Translate this page into:
Hemophilia-related radial head re-dislocation
2 Department of Orthopedics, King Fahad Hospital, Almadinah Almunawwarah, Saudi Arabia
3 Department of Orthopedics, College of Medicine, Taibah University, Almadinah Almunawwarah, Saudi Arabia
Corresponding Author:
Ibrahim M Alhumaidi
Department of Orthopedics, Prince Mohammed Bin Abdulaziz Hospital, Almadinah Almunawwarah
Saudi Arabia
dr.ibrahimalhumaidi@gmail.com
| How to cite this article: Alhumaidi IM, Taha WS, Abutalib RA, Alshabi YA, Almahdi HH, Mohammed BS. Hemophilia-related radial head re-dislocation. J Musculoskelet Surg Res 2020;4:52-55 |
Abstract
Surgical management of joint dislocation in a patient with hemophilia with an unremarkable medical history and a negative family history of hereditary diseases or hematological disorders is quite challenging. Due to its rare representation, the diagnosis can be delayed or even missed; therefore, frequent evaluations are necessary for early diagnosis and treatment. The treatment of such patients should be carried out on a comprehensive basis by a multidisciplinary team. No cases of joint dislocation secondary to hemophilia have been reported in the available English literature. In this report, we present a case of recurrent radial head dislocation following an open reduction and internal fixation of Monteggia fracture–dislocation in a patient with undiagnosed hemophilia. We describe its symptoms, signs, and investigations along with the surgical management. We present this case report and its management to increase the awareness of the possibility of this pathology and to avoid future misdiagnoses.Introduction
Monteggia fracture–dislocation is a fracture–dislocation of the proximal ulna that is associated with a disruption of the proximal radioulnar joint. It was originally described in 1814 by Monteggia.[1] Monteggia fracture–dislocation most commonly results from a fall on an outstretched hand with the forearm in hyperpronation position.[1] It accounts for approximately 2%–7% of all forearm fractures and 0.7% of all elbow dislocations in adult patients.[2]
When suspecting a forearm fracture and/or dislocation, radiographs are necessary. Anteroposterior and lateral views will usually pick up the injury. An additional oblique view may help in the classification, as well.[1]
In an adult, operative management is crucial for the management of most of these cases. The most common operative technique is an open reduction and internal fixation with a locked compression plate of the ulna placed dorsally with approximately three screws on each side of the fracture. The radial head dislocation usually reduces after the ulna fracture is realigned.[1],[2]
Hemophilia is a rare type of inherited coagulopathy characterized by the absence of factor VIII in hemophilia A and factor IX in hemophilia B. It is an X-linked recessive disease. However, some spontaneous mutations occasionally occur.[3],[4] The absence of these coagulation factors increases the susceptibility to have abnormal bleeding. Eighty percent of hemorrhages occur in the musculoskeletal system, while 20% occur in the central nervous system and other systems. Hemophilia is an interesting disorder to the orthopedic surgeons because of the high percentage of musculoskeletal involvement.[3],[4] Approximately 1/10,000 is the average prevalence of hemophilia worldwide.[3] The severity of this disorder is divided according to the presence of the coagulation factor in the blood: severe (<1%), moderate (1%–5%), and mild (>5%).[3]
Hemarthrosis, muscle hemorrhage, joint arthropathy, joint contracture and deformities, pseudotumors, and fractures are well known musculoskeletal manifestations of hemophilia.[3],[4],[5]
In this report, we present a case of recurrent radial head dislocations following open reduction and internal fixation of Monteggia fracture–dislocation in a patient with undiagnosed hemophilia. We could not find a similar case in the available English literature, so we report this case and its management to increase the awareness of the possibility of this pathology and avoiding misdiagnosis.
