Translate this page into:
Hallux valgus: Surgical treatment with open proximal wedge osteotomy using low-profile plate — A case series
2 King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
Corresponding Author:
Ali A Alhandi
National Guard Hospital, King Abdulaziz Medical City, Po Box 22490, Riyadh 11426
Saudi Arabia
ali.alhandi@gmail.com
| How to cite this article: Alturki AA, Alassiri SS, Alsalman MJ, Afaleh AF, Alhelal FH, Alqahtani HM, Alhandi AA. Hallux valgus: Surgical treatment with open proximal wedge osteotomy using low-profile plate — A case series. J Musculoskelet Surg Res 2018;2:126-129 |
Abstract
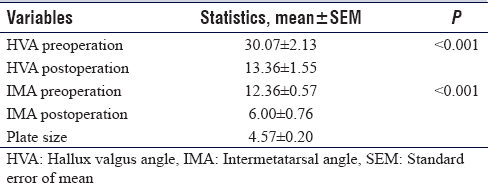
Objectives: Hallux valgus is one of the common causes of foot pain and deformity in the adult and adolescent population with multiple possible causes. Surgical correction with the opening proximal wedge osteotomy using low-profile plate system (LPS) fixation has been gaining popularity in the recent literature. This study report results from a case series of feet with hallux valgus corrected utilizing open proximal wedge osteotomy using LPS fixation. Methods: This was a retrospective case series of 12 consecutive patients (14 feet). All surgeries were done by a single orthopedic surgeon. A proximal wedge osteotomy using Arthrex opening wedge LPS fixation was done to all patients. Follow-up was 3 years minimum except for four patients who were lost to follow. Patient subjective satisfaction, radiographic assessment, and physical examination were reported. Results: The overall satisfaction was at 100% of followed patients. Shoe wear and foot shape were improved in 11 feet, and 12 had postoperative pain improvement. Mean preoperative hallux valgus angle (HVA) and intermetatarsal angle (IMA) were at 30.07° and 12.36°, respectively. Postoperatively, the mean HVA and IMA improved to 13.36° and 6°, respectively (P < 0.001). All followed patients showed complete healing. Conclusion: The opening proximal wedge osteotomy with a LPS fixation has a high overall satisfaction by patients and is preferred by surgeons, which stems from its straightforward technique, which makes the technique an attractive option for correcting the hallux valgus deformity.
Introduction
Hallux valgus is one of the common causes of foot pain and deformity in the adult and adolescent population. It is defined as a lateral deviation of the great toe with medial deviation of the first metatarsal bone.[1] The female-to-male ratio is 2:1 with a reported prevalence of 2%—4%.[2] Although it is not clear, possible causes may include footwear, namely high heel shoes that have a narrow toe box and genetic predisposition. Other causes of hallux valgus include rheumatoid arthritis, connective tissue disorders, and cerebral palsy.[3] Patients with hallux valgus mainly present with pain as the primary complaint. Nevertheless, complaints may include difficulty wearing specific footwear and undesirable appearance.
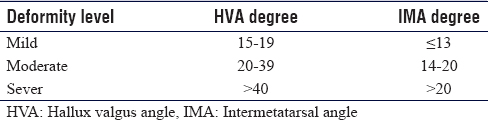
Hallux valgus is classified into mild, moderate, and severe [Table - 1]. Trethowan, in 1923, was the first to describe the proximal opening wedge osteotomy using the resected medial first metatarsal eminence as a structural autogenous bone graft.[4] In the literature, the use of the opening wedge osteotomy has been limited and reasonably objectionable due to its technical limitations and its potential complications. Moreover, the need for structural bone graft and the inability to achieve stable fixation resulting in fear of osteotomy fracture, malunion, or nonunion contributed to its limited use.[5]
In recent years, more studies have been published in the literature evaluating the opening proximal wedge osteotomy with low-profile plate system (LPS) fixation.[6],[7],[8],[9],[10],[11] Notably, a randomized controlled trial by Glazebrook et al. reported comparable radiographic and clinical results between the opening wedge with LPS fixation and proximal Chevron technique, with a subjective preference of surgeons to the opening wedge technique with LPS fixation citing its ease. The addition of the LPS provides stable fixation, which allows earlier return to weight-bearing status with functional rehabilitation, in contrast to standard proximal procedures, which require 6—8 weeks of strict nonweight-bearing recovery status.[11] A few cases have been reported with nonunion, malunion, symptomatic hardware, or hardware failure using LPS fixation.
