Translate this page into:
Correlation of preoperatively predicted and intraoperative soft-tissue releases in total knee arthroplasty
2 Department of Surgery, Division of Orthopaedic Surgery, Hamilton Health Sciences, McMaster University, Hamilton, Canada
3 Department of Surgery, Division of Orthopaedic Surgery, London Health Sciences Centre University Campus, University of Western Ontario, London, Ontario, Canada
Corresponding Author:
Mohammad M Alzahrani
Department of Orthopaedic Surgery, College of Medicine, Imam Abdulrahman Bin Faisal University, 2835 King Faisal Road, Dammam 34212
Saudi Arabia
mmalzahrani@iau.edu.sa
| How to cite this article: Alzahrani MM, Wood TJ, Somerville LE, Howard JL, Vasarhelyi EM, Lanting BA. Correlation of preoperatively predicted and intraoperative soft-tissue releases in total knee arthroplasty. J Musculoskelet Surg Res 2020;4:210-212 |
Abstract
Objectives: Soft-tissue balancing is one of the key components to achieving a successful total knee arthroplasty (TKA), but the planned soft-tissue release may not always correlate with the required releases intraoperatively to achieve a balanced knee. The aim of our study is to explore whether these required releases can be predicted accurately preoperatively and if their accuracy correlates with the level of training. Methods: Two hundred and fifty-one patients undergoing primary TKA were included in the study. Preoperatively, the consultant, fellow, and resident independently predicted the required releases to gain a balanced knee. Postoperatively, the performed releases were recorded and compared to the preoperative predictions. Results: Consultants had the highest exact match (62%), while the fellows and residents were less accurate (57% and 58%, respectively). Fellows and consultants had the least deviation of their prediction from the performed soft-tissue release. The intraclass correlation coefficients were also highest for consultants, followed by fellows and then residents, but this was not statistically significant. Conclusion: We found that participants irrespective of their level of training were able to accurately predict the required soft-tissue balancing in TKA. We believe this can be a valuable educational and assessment tool for trainees at all levels.
Introduction
Symptomatic osteoarthritis (OA) of the knee is commonly managed successfully by a total knee arthroplasty (TKA), but several requirements must be met to achieve this successful outcome. These criteria include adequate alignment, soft-tissue balancing, and restoration of the native joint line.[1],[2],[3] To achieve adequate intraoperative soft-tissue balancing, the preoperative alignment of the patient must be adequately assessed, as the majority of patients suffering from knee OA typically present with medial compartmental involvement and thus present with some degree of preoperative varus alignment. While correcting the coronal alignment to a neutral one at the time of TKA has been debated in the current literature,[4],[5],[6],[7],[8] most of the surgeons still aim to correct coronal alignment to a neutral mechanical axis. Thus, the medial soft-tissue structures must be released to balance the knee properly.[1]
There is no universally acceptable progression for the order of soft-tissue releases. Surgeons follow general guidelines typically starting with the release of the deep medial collateral ligament (MCL) and removal of osteophytes, but progression beyond this varies between centers and surgeons.[9]
The objective of our current study is to examine whether the required soft-tissue balancing in TKA can be predicted accurately before surgery and if the level of training in adult joint reconstruction influences the accuracy of this prediction. To the best of our knowledge, this is the first study to assess the soft-tissue balancing prediction in TKA at different training levels.