Case Report
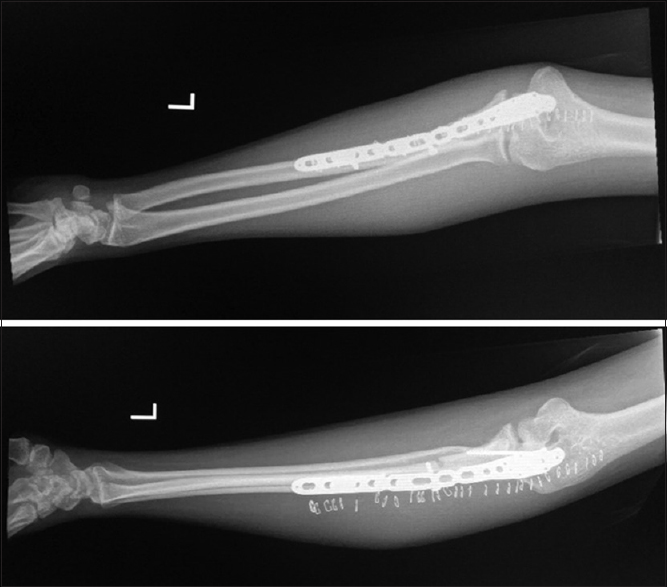
A 21-year-old male patient with an unremarkable medical history presented with left Monteggia closed fracture–dislocation after a road traffic accident [Figure - 1]. After the initial stabilization and preparation, the patient was taken to the operative room for an open reduction and internal fixation of the ulna fracture followed by closed reduction of the radial head dislocation and above elbow back slab application. Initial postoperative radiographs were satisfactory [Figure - 2], and the patient was discharged home on the 2nd day in a good state of health.
 |
| Figure 1: Initial radiographs of the elbow showing Monteggia fracture–dislocation |
 |
| Figure 2: Initial postoperative radiographs followed an open reduction and internal fixation of the ulna with close reduction of radial head |
Three weeks later, on the first follow-up visit, the patient was complaining of continuous elbow pain and swelling since the surgery. The pain was mainly in the lateral part of the elbow joint. There was no history of trauma or constitutional symptoms.
His local examination showed that the surgical scar was healing with no complications; there was a moderate swelling of the posterior and lateral parts of the left elbow with tenderness. Elbow motion was restricted. However, there were no signs of acute inflammation; the distal neurological examination was intact, and the distal pulse was palpable. Inflammatory markers were normal with a white blood cell count of 7.0 mcL, erythrocyte sedimentation rate of 32 mm/h, and C-reactive protein of 3 mg/L, and blood cultures were negative. The coagulation profile was showing isolated mild prolongation of activated partial thromboplastin time (aPTT) of 49.9 s; other parameters were within the normal range.
Radiographs showed a dislocated radial head with maintained fixation of proximal ulna fracture [Figure - 3].
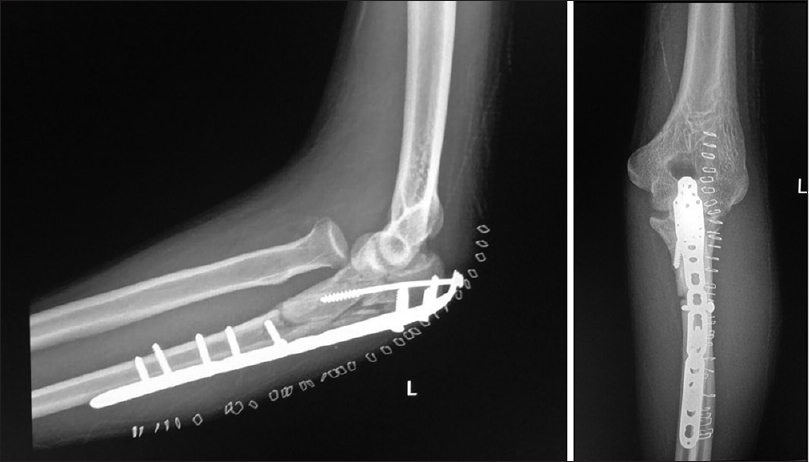 |
| Figure 3: Left elbow radiographs, three weeks postfixation showing radial head re-dislocation |
The patient was admitted and prepared for surgery the following day. The previous surgical wound was opened. There was a large hematoma subcutaneously and within the muscle layers. Evacuation of the hematoma was done, and closed reduction of the radial head was then easily achieved but was unstable and dislocating once the forearm was pronated. Further exploration showed no active bleeder, but a profuse oozing from the surrounding soft tissue was noted. Fluid samples were taken and sent for the culture and sensitivity analysis and proved negative later on. A hemostatic dressing (QuikClot Combat Gauze) was applied to the oozing surface, and the skin was approximated on top of the gauze. A second look surgery within 24–48 h was planned to inspect the wound and remove the gauze. On the second surgery, the compression gauze was removed; the oozing was less, and there were many small clots. The wound was irrigated at that time, and the skin was closed after drain application, which was removed after 48 h. The elbow was placed in a back slab with the forearm in supination to hold the radial head reduced.
