Translate this page into:
Iliopectineal line: A valuable radiological reference for spino-pelvic parameters
*Corresponding author: Abduljabbar Alhammoud, SUNY Upstate Medical University, Orthopedics Spine Surgery, Syracuse, New York, United States. aghammoud85@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Baco AM, Mukhter K, Moghamis I, Mehrab N, Alhabash MA, Abdalrahman MA, et al. Iliopectineal line: A valuable radiological reference for spino-pelvic parameters. J Musculoskelet Surg Res 2022;6:77-82.
Abstract
Objectives:
Spinopelvic parameters are crucial to address sagittal spinal imbalance; such measurements require standardized lateral radiographs that include spine and hips, which are neither always available, nor readily feasible intra-operatively. The aim of this study was to describe pelvic radiological reference points that could provide reliable sagittal balance estimates from conventional lumbosacral lateral radiographs.
Methods:
A descriptive, cross-sectional, radiological-based study was conducted. Readings were taken from institute’s digital radiology library, blinded to personal and clinical data. The correlation was made to conventional pelvic incidence (CPI), conventional pelvic tilt (CPT), and sacral slope (SS), measured for the same patients, and from the same standardized standing radiographs that included femoral heads.
Results:
Radiological images for 140 adult subjects, with suspected or established spine problems were studied. The average lumbar lordosis (LL) of 3 readers was 47 ± 13 (13–81) with an interclass agreement of 0.9, SS was 41 ± 9 with an interclass agreement of 0.9, CPI was 53 ± 10 with an interclass agreement of 0.8, CPT was 14 ± 8 with an interclass agreement of 0.9, iliopectineal inclination (IPI) of 4 readers was 64 ± 8 with an interclass agreement of 0.7 and iliopectineal tilt (IPT) was 24 ± 8 with an interclass agreement of 0.8 LL was with 6° of CPI and 16° of IPI. The CPI was equal to (CPI = SS + [CPT + 1.2]) and (IPI = SS + [IPT + 0.6]). The IPI was negatively correlated with CPI –0.2 P = 0.006, and IPI was negatively correlated with CPT –0.333 P < 0.001.
Conclusion:
Iliopectineal line provides reproducible readings, closer values to LL, and addresses the center of mass displacement.
Keywords
Deformity
Iliopectineal line
Lumbosacral spine
Sagittal balance
Spinopelvic parameters
INTRODUCTION
The contribution of the pelvis to the upright posture has been attributed to the backward rotation of the iliac bones; the upper pelvis, which together with the S-shaped spine curvature, brings the center of gravity closer to the hip joints.[1] This is in contrast to the lower pelvis, which is essentially that of quadrupeds.[2]
The study of spinopelvic measurements, namely the pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS), has been used as reliable indices to address the quality of posture, and clinically, the severity of the sagittal spinal imbalance to estimate the amount of lumbar lordosis (LL) targeted upon surgical correction.[3-7] The center of gravity of the trunk in the upright posture is anterior to the ninth thoracic vertebra, crosses the fifth lumbar vertebra and the posterior portion of the first sacral vertebra, to pass 3.5 cm posterior to the hip joints.[5] The sagittal balance can generally vary among asymptomatic adults, with the PI and SS decreasing as spinal balance becomes more negative.[7]
Those parameters have led many to derive formulae to address the required LL, using variables such as the kyphotic angle and “T9” tilt in 2006,[8] then, later on, a simple formula was described by Schwab et al. in 2009[9] as it depends on adding a fixed value to one variable; the PI.[10-12] Further works aimed to address the contribution of other factors caudal to the pelvis,[12-15] implying a role of the lower limbs in compensation to the sagittal spinal imbalance.
The iliopectineal line is an anatomic sacro-acetabular distance that starts in the sagittal plane from the posterior surface of the S1 vertebra, where it intersects the vector of the center of the gravity.[6] The formed angle with the center of gravity vector corresponds to the correction to the LL and provides a direct indicator for the position of the center of gravity vector relative to the hip, which can contribute more to the understanding of the variations in the sagittal alignment.[16]
This study aims to determine the consistency of the new radiological parameters (angles) using the iliopectineal line and to determine the correlation between the readings in our two “new” angles on one side, and the Conventional PI (CPI), PT, and SS, from the same films, on the other side. Furthermore, it aims to determine the presence of a relationship between measured angles and to determine the discrepancy between the “new” angle values and the estimated LL as per Schwab’s formula (LL = PI +9).
MATERIALS AND METHODS
A descriptive, cross-sectional, radiological-based study was conducted at a tertiary orthopedics’ spine department. The target population was spine clinic patients with “whole spine” radiographs taken for suspected/previously diagnosed mechanical/structural spine diseases; between January 2011 and 2019. Their images should be fulfilling the standardization criteria (Pre-operative, Lumbosacral lateral radiograph in upright (standing) position, including the hip and upper femur, with arms lying forward horizontally on a support “if needed”); and postoperative images were excluded.
Convenient sampling was used to stratify subjects according to the age group where those younger than 16 years old were excluded; thus, purposeful convenient sampling was used at this stage to ensure the presence of representative data for each age group, in 10 years’ intervals as follow (16–30 years, 31–40 years, 41–50 years, 51–60 years, and >61 years); simple random sampling was used then to allocate subjects.
The selection was “blinded” in terms of diagnosis, as well as both clinical and personal data of the studied subjects, except for the subject’s age and the hospital’s serial numbers, as the latter was used to prevent duplication of case selection.