This study aims to present the results of open proximal wedge osteotomy with LPS fixation for adult hallux valgus in terms of degree of correction both subjectively and radiologically, the rate of nonunion, malunion, infection, hardware failure, patient satisfaction, patient function, and reduction of pain.
Materials and Methods
After acquiring appropriate institutional review board approval, 12 consecutive patients (14 feet) were included in this retrospective case series. All underwent proximal wedge osteotomy with Arthrex Opening Wedge Low-Profile Plate and Screw System (LPS®) (Arthrex Inc., Germany) fixation. Surgery was performed by a single orthopedic surgeon from January 2014 to December 2015. All patients were assessed by an orthopedic board-certified physician, where detailed history and physical examinations were performed including demographic data, comorbidities (by history and from patient files), and medications. Data were collected using medical charts of the patients. Satisfaction rates were assessed subjectively using a home-made questionnaire. One musculoskeletal radiologist was involved in determining the correction objectively through radiological images. Patients with radiographic evidence of an abnormal hallux valgus angle (HVA) accompanied by a shape dissatisfaction and/or pain were included in the study. Exclusion criteria included patients who underwent any other correction of hallux valgus not using an LPS fixation, first metatarsophalangeal (MTP) joint arthritis, and hypermobility of tarsometatarsal joint or any other concomitant foot deformities.
Patient consent was obtained postsurgery to complete a questionnaire, which included demographic data, main complaint upon admission, pain scale (1—10 analog pain scale) before and after surgery, onset of pain related to walking (patients were measured in terms of time against their own preoperative reported result) or footwear, chronic pain, management, nonsurgical treatments pursued, conservative management, and perceived cosmetic appearance before and after surgery. The answers included yes, no, and other options as well as open-ended responses. Patients filled the questionnaires at their 6-week follow-up appointment (for bilateral patients, each foot was scored separately on the questionnaire) and again at their last follow-up visit. Follow-up was up to 3 years. Radiographic images were also taken at 6 weeks, 12 weeks, and finally, at the last follow-up. All analyses were conducted using Statistical Analysis System SAS® (SAS Institute Inc., released 2007, SAS for Windows, version 9.2, Cary, NC). A Student's t-test with a 95% confidence interval was used to compare pre- and postoperative angles, and P < 0.05 was considered significant in numerical variables (age, HVA-pre, HVA-post, intermetatarsal angle (IMA)-pre, and IMA-post) that were summarized and reported as means and standard deviations. Categorical variables (implant failure, healing problem, preoperative complaints, preoperative pain status, and postsurgical satisfaction) were summarized and reported in terms of frequency distribution.
Surgical technique
The operative technique consisted of an incision over the dorsal first web space, and the adductor tenotomy is performed as well as releasing part of the intermetatarsal ligament. A correction was achieved. Dorsomedial incision over the first MTP joint is made and digital nerves are identified and protected throughout the operation. After raising the flaps of the capsule, bunionectomy is done with taking a thin piece of bone from the metatarsal. Then, under the guidance of C-arm imaging, utilizing a dorsomedial approach, the tarsometatarsal joint is identified with a needle, and then, proximal metatarsal osteotomy is done 15 mm distal to the first tarsometatarsal joint. A gradual opening of the wedge is used until the desired angle is reached, which gave excellent correction of the IMA as well as a right place for the lateral sesamoid bone. Depending on the amount of correction, the size of the wedge is decided. Fixation is done with screws and a medially placed plate. Augmentation with an auto bone graft impacted into the wedge side is done. Finally, excellent correction of the IMA and HVA with a congruent MTP joint was achieved [Figure - 1]. Patients were allowed full weight-bearing immediately after surgery.