Materials and Methods
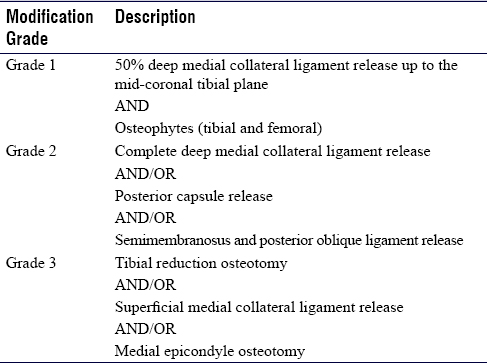
After obtaining ethics approval from the institutional research ethics board, 251 patients undergoing primary TKA were included in the study. All procedures were conducted at a single center by three adult reconstructive fellowship-trained orthopedic surgeons. All patients, with no history of knee surgery or lower extremity trauma, who required TKA for varus OA of the knee and had neutral or varus alignment of their lower extremity as indicated by the preoperative hip to ankle radiographs were included in the study. Prior to each surgery, the attending consultant, fellow, and resident independently recorded the predicted soft-tissue and bone modifications required to achieve a balanced knee. The participants did not discuss the case before recording their predictions, the recording was done without the presence of the other participants, and no changes in the recorded predictions were allowed. Predictions were based solely on information from the patient's chart, clinical examination, and preoperative radiographs. The actual soft-tissue and bone modifications were performed as required to create a balanced knee intraoperatively and the releases were then recorded. The steps to balance the knee were done according to the traditional sequence followed by the arthroplasty surgeons at our center [Table - 1].[9] Data were coded according to the most extensive grade of balancing step the patient received.
The frequency of each modification was calculated and reported using descriptive statistics. Percentages of exact matches between the predicted and actual soft-tissue modifications completed were reported for consultants, fellows, and residents. The percentage of being ±1 release was also reported for each group. Intraclass correlation coefficients (ICCs) and their 95% confidence intervals were calculated for consultants, fellows, and residents. ICC estimates and their 95% confidence intervals were calculated using the Statistical Package for the Social Sciences version 24 (SPSS Inc., Chicago, IL, USA) based on a single-rater, absolute-agreement, 2-way random-effects model.
Results
Of the 251 cases, 18 knees (7%) received 50% deep MCL mid-coronal plane release and 85 knees (34%) received osteophyte (tibial and femoral) removal. Of the remaining cases, 64 knees (25%) received complete deep MCL release, 28 knees (11%) received posterior capsule release, and 23 knees (9%) received semimembranosus and posterior oblique ligament release. A more extensive modification was required in 33 knees, of which 22 (9%) received a tibial reduction osteotomy, 7 (3%) received superficial MCL release, and 4 (2%) received a medial epicondyle osteotomy.
Consultants, fellows, and residents were able to exactly match their prediction to the actual soft-tissue balancing in 62%, 57%, and 58% of the cases, respectively. Consultants, fellows, and residents were able to predict the soft-tissue balancing within ±1 release in 80%, 81%, and 79% of the cases, respectively. The ICC was highest for the consultants (single rater (SR) = 0.596, average rater (AR) = 0.747), followed by the fellows (SR = 0.547, AR = 0.707) and finally, the residents (SR = 0.461, AR = 0.631) with no statistically significant difference between them [Table - 2].

Discussion
Our current study has shown that the ability to correctly predict the required soft-tissue release in patients undergoing TKA was lowest by the residents and fellows involved (58% and 57%, respectively) and the accuracy was higher for the consultants (62%). In addition, the ICC showed a gradual improvement in accuracy as we progressed into higher levels of training, from residents to fellows and finally to consultants, although it did not reach clinical significance.
Correctly predicting the required soft-tissue releases in TKA requires a thorough understanding of the knee's anatomy and mechanics. Therefore, the concept of preoperative prediction of releases to gain a balanced knee can be applied as an element of both trainee education and assessment. With a large number of programs trending toward competency-based training, this tool can act as a way to measure resident and/or fellow progression and understanding of the several concepts encompassed in TKA soft-tissue balancing. This type of training is especially useful to aid in vocational learning, which is an integral part of medical training programs.[10]
Academic teaching, patient-centered care, and intraoperative teaching and skill practice are considered the cornerstone of residency and fellowship training programs.[11],[12] Specific attention has been directed recently toward surgical simulation and its role in both teaching and assessing trainees, showing improved knowledge and skills compared to formal teaching methods.[13],[14],[15] Applying the concept and understanding of releases required to gain a balanced TKA can be presented in the form of a simulation program to assess the trainee's knowledge of both required and sequence of releases. In addition, it can also provide a platform for trainees to perform and evaluate these releases on the simulator, with an ultimate goal of achieving a balanced knee arthroplasty.
