Translate this page into:
Floating elbow in children: Factors associated with serious complications
*Corresponding author: Alberto Daniel Navarro Vergara, Servicio De Ortopedia y Traumatologia, Hospital de Trauma “Manuel Giagni,” General Santos Casi Teodoro S Mongelos, Asuncion, Paraguay. djocote@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vergara ADN, Fretes AN. Floating elbow in children: Factors associated with serious complications. J Musculoskelet Surg Res, 2023;7:259-64.
Abstract
Objectives:
Simultaneous ipsilateral humerus and forearm fractures are rare injuries commonly caused by high-energy trauma. They are known for their higher potential for complications than isolated injuries on the same sites. There is no standardized management nor universally accepted classification for this condition. This study aimed to describe our experience with these injuries.
Methods:
This is a retrospective study of consecutive cases treated from June 2018 to December 2022. The following variables were assessed: age, sex, affected side, mechanism of injury, type of humeral fracture, type of forearm fracture, presence of bone exposure, associated injuries, treatment performed, complications, and elbow functionality according to the Mayo Elbow Performance Score (MEPS).
Results:
Thirty-four cases were analyzed, 58.8% of which were male. The mean age was 6.7 years (6 months–15 years). The most frequent mechanism was spin cycle rotatory injuries. The most affected location in the humerus was the diaphysis (55.8%), and 79.4% of fractures involved both forearm bones. Open fractures accounted for 23.5% of the cases. Regarding the treatments performed, fixation of at least one bone was performed in 32 cases (94%), and both sites were fixed in 24 cases (70.5%). Complications occurred in 26.5% of cases, of which 8.8% were compartment syndromes, and no implant-related infections were reported. All compartment syndromes were related to the torsion trauma caused by the spin cycle rotatory injuries. Elbow function graded according to the MEPS was excellent in 50% of patients.
Conclusion:
Floating elbow injuries are rare serious injuries. Spin cycle rotatory injuries further increase the complexity of treatment and the potential for complications.
Keywords
Pediatrics
Floating elbow
Forearm fracture
Humeral fracture
Mechanism of injury
Spin cycle rotatory injuries
INTRODUCTION
Conventionally, simultaneous ipsilateral humerus and forearm fractures are known as floating elbow injuries, a term coined by Stanitski and Micheli.[1] They described this injury as a condition resulting from high-energy trauma, such as falls from height. This entity is unusual compared to the high incidence of isolated fractures at these sites. The injury pattern usually described in floating elbow injuries is supracondylar fractures of the humerus accompanied by distal metaphyseal forearm fractures[1,2] resulting from elbow hyperextension and wrist dorsiflexion at the time of the injury.[3,4] Higher rates of neurovascular complications and malunion were observed in floating elbow injuries compared to supracondylar elbow fractures in children. Therefore, a floating elbow is deemed to require aggressive treatment, with the need for surgical intervention to reduce the percentage of complications and increase the rate of acceptable functional outcomes.[5] Another advantage of the surgical approach is facilitating the care for skin wounds due to the high rate of associated open fractures.[2] Although floating elbow injuries have been described for years, there is no popular classification for these injuries, unlike similar injuries such as the floating knee, nor is there a definite gold standard treatment protocol for floating elbow injuries.[6,7] This study aimed to describe the cases treated at a trauma hospital, reporting a different mechanism from that traditionally reported. Rotational trauma caused by centrifuge machines has taken on new importance as a cause of floating elbow injuries since it generates fracture patterns and soft-tissue changes different from those generated by falls from height. Therefore, this is a relevant study on a rare serious injury scarcely addressed in local and international literature.
MATERIALS AND METHODS
This is a retrospective, cross-sectional, and analytical study with patients treated from June 2018 to June 2022. The following variables were analyzed: Age, sex, affected side, mechanism of injury, type of humeral fracture, type of forearm fracture, presence of open fracture-associated injuries, treatment performed, complications, and elbow function according to the Mayo Elbow Performance Score (MEPS).[8] Hospital records were analyzed, and data were stored in worksheets specifically designed for this research. Thirty-seven cases were admitted to a trauma hospital with the diagnosis of floating elbow injuries. The study did not include three cases that underwent surgery at another service and were referred to our hospital for better management of soft tissues by the plastic and reconstructive surgery work group and vascular assessment by the vascular surgery department. The pediatric orthopedics department later followed these cases. The trauma mechanism was grouped into two main categories: Direct trauma and spin cycle rotatory injuries trauma [Table 1]. Data were expressed as means and proportions. Intergroup comparison of nominal variables was made using the Chi-square test, odds ratio, and Cramer’s correlation coefficient (R2). Intergroup comparison of continuous variables was made using the Student’s t-test, conducted after the normality test, considering a significance level of P < 0.05 in all cases.