 |
| Figure 1: Preoperative (right) and postoperative (left) X-rays of hallux valgus deformity showing excellent alignment postoperatively |
Results
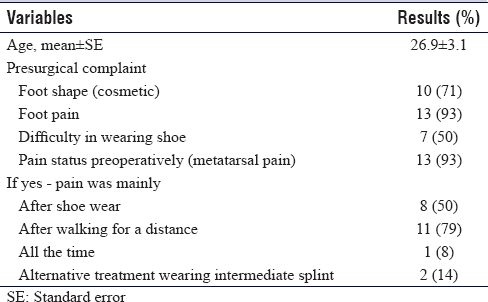
A total of 12 patients (14 feet) were reviewed who underwent open proximal wedge osteotomy using an LPS fixation. Nine patients underwent surgery on the right foot, one patient for the left foot, and two bilaterally. The average age was 26.86 years (range; 16—53 years). Preoperatively, nine patients (10 feet) complained of unsatisfactory foot appearance, 11 (13 feet) complained of foot pain, and 6 (7 feet) complained of difficulty in wearing shoes. [Table - 2] summarizes the preoperative status of the patients. Postoperatively at 6 weeks, 11 patients (11 feet) had improvement in shoe wear and 11 patients (12 feet) reported improvement of pain. In addition, 11 patients (11 feet) were satisfied with their foot shape and 10 patients also reported to be overall satisfied with the surgery. Four patients were lost to follow-up at the 3-year mark, with all remaining patients reporting to be still completely satisfied with their results.
[Table - 3] shows the clinical preoperative data for the 14 feet. At 6 weeks postoperatively, 4 feet had healing bone, and after 12 weeks, 7 more feet had healed bones. Two patients were lost to follow-up at 12 weeks (done at the end of 2015), and two more were lost to follow-up at the 3-year mark, resulting in an average follow-up of 26.4 months. All remaining patients had complete healing on radiographic images after 3 years with no changes noted in the angles measured. There was no implant failure noted in this study.
Discussion
This case series study demonstrated the clinical and radiological subjective and objective outcomes of 12 patients (14 feet) with hallux valgus, who underwent open proximal wedge osteotomy using an LPS fixation in a single center. Review of the literature showed that there was no ideal surgical technique described to treat hallux valgus; there were 150 different surgical techniques described in the literature.[4] Due to the technical limitations and its potential complications, the use of opening wedge osteotomy has been limited and reduced in the past.[5] However, the addition of LPS fixation has spiked the interest in the technique in recent literature.[6],[8],[9],[10]
This study showed a decrease of 48% and 43% in the mean IMA and HVA angles postoperatively, respectively. Compared to a study by Bagatur et al. that showed an IMA of 15° + 2.5° and an HVA of 29° + 6.4° preoperatively and dropped to IMA of 11° + 4.0° and HVA of 23° + 10.4° in the postoperatively, this study population shows better results although the sample size is smaller, which prevents a direct comparison.[12] Randhawa and Pepper found that the mean HVA and IMA decreased significantly in relation to the plate size. In patients who had 3.5-mm plate, the mean preoperative IMA was 13.8° (range: 6—18) and postoperative IMA was 5.8 (range: 3—8), with a mean correction of 8.0°. While in patients with 4.0 mm plate, the mean preoperative IMA was 16.9° (range: 11—30) and postoperative IMA was 8.9° (range: 4—11) with a mean correction of 9.0°. Patients with plate size of 5.0 mm had a mean preoperative IMA of 24.7° (range: 15—35) and postoperative IMA of 9.8° (range: 3—22) with a mean correction of 14.9°.[13] This study population had a mean plate size of 4.57 mm and a mean correction of the IMA and HVA of 6.4° and 16.7°, respectively. A randomized controlled trial by Glazebrook et al., in which they compared proximal wedge osteotomy and proximal Chevron osteotomy, concluded that proximal wedge osteotomy had better correction over the IMA, with a decrease from 14.8° + 3.2° to 9.1° + 2.9°, while the Chevron osteotomy had a decrease from 14.6° + 3.9° to 11.3° + 4.0°. Moreover, they have concluded that open wedge osteotomy is preferred by orthopedic surgeons for the fact that it is less technically demanding.[6]
The postoperative overall satisfaction in this study population is considered good; ten out of 12 patients were satisfied postoperatively at 6 weeks. At 3 years, four patients were lost to follow-up leaving eight total patients (10 feet). One of the unsatisfied patients reported complete satisfaction at 2 years, and the other was lost to follow-up. The technique has even better satisfaction results when plotted on larger sample sizes; Shurnas et al., who evaluated 78 patients (84 feet), showed that 70 patients (90%) noted good-to-excellent subjective satisfaction after the surgery.[9] There were no implant failures in this study population with all followed patients showing complete healing at the last follow-up, a recurring theme when plotted for larger sample size by Shurnas et al., is shown, which reported one case in their population that had nonunion, who underwent a Lapidus procedure in the revision surgery, adding to that there was no failure to the hardware used.[9] Furthermore, a study by Han et al. showed zero cases of nonunion when they compared oblique and straight osteotomies in the opening wedge technique.[14] Similarly, a study performed by Smith et al. reviewed 47 patients who underwent opening wedge osteotomy and reported 6 patients with hardware irritation, and 4 patients had nonunion or delayed union.[10] While in this study, the union rate seems high. The authors attribute that to the low number of patients included in the study.