Concerning its application in a more formal teaching style, this method of prediction may help foster an optimal learning environment in the operating room and bring about the discussion about one of the more variable aspects of the TKA procedure. This, in turn, will help the trainee gain a better understanding of the principles involved in TKA soft-tissue balancing.
We recognize that there are limitations to this study. There was no objective assessment of the soft-tissue tension and required release, which may have led to a stronger influence of the consultant surgeon on the performed releases. Having an objective tool to assess the knee balance after the release may have minimized this potential bias. Furthermore, since the consultant ultimately performs the soft-tissue balancing after making the prediction, this could have made the consultant appear more accurate than their trainees. Surprisingly, we found no statistically significant difference in the accuracy of prediction between the different participant levels.
Conclusion
Irrespective of the level of training, the participants were able to accurately predict the required soft-tissue balancing in TKA. The resident level had the lowest ability to predict the necessary soft-tissue releases accurately, while consultants had the highest prediction ability, but this did not reach statistical significance. We believe that this can be a valuable educational tool to assess the trainees' understanding of soft-tissue balancing concepts and assess progression through the different levels of training under the umbrella of competency-based training.
Ethical approval
This study has been approved by The Western University Research Ethics Board on 3rd June 2020 under the IRB registration number IRB 00000940. Patient consent was obtained for all participants and is compliant with the Declaration of Helsinki.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Author contributions
MMA, TJW, and LES collected, organized, analyzed, and interpreted data. JLH, EMV, and BAL conceived and designed the study, conducted research, provided research materials and MMA and TJW wrote the initial and final draft of the article and provided logistic support. All the authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: Just how important is it? J Arthroplasty 2009;24:39-43. [Google Scholar] |
| 2. | Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech 2005;38:349-55. [Google Scholar] |
| 3. | Vince KG, Abdeen A, Sugimori T. The unstable total knee arthroplasty: Causes and cures. J Arthroplasty 2006;21:44-9. [Google Scholar] |
| 4. | Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, et al. Tibial component failure mechanisms in total knee arthroplasty. Clinical orthopaedics and related research 2004;(428):26-34. [Google Scholar] |
| 5. | Townley CO. The anatomic total knee resurfacing arthroplasty. Clinical orthopaedics and related research 1985;(192):82-96. [Google Scholar] |
| 6. | Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clinical orthopaedics and related research 1983;(173):178-83. [Google Scholar] |
| 7. | Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 2010;92:2143-9. [Google Scholar] |
| 8. | Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991;73:709-14. [Google Scholar] |
| 9. | Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA. Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 2009;17:766-74. [Google Scholar] |
| 10. | Long DM. Competency-based residency training: The next advance in graduate medical education. Acad Med 2000;75:1178-83. [Google Scholar] |
| 11. | Gil JA, Daniels AH, Weiss AP. Variability in surgical case volume of orthopaedic surgery residents: 2007 to 2013. J Am Acad Orthop Surg 2016;24:207-12. [Google Scholar] |
| 12. | Van Heest A, Putnam M, Agel J, Shanedling J, McPherson S, Schmitz C. Assessment of technical skills of orthopaedic surgery residents performing open carpal tunnel release surgery. J Bone Joint Surg Am 2009;91:2811-7. [Google Scholar] |
| 13. | Rebolledo BJ, Hammann-Scala J, Leali A, Ranawat AS. Arthroscopy skills development with a surgical simulator: A comparative study in orthopaedic surgery residents. Am J Sports Med 2015;43:1526-9. [Google Scholar] |
| 14. | Angelo RL, Pedowitz RA, Ryu RK, Gallagher AG. The Bankart performance metrics combined with a shoulder model simulator create a precise and accurate training tool for measuring surgeon skill. Arthroscopy 2015;31:1639-54. [Google Scholar] |
| 15. | Angelo RL, Ryu RK, Pedowitz RA, Beach W, Burns J, Dodds J, et al. A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy 2015;31:1854-71. [Google Scholar] |
Fulltext Views
2,628
PDF downloads
1,286