| Morbidity | P | R2 | OR | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| (n=9) | (n=25) | ||||
| Sex | |||||
| Male | 6 | 14 | 0.442 | 9 | 1.5 (0.3–7.7) |
| Female | 3 | 11 | |||
| Affected side | |||||
| Right | 5 | 13 | 0.583 | 3 | 1.1 (0.2–5.3) |
| Left | 4 | 12 | |||
| Age | 3–15 (8±5) | 1–13 (6±3) | 0.018* | 44 | |
| Humerus | |||||
| Diaphysis | 3 | 9 | 0.426 | 5 | |
| Segmental fracture | 2 | 1 | |||
| Gartland II | 0 | 6 | |||
| Spiral diaphysis | 1 | 1 | |||
| Lateral condyle | 1 | 1 | |||
| Metaphysis and diaphysis | 1 | 1 | |||
| Gartland III | 1 | 5 | |||
| Epiphysis | 0 | 1 | |||
| Radius | |||||
| Distal metaphysis | 5 | 18 | 0.307 | 15% | 0.48 (0.1–2.3) |
| Diaphysis | 4 | 7 | |||
| Ulna | |||||
| No | 2 | 5 | 0.253 | 26 | |
| Diaphysis | 6 | 7 | |||
| Distal metaphysic | 1 | 11 | |||
| Physeal | 0 | 1 | |||
| Diaphysis/Olecranon | 0 | 1 | |||
| Open fracture | |||||
| Yes | 5 | 3 | 0.017* | 45 | 9.1 (1.5–54) |
| No | 4 | 22 | |||
| Mechanism | |||||
| Spin cycle rotatory | 6 | 12 | 0.021* | 38 | |
| Fall from height | 1 | 11 | |||
| Vehicle accident | 2 | 2 | |||
| Treatment of humeral fracture | |||||
| IMN | 6 | 7 | 0.027 | 16 | |
| CRPP | 1 | 14 | |||
| Conservative | 0 | 3 | |||
| ORIF | 2 | 1 | |||
| Treatment of forearm fracture | |||||
| CRPP | 3 | 13 | 0.235 | 14 | |
| IMN | 3 | 3 | |||
| Conservative | 2 | 8 | |||
| ORIF/Tension band | 0 | 1 | |||
| CRPP/IMN | 1 | 0 | |||
| Days of hospitalization | 2–10 (5.6±3) | 2–32 (8±4) | 0.001* | 36 | |
RESULTS
The review of medical records from June 2018 to June 2022 obtained 37 medical records diagnosed with floating elbow injuries, of which three were excluded from the study because fracture fixation was not performed at our service. Thus, 34 patients were assessed in this study, of which 20 (58.8%) were male and 14 (41.2%) were female. The mean age was 6.7 years, ranging from 6 months to 15 years, including 13 (38.2%) patients younger than 6 years, 17 (50%) aged 6–10 years, and the remaining older than 10 years (11.8%). The most affected side was the right side (18 cases, 53%).
Concerning the mechanism of trauma, all cases involved high-energy trauma, and a mechanism rarely described in the literature[9,10] stood out, in which injury was related to spin cycle rotatory injuries resulting from domestic accidents involving washer driers. Seventeen injuries (50%) resulted from rotational traumatic spin cycle from the washer, and the other 17 injuries resulted from typical trauma, of which 12 (35.2%) were caused by falls from height, two by falls from a motorcycle, two by a car accident, and one case resulted from a domestic accident in which a large animal ran over the patient. No accident due to a fall from a bicycle was reported.