Hematology team was consulted regarding the isolated mild prolongation of aPTT and the operative findings; the patient was fully examined and investigated from their side, and they recommended starting the patient on tranexamic acid 500 mg orally twice a day.
Later, on investigation, the results came out with aPTT of 49 s, prothrombin time of 13.1 s, international normalized ratio of 1.11, factor VIII level of 5%, factor IX level of 100%, factor XI level of 83%, and lupus anticoagulant being not detected. Tests for von Willebrand disease were unremarkable, and factor VIII inhibitor was negative. The patient's diagnosis with hemophilia A was proved, and the treatment was started accordingly for pre- and postoperation doses and intervals as per protocol.
In the meantime, the patient developed another collection in the wound around 1 week after the last surgery. The patient was then taken to the operating room after starting treatment and with a clearance of the hematology team. The wound was evacuated, the elbow was examined, and the radial head was found stable. Postoperatively, he was kept in a back slab with the forearm in supination for 4 weeks.
The patient remained in the hospital for a couple of days for pain control, wound inspection, and monitoring of the coagulation profile. The patient was discharged on a prophylactic coagulation factor VIII after a normal coagulation profile result and satisfactory radiographs [Figure - 4].
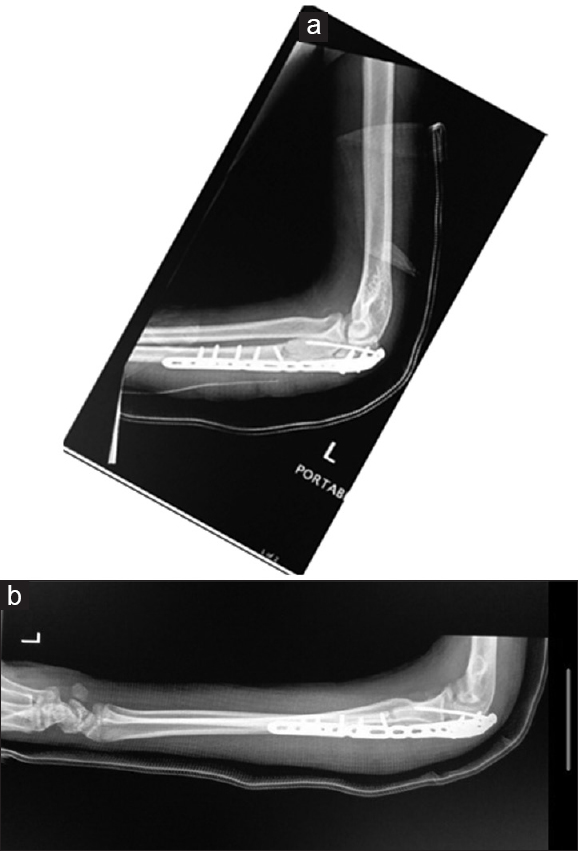 |
| Figure 4: (a and b) Radiographs postclose reduction of radial head and hematoma evacuation |
The patient underwent an uneventful follow-up for 1 year; the slab was removed at 4 weeks, and physiotherapy was started at 8 weeks. At a 1-year follow-up, the fracture was completely healed, and the patient had an almost full range of motion in the elbow with a functional supination/pronation [Figure - 5]. Radiologically, there were no signs of degenerative changes in the elbow joint [Figure - 6].