Limitations and weaknesses
The small number of patients involved in the study and the retrospective nature of the study, which led to the lack of preoperative functional outcome measures.
Conclusion
This study shows a single surgeon experience with open proximal wedge osteotomy using a low-profile plate fixation resulting in high overall satisfaction and is proving to be an attractive option for patients seeking hallux valgus deformity correction. Moreover, significant improvement in the clinical and radiological parameters of patients who underwent surgery was noted in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AAA conceived the study and conducted research, SSA designed, collected data, involved in writing and proof reading the manuscript, MJA aided in determining angles on all x-rays and interpreted raw data, AFA and FHA were involved in data collection and analysis, HMA provided valuable support in data collection and management and logistic support, and finally AAA was involved in data analysis, manuscript writing, editing, and proof reading. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Coughlin MJ. Roger A. Mann award. Juvenile hallux valgus: Etiology and treatment. Foot Ankle Int 1995;16:682-97. [Google Scholar] |
| 2. | Okuda H, Juman S, Ueda A, Miki T, Shima M. Factors related to prevalence of hallux valgus in female university students: A cross-sectional study. J Epidemiol 2014;24:200-8. [Google Scholar] |
| 3. | Coughlin MJ, Jones CP. Hallux valgus: Demographics, etiology, and radiographic assessment. Foot Ankle Int 2007;28:759-77. [Google Scholar] |
| 4. | Trethowan L. Hallux valgus. In: Choyce C, editor. A System of Surgery. New York: P.B. Hoeber; 1923. p. 1046. [Google Scholar] |
| 5. | Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br 2005;87:1038-45. [Google Scholar] |
| 6. | Glazebrook M, Copithorne P, Boyd G, Daniels T, Lalonde KA, Francis P, et al. Proximal opening wedge osteotomy with wedge-plate fixation compared with proximal chevron osteotomy for the treatment of hallux valgus: A prospective, randomized study. J Bone Joint Surg Am 2014;96:1585-92. [Google Scholar] |
| 7. | Nery C, Réssio C, de Azevedo Santa Cruz G, de Oliveira RS, Chertman C. Proximal opening-wedge osteotomy of the first metatarsal for moderate and severe hallux valgus using low profile plates. Foot Ankle Surg 2013;19:276-82. [Google Scholar] |
| 8. | Saragas NP. Proximal opening-wedge osteotomy of the first metatarsal for hallux valgus using a low profile plate. Foot Ankle Int 2009;30:976-80. [Google Scholar] |
| 9. | Shurnas PS, Watson TS, Crislip TW. Proximal first metatarsal opening wedge osteotomy with a low profile plate. Foot Ankle Int 2009;30:865-72. [Google Scholar] |
| 10. | Smith WB, Hyer CF, DeCarbo WT, Berlet GC, Lee TH. Opening wedge osteotomies for correction of hallux valgus: A review of wedge plate fixation. Foot Ankle Spec 2009;2:277-82. [Google Scholar] |
| 11. | Wukich DK, Roussel AJ, Dial D. Opening wedge osteotomy of the first metatarsal base: A technique for correction of metatarsus primus varus using a new titanium opening wedge plate. Oper Techn Orthop 2006;16:76-81. [Google Scholar] |
| 12. | Bagatur AE, Albayrak M, Akman YE, Yalcinkaya M, Ozer UE, Yalcin MB, et al. A simple method for fixation of proximal opening-wedge osteotomy of the first metatarsal for correction of hallux valgus. Orthopedics 2016;39:e1213-7. [Google Scholar] |
| 13. | Randhawa S, Pepper D. Radiographic evaluation of hallux valgus treated with opening wedge osteotomy. Foot Ankle Int 2009;30:427-31. [Google Scholar] |
| 14. | Han SH, Park EH, Jo J, Koh YG, Lee JW, Choi WJ, et al. First metatarsal proximal opening wedge osteotomy for correction of hallux valgus deformity: Comparison of straight versus oblique osteotomy. Yonsei Med J 2015;56:744-52. [Google Scholar] |
Fulltext Views
2,504
PDF downloads
352