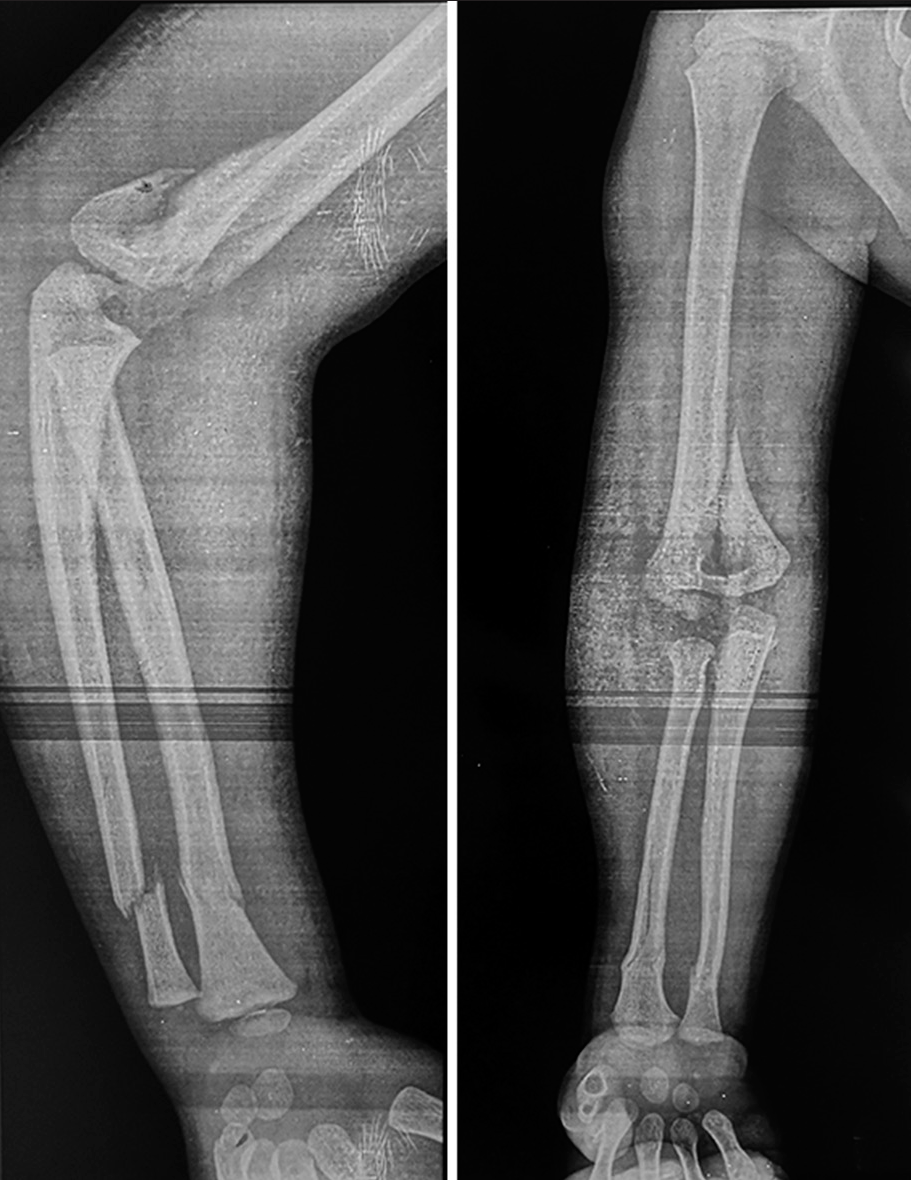
Regarding the site and type of fracture in each bone, there were 19 (55.8%) cases of diaphyseal fracture of the humerus. Twelve cases of supracondylar fractures of the humerus, of which six were classified as Gartland type III and six as Gartland II. Two cases of lateral condylar fractures of the humerus and one case of transverse fracture in the distal humerus with joint involvement [Figure 1]. Regarding the forearm, both bones were affected in 27 (79.4%) patients, and the ulna was not involved in only 7 (20.6%) patients. Most fractures of the radius (23 cases; 67.6%) occurred at the distal metaphysis, followed by 11 cases (32.4%) at the diaphysis. As for the ulna, diaphysis was affected in 14 patients, distal metaphysis in 12 patients, and a case of physeal injury with slipped epiphysis [Figure 2].
- Case 14. Longitudinal line with uncommon metaphyseal-epiphyseal involvement. Spin cycle rotatory injury.

- Case 11. Serious injury consisting of metaphyseal fracture of the radius and segmental ulnar fracture with physeal displacement of the distal ulna. Spin cycle rotatory injury.
Open fractures were reported in 8 cases (23.5%), of which six involved only the humerus and were classified as Gustilo IIIA, one case involved both sites, and one case involved the ulna and was classified as Gustilo I. Nine patients (26.5%) had associated injuries, including three cases of metacarpal injuries, two nervous injuries, one scapular fracture, one case of contralateral clavicular fracture, and one femoral fracture. One had multiple fractures of the pelvis and ipsilateral femur.