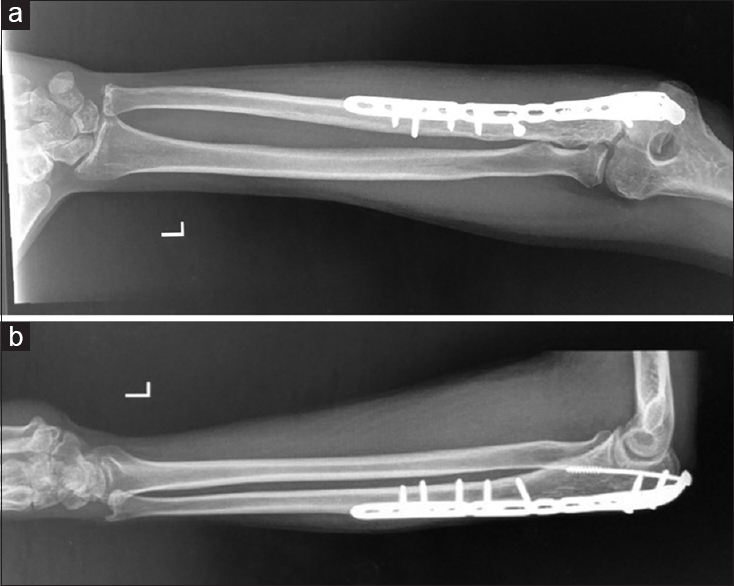 |
| Figure 5: (a and b) Left elbow radiographs, nine-month follow-up |
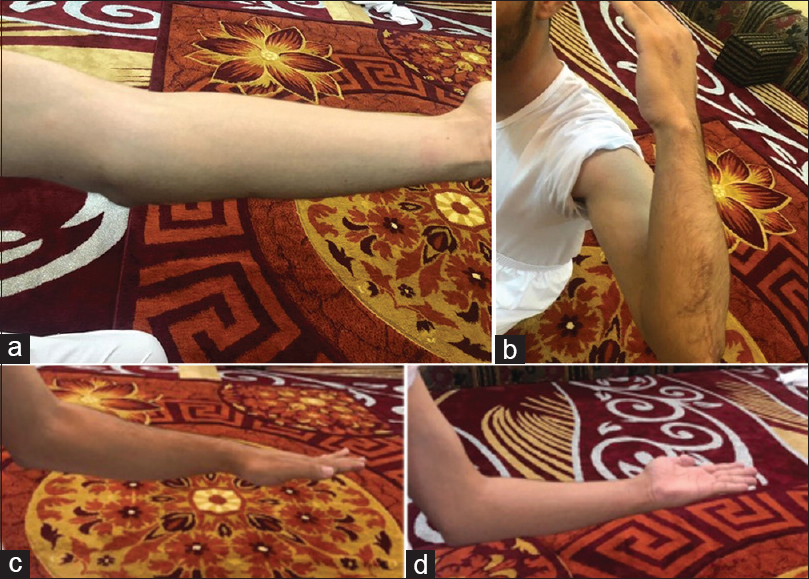 |
| Figure 6: (a-d) Elbow range of motion at five months postoperatively |
Discussion
The delay in the diagnosis of hemophilia as a possible cause for a recurrence of a traumatic dislocation might result in undesirable delay of the management. The reason behind this is due to its relatively rare occurrence, as demonstrated in our case. Many such patients have an unremarkable medical history, and a negative family history of hereditary diseases or hematological disorders, with no previous history of heavy or unusual bleeding. This, in turn, makes it difficult to diagnose, sequentially causing a potential delay in delivering proper management, as we faced in this case where recurrent dislocation happened as a result of the hematoma caused by the bleeding secondary to undiagnosed hemophilia. The initial laboratory tests were showed isolated mild prolongation of aPTT. However, this was not specific. The other laboratory and radiological tests excluded other key differentials such as infection, malalignment of the ulna, proximal radius fracture, and vascular injury; we had to look for another cause.
With previously diagnosed hemophilic individuals, surgeries can be performed smoothly with the improvement in the safety and the effectiveness of factor replacements therapy. Problems can be encountered with undiagnosed cases of mild and moderate hemophilia as in this case. In general, mild hemophilia is only diagnosed when an injury or medical intervention results in prolonged bleeding. Thereafter, the management of a patient may be relatively delayed as they do not usually experience spontaneous bleeds, which can result in a delay in the diagnosis of hemophilia.[6],[7]
Strauss et al. reported no significant difference regarding the length of preoperative hospital stay between patients with hemophilia and controls. Only patients with hemophilia who were operated at the distal lower extremity stayed significantly longer in the hospital than controls. Neither frequency nor duration of surgical drainage placement differed significantly between the two groups. The overall complication rate in both the groups was low without a statistically significant difference.[8]
Prolonged exposure of cartilage to blood causes cartilage damage, and bone remodeling occurs as the joint disease progresses. All of these will lead to degenerative arthritis, which is known as hemophilic arthropathy.[9],[10] Thus, the optimal management of musculoskeletal complications of hemophilia requires early prevention and treatment of acute bleeding episodes.
