71 years.[17] In a study made by Fang M where their objective was to describe age-related differences in outcomes among older adults undergoing THR or TKR they found out that compared to younger patients, older THR and TKR recipients were more likely to experience postoperative complications, admission to the intensive care unit and longer hospitalizations, which can possibly be reflected on worst satisfaction indices.[18]
We had a higher prevalence of females undergoing these procedures, compared to a similar paper by Kwon et al., with an incidence of 70.9% of females, it is not illogical to think that the physical demand and expectations of an elder population and mainly females are different from other age groups and gender.[8],[9],[10],[19],[20],[21],[22],[23]
Measuring satisfaction remains a great challenge, currently there are only two “truly” validated scales for joint replacement: the SAPS and the KSKSS (non was found for THR) and even this two are far from an ideal scale, as they both failed assessment for content validity due to lack of patient involvement during their development and testing.[11]
Conclusions
The correlation between SAPS and the functional scores (HHS/KSS) was 0.44, which is good/moderate and it is clinically and statistically significant. The program's satisfaction with surgery rate based on SAPS has a mean of 95%. Functionality assessed with HHS/KKS with an initial median of 39.14 points had a final result of 87 for IJD and 93 for OA with a mean of 90 points. Using SAPS and HHS/KSS scales, we can conclude that the patients had a favorable clinical outcome. According to SAPS, IJD patients have better satisfaction indices than OA even though they have worst functional end results.
Recommendations
We recommend to apply SAPS or any other validated questionnaire as for now they are the best tools we have to evaluate satisfaction in joint replacement surgeries. We recommend to use a multimodal analgesic program added to a close and personal supervision of the patients.
We think that there is still a lot to do for improving the way we measure satisfaction, the good and statistical significant correlation that we found between the SAPS and KSS/HHS in both OA and IJD patients makes us believe that we are still stuck measuring physicians outcomes instead of how really the patient feels.
Ethical considerations
The study was approved by the Research Ethics Committee of the ABC Medical Center on 12th of March 2019 vide the approval number is ABC-19-08. The patients' informed consent was obtained before their participation in this study, with only the researchers were able to access the data.
Acknowledgments
We would like to thank Dr. José A. Jacome Mondragon head of The ABC Amistad clinic, for granting us access to the clinics patients and making the process easier.
We specially thank Dr. Juan O. Head of Teaching department at The ABC Medical Center for his help in the statistical analysis of this study.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AMG, AMSA, and JCG contributed with concepts, design, definition of intellectual content, clinical study, manuscript preparation, editing, and review. AMG was in charge of applying questioners and objective functional scales. AMG, AMSA have contributed to statistical analysis and interpretation of the results. JCG was the expert surgeon performing all the surgeries. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: A systematic review. HSS J 2018;14:192-201. [Google Scholar] |
| 2. | Baker PN, Rushton S, Jameson SS, Reed M, Gregg P, Deehan DJ. Patient satisfaction with total knee replacement cannot be predicted from pre-operative variables alone: A cohort study from the National Joint Registry for England and Wales. Bone Joint J 2013;95-B:1359-65. [Google Scholar] |
| 3. | Nwachukwu BU, Bozic KJ, Schairer WW, Bernstein JL, Jevsevar DS, Marx RG, et al. Current status of cost utility analyses in total joint arthroplasty: A systematic review. Clin Orthop Relat Res 2015;473:1815-27. [Google Scholar] |
| 4. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Google Scholar] |
| 5. | Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis 2011;2011:591253. [Google Scholar] |
| 6. | Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012;2:e000435. [Google Scholar] |
| 7. | Lavernia C, Guzman J, Gachupin-Garcia A. Cost Effectiveness and Quality of Life in Knee Arthroplasty. Clin Orthop Relat Res 1997;345:134-9. [Google Scholar] |
| 8. | Kwon SK, Kang YG, Kim SJ, Chang CB, Seong SC, Kim TK. Correlations between commonly used clinical outcome scales and patient satisfaction after total knee arthroplasty. J Arthroplasty 2010;25:1125-30. [Google Scholar] |
| 9. | Shirley ED, Sanders JO. Patient satisfaction: Implications and predictors of success. J Bone Joint Surg Am 2013;95:e69. [Google Scholar] |
| 10. | Okafor L, Chen AF. Patient satisfaction and total hip arthroplasty: A review. Arthroplasty 2019;1:6. [Google Scholar] |
| 11. | Klema NR, Kent P, Smitha A, Dowseyc M, Farya R, Schützea R. Satisfaction after total knee replacement for osteoarthritis is usually high, but what are we measuring? A systematic review. Osteoarthritis Cartilage Open 2020;2:1, 100032. [Google Scholar] |
| 12. | Halawi MJ, Grant SA, Bolognesi MP. Multimodal Analgesia for Total Joint Arthroplasty. Orthopedics 2015;38:e616-25. [Google Scholar] |
| 13. | Kapetanovic MC, Lindqvist E, Saxne T, Eberhardt K. Orthopaedic surgery in patients with rheumatoid arthritis over 20 years: Prevalence and predictive factors of large joint replacement. Ann Rheum Dis 2008;67:1412-6. [Google Scholar] |
| 14. | Minator Sajjadi M, Keyhani S, Kazemi SM, Hanafizadeh B, Ebrahimpour A, Banasiri M. Patient satisfaction following total knee arthroplasty: Comparison of short-term results in rheumatoid arthritis and osteoarthritis. Arch Bone Jt Surg 2019;7:61-6. [Google Scholar] |
| 15. | Singh JA, Inacio MC, Namba RS, Paxton EW. Rheumatoid arthritis is associated with higher ninety-day hospital readmission rates compared to osteoarthritis after hip or knee arthroplasty: A cohort study. Arthritis Care Res (Hoboken) 2015;67:718-24. [Google Scholar] |
| 16. | Ravi B, Escott B, Shah PS, Jenkinson R, Chahal J, Bogoch E, et al. A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum 2012;64:3839-49. [Google Scholar] |
| 17. | Porter M, Armstrong R, Howard P, Porteous M, Wilkinson JM. Orthopaedic registries - the UK view (National Joint Registry): Impact on practice. EFORT Open Rev 2019;4:377-90. [Google Scholar] |
| 18. | Fang M, Noiseux N, Linson E, Cram P. The effect of advancing age on total joint replacement outcomes. Geriatr Orthop Surg Rehabil 2015;6:173-9. [Google Scholar] |
| 19. | Thambiah MD, Nathan S, Seow BZ, Liang S, Lingaraj K. Patient satisfaction after total knee arthroplasty: An Asian perspective. Singapore Med J 2015;56:259-63. [Google Scholar] |
| 20. | Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res 2006;443:266-72. [Google Scholar] |
| 21. | Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 2005;87:1487-97. [Google Scholar] |
| 22. | Wainwright C, Theis JC, Garneti N, Melloh M. Age at hip or knee joint replacement surgery predicts likelihood of revision surgery. J Bone Joint Surg Br 2011;93:1411-5. [Google Scholar] |
| 23. | Sloan M, Premkumar A, Sheth NP. Projected Volume of Primary Total Joint Arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018;100:1455-60. [Google Scholar] |
Fulltext Views
1,864
PDF downloads
376