Concerning the treatments performed, 32 patients (94%) had a fixation on at least one bone and 24 patients (70.5%) had a fixation on both sites. Conservative treatment was chosen for both injuries in 2 cases (5.9%). When surgical treatment was chosen, the following procedures were carried out: As for the humerus, close reduction and percutaneous pinning in 15 cases (44.1%) and titanium elastic nailing in 13 (38.2%) cases, bridge plating in two cases, and cannulated screw fixation in one case. In relation to the forearm, 17 patients (50%) were treated with percutaneously inserted Kirschner wires, 10 (29.4%) were treated conservatively with cast immobilization, 6 patients (17.6%) underwent intramedullary elastic nailing, and one patient underwent fixation with DCP plate.
Complications [Table 2] occurred in 9 cases (26.5%), including 3 cases (8.8%) of compartment syndrome that was treated with urgent fasciotomy [Figure 3], 2 (5.9%) cases had limited range of motion, 2 (5.9%) had hardware protrusion, one had varus malunion, and one had nerve injury associated with the initial trauma. No implant-related infections were reported. Evaluating the complications, we saw that 100% of the compartment syndromes were related to the torsion trauma caused by the centrifuge machine. In addition, 66.6% of the complications were after the torsional trauma caused by the centrifuge.
| Type of morbidity | n | Percentage |
|---|---|---|
| Compartment syndrome | 3 | 8.8 |
| Limited flexion/extension | 1 | 2.9 |
| Varus malunion | 1 | 2.9 |
| Radial nerve injury | 1 | 2.9 |
| Neuropraxia | 1 | 2.9 |
| Implant protrusion | 2 | 5.9 |
| Loss of fixation | 1 | 2.9 |
| Synostosis | 2 | 5.9 |

- Case 26. Urgent wide fasciotomy.
Elbow function, as assessed according to MEPS criteria, was excellent in 17 patients (50%), good in 15 patients (44.1%), and average and poor in 1 patient (2.9%).[8]
DISCUSSION
Although some systematic reviews attempted to discredit the severity[5] of floating elbow injuries, we believe that these injuries should be taken very seriously since permanent complications are possible.[1,2,7] This premise is even more evident with traumatic spin cycle machine injuries, such as those reported in the present study, because nearly 20% of these injuries led to the development of compartment syndrome. Some case reports mentioned this new trauma mechanism,[9,10] and we found 17 similar consecutive cases showing that fracture lines and involvement of soft tissues were different from those observed in presentations typically found in falls from height.[5-7,11]
The incidence of floating elbow injuries is still low, and their treatment remains under discussion, especially when analyzing the need for fixation of both injuries,[12] only of humeral fracture,[13] or treatment based on fracture personality.[7-11] In this study, most patients underwent definite surgical treatment of at least one bone (94%) since fracture site stability facilitates the patient’s treatment, which reduces pain and discomfort that may result from prolonged immobilization. The differentiation between typical trauma and spin cycle machine trauma opens an opportunity for a new classification of floating elbow injuries since the fracture line produced by these novel injuries was not considered in the classification proposed by Ríos and Lucio in 2007.[14] The presence of compartment syndrome since the beginning worsens the prognosis of patients who suffer such severe trauma.
The typical fracture pattern of floating elbow injuries is a supracondylar fracture of the humerus accompanied by a fracture at the distal third of the forearm, which may involve the radius and the ulna, or only the radius resulting from elbow hyperextension and wrist dorsiflexion at the time of trauma following a fall from height.[1-5,7] We observed that the fracture pattern produced by the traumatic spin cycle rotation is a spiral-type line at the humerus and diaphyseal involvement at the forearm [Figure 4] due to the pronation/ supination movements performed by this part of the body. Percutaneous fixation of the supracondylar fracture and distal involvement of the forearm is preferred by numerous authors when the injury is caused by the classical mechanism.[1-4,12,13] We decided to perform intramedullary fixation of diaphyseal injuries of the forearm and placement of an elastic nail at the humerus to achieve fracture stabilization until union, with subsequent removal of the implant in all cases.

- (a and b) Case 2. Spin cycle rotatory injury. Atypical fracture pattern. Anteroposterior and profile views.
Some articles report a high percentage of excellent results regarding trauma-related functional outcomes.[12-15] In contrast, another article[11] obtained poor outcomes, which may be explained by the severity of the trauma reported by this article. Using MEPS criteria, more than 90% of outcomes were classified as excellent (50%) and good (44.1%) in the present study, which is infrequent in the outcomes of floating elbow injuries in adults, which show high rates of poor outcomes.[16,17]
Compartment syndrome is the most feared complication in cases of floating elbow injuries. To avoid this type of outcome, absolute indication for fracture fixation was recommended when floating elbow injuries were diagnosed in patients with a history of falls from height, and conservative treatment was set aside, especially in the case of supracondylar injuries of the humerus, so as to prevent fracture displacement.[6] This premise may be categorized as a “myth,” according to a systematic review conducted by Baghdadi.[5] However, we observed statistically significant values when a spin cycle traumatic mechanism caused the injury. The presence of complications in 26.5% of patients is coherent with similar previously published case series. Varus deviation and reduced range of motion were reported in our study. The most severe complication was the presence of radial nerve injury, which was related to trauma and not to the treatment performed.