Studies showed that primary (early) prophylaxis is more effective than on-demand therapy regarding the prevention of arthropathy.[11],[12]
As early management of hemarthrosis is important to minimize joint damage, guidelines emphasize the importance of the prompt treatment of bleeding attacks, preferably within the first 24 h.[13]
We could not find a similar case in the available English literature. We present this case report and its management to increase the awareness of the surgeons if they face an unexplained profuse oozing during surgery, or there is an unexplained recurrence of a dislocation where the bone was reduced anatomically. This should arise the suspicion about the possibility of an undiagnosed form of mild hemophilia, and proper consultation, diagnosis, and replacement of the deficient coagulation factor should be considered.
We recommend avoiding overlooking abnormal coagulation profile results, even with the absence of personal and family history. The basic approach for patients with recent or previous bleeding tendencies required checking platelet counts and coagulation profile, and any abnormality in the results should be investigated accordingly. Hematology team consultation should be considered earlier in any case with an unexplained bleeding tendency that is not related to surgical site causes and in case of abnormal coagulation profile results.
Conclusion
The recognition and identification of hemophilia as a possible cause of joints recurrent dislocation after reduction can help to avoid undesirable delays in diagnosis and reduce hemophilia related joints complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Acknowledgment
The authors would like to thank Prof. Khalid I. Khoshhal, Pediatric Orthopedics, and Dr. Turki Alwasaidi, Hematology, for their assistance in the writing of this case report.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Author's contributions
HHA and BSM conceived and designed the study. HHA and IMA collected and organized data while IMA, YAA, WST, and RAA wrote the initial and final draft of the article and provided critical input. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
| 1. | Streubel PN, Pesántez RF. In: Diaphyseal fractures of the radius and ulna. Rockwood and Green's Fractures in Adults. 8th ed. Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, 3ed, McKee M, editors. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014;1:1139-67. [Google Scholar] |
| 2. | Siebenlist S, Buchholz A, Braun KF. Fractures of the proximal ulna: Current concepts in surgical management. EFORT Open Rev 2019;4:1-9. [Google Scholar] |
| 3. | Rodriguez-Merchan EC. Musculoskeletal complications of hemophilia. HSS J 2010;6:37-42. [Google Scholar] |
| 4. | Alhaosawi MM. Guidelines of management of musculoskeletal complications of hemophilia. J Appl Hematol 2014;5:75-85. [Google Scholar] |
| 5. | Rodriguez-Merchan EC. Musculo-skeletal manifestations of haemophilia. Blood Rev 2016;30:401-9. [Google Scholar] |
| 6. | Eyster ME, Gill FM, Blatt PM, Hilgartner MW, Ballard JO, Kinney TR. Central nervous system bleeding in hemophiliacs. Blood 1978;51:1179-88. [Google Scholar] |
| 7. | Small M, Steven MM, Freeman PA, Lowe GD, Belch JJ, Forbes CD, et al. Total knee arthroplasty in haemophilic arthritis. J Bone Joint Surg Br 1983;65:163-5. [Google Scholar] |
| 8. | Strauss AC, Pennekamp PH, Placzek R, Schmolders J, Friedrich MJ, Oldenburg J, et al. Perioperative management and outcome of fracture treatment in patients with haemophilia without inhibitors. Haemophilia 2016;22:e30-5. [Google Scholar] |
| 9. | Roosendaal G, Lafeber FP. Pathogenesis of haemophilic arthropathy. Haemophilia 2006;12 Suppl 3:117-21. [Google Scholar] |
| 10. | Valentino LA. Blood-induced joint disease: The pathophysiology of hemophilic arthropathy. J Thromb Haemost 2010;8:1895-902. [Google Scholar] |
| 11. | Gringeri A, Lundin B, von Mackensen S, Mantovani L, Mannucci PM, ESPRIT Study Group. A randomized clinical trial of prophylaxis in children with hemophilia A (the ESPRIT study). J Thromb Haemost 2011;9:700-10. [Google Scholar] |
| 12. | Manco-Johnson MJ, Abshire TC, Shapiro AD, Riske B, Hacker MR, Kilcoyne R, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med 2007;357:535-44. [Google Scholar] |
| 13. | Srivastava A, Brewer AK, Mauser-Bunschoten EP, Key NS, Kitchen S, Llinas A, et al. Guidelines for the management of hemophilia. Haemophilia 2013;19:e1-47. [Google Scholar] |
Fulltext Views
2,760
PDF downloads
1,425