Limitations and strengths
The main limitations of this study are its retrospective nature, single-center design, and small sample size, which hampered relevant comparisons. Comparison with other cases from the same region or countries with the same socioeconomic level could yield valuable results. The strength of this study is the description of cases resulting from sprain injuries, which allows for a better understanding of the overall management of patients with this infrequent entity.
CONCLUSION
Floating elbow injuries are rare, although serious injuries; traumatic spin cycle rotatory injuries further increase the complexity of treatment and the potential for complications. Numerous authors endorse the recommendation for surgical treatment. Early fixations may prevent compartment syndrome to help improve the swelling of soft tissues. However, the traumatic spin cycle rotatory mechanism causes injuries to soft tissues that may inevitably result in compartment syndrome.
ACKNOWLEDGMENT
The Board of AOtrauma LatinoAmerica, for its constant support.
ETHICAL APPROVAL
The study complied with ethical guidelines and principles and was approved by the institution’s Research Ethics Committee and the hospital’s General Directorate (June 06, 2022 Number: HT-06622-MG). This investigation was classified as harmless to humans.
AUTHORS’ CONTRIBUTIONS
ADNV conceived and designed the study, conducted research, provided research materials, and collected and organized data. ANF analyzed and interpreted data. ADNV wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the guardians have given their consent for the images and other clinical information to be reported in the journal. The guardians understand that the names and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Simultaneous ipsilateral fractures of the arm and forearm in children. Clin Orthop Relat Res. 1980;153:218-22.
- [CrossRef] [Google Scholar]
- The 'floating elbow' in children. Simultaneous supracondylar fractures of the humerus and of the forearm in the same upper limb. J Bone Joint Surg Br. 1995;77:791-6.
- [CrossRef] [PubMed] [Google Scholar]
- Supracondylar fractures of the humerus in children. Treatment by straight lateral traction. J Bone Joint Surg Br. 1986;68:577-83.
- [CrossRef] [PubMed] [Google Scholar]
- Closed reduction and percutaneous fixation of supracondylar fracture of the humerus and ipsilateral fracture of the forearm in children. J Bone Joint Surg Br. 2003;85:1169-72.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric floating elbow injuries are not as problematic as they were once thought to be: A systematic review. J Pediatr Orthop. 2020;40:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- Floating elbow in children: A descriptive study of 31 cases attended in a reference center for pediatric trauma. Rev Bras Ortop. 2011;46:500-4.
- [CrossRef] [PubMed] [Google Scholar]
- The elbow self-assessment score (ESAS): Development and validation of a new patient-reported outcome measurement tool for elbow disorders. Knee Surg Sports Traumatol Arthrosc. 2017;25:2230-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric floating elbow caused by a novel mechanism: A case report. Cureus. 2022;14:e29124.
- [CrossRef] [Google Scholar]
- Complex pediatric “spin dryer” injuries-an uncommon mechanism and pattern of synchronous upper limb fractures. Afr J Paediatr Surg. 2022;19:261-4.
- [Google Scholar]
- Paediatric floating elbow-a prospective study. J Clin Diagn Res. 2019;13:RC12-5.
- [CrossRef] [Google Scholar]
- Supracondylar fractures of the humerus associated with ipsilateral forearm fractures in children: A report of forty-seven cases. J Pediatr Orthop. 2001;21:307-12.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of ipsilateral supracondylar and forearm fractures in children. Injury. 1992;23:159-61.
- [CrossRef] [PubMed] [Google Scholar]
- A prognostic classification of the “floating elbow” in children. Acta Ortop Mex. 2007;21:300-3.
- [Google Scholar]
- Simultaneous ipsilateral pediatric fractures of the elbow and forearm attending a tertiary care hospital. JLMC. 2016;4:35-41.
- [CrossRef] [Google Scholar]
- Analysis of complications after a floating elbow injury. Eur J Orthop Surg Traumatol. 2017;27:607-15.
- [CrossRef] [PubMed] [Google Scholar]
- Floating elbow injuries in adults: Prognostic factors affecting clinical outcomes. J Shoulder Elbow Surg. 2013;22:74-80.
- [CrossRef] [PubMed] [Google Scholar]