The iliopectineal line was addressed as a radiological reference in the pelvis. It is described here as the most straight and cephalad portion of the arcuate line in the lateral pelvic view. It is measured from the anterior border of the S1 to the roof of the acetabulum, and that along with the horizontal line, and upper endplate of the first sacral vertebra, providing two angles, the iliopectineal inclination angle (IPI) and iliopectineal tilt (IPT), respectively [Figure 1]. These angles are more easily derived in this method.

- The red rectangular is showing the Anatomical demonstration of the iliopectineal line; drawn just anterior to the border of S1-S2, with angular measurements in relation to the imaginary horizontal line, and the superior border of S1.
A third angle that can be derived, though not a subject of study here, is by subtracting the iliopectineal angel from 90°; the complementary angle is effectively the inclination angle of the iliopectineal line from the vertical axis; the center of the gravity vector. As the iliopectineal represents the sacroacetabular distance, the distance between the hip and center of gravity can be calculated using this angle through simple trigonometrical calculations.
The conventionally measured PI, PT; named here CPI and conventional PT (CPT) respectively, in addition to the SS, and the LL were measured were compared to the newly proposed way as the following:
The angle between the iliopectineal and horizontal line (“IPI”), [Figure 2]
The angle between the iliopectineal line and the line drawn along the upper endplate of the first sacral vertebra (“IPT”); describing the upper sacrum position relative to the pelvis iliopectineal line, [Figure 2].
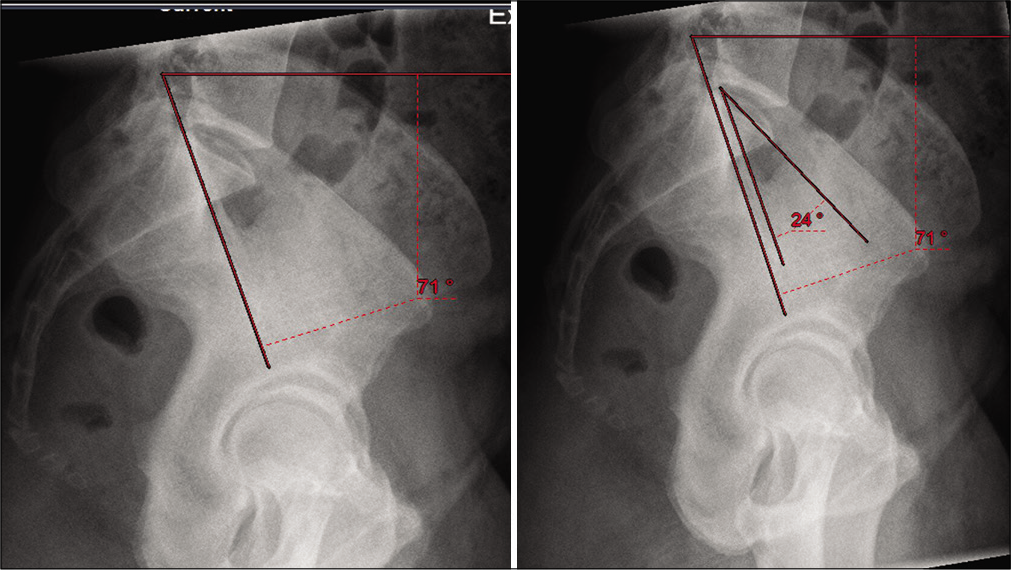
- Iliopectineal inclination angle and iliopectineal tilt.
Study subjects were retrieved from the digital database of Hamad General Hospital’s radiology department, utilizing Radiology Information System and Picture Archiving and Communications System, which support performing digital angle/metric measurements, as per the demonstration below.
Data entry was done independently by two orthopedic spine surgeons and a general orthopedic surgeon into a Microsoft Excel file, then transferred to Statistical Package for the Social Sciences (SPSS) version 20 software (SPSS Inc. Chicago, IL), where coding, computing, and analysis were done. Pearson correlations were taken as significant for P < 0.05, and a t-test was used to compare the differences in “mean” values, attributing test significance for the same P-values. Inter-rater reliability was used to check the consistency between the three readers.
RESULTS
We have reviewed standardized standing lumbosacral lateral view radiographs for 140 adults seen at our clinic for low back pain. Ages ranged between 16 and 87 years old, average 34 ± 17 years, with 45 males and 95 females. All the radiological measurements below showed no statistically significant difference for the gender and age groups [Table 1].
| n=140 | Age (years) | LL average | SS average | CPT average | CPI average | IPT average | IPI average |
|---|---|---|---|---|---|---|---|
| Mean | 33.7 | 47.5 | 41 | 14 | 53 | 24 | 64 |
| Median | 28 | 49 | 41 | 12 | 53 | 24 | 64 |
| Std. deviation | 17 | 13 | 9 | 8 | 10 | 8 | 8 |
| Minimum | 16 | 13 | 10 | 2 | 33 | 4 | 41 |
| Maximum | 87 | 81 | 60 | 38 | 79 | 45 | 85 |
LL: Lumbar lordosis, SS: Sacral slope, CPI: Conventional pelvic incidence, CPT: Conventional pelvic tilt, IPI: Iliopectneal incidence, IPT: Iliopectneal tilt
All radiological parameters were actually measured; however, the relationship between them can be mathematically represented as:
Pelvic incidence (CPI) = Sacral slope (SS)+ Pelvic tilt (CPT)
Iliopectineal inclination (IPI) = Sacral slope (SS) + Sacro-pelvic tilt (IPT).
That mathematical description shows SS coexisting as a shared variable for both.
LL and SS
The three readers’ average LL was 47° ± 13° (13–81.3°) with an interclass agreement of 0.9. LL was with 6° of CPI and 16° of IPI [Table 2]. The average of SS was 40.7° ± 8.9° with interclass agreement of 0.9. SS was equal to (SS = CPI[CPT–1.2]) and equal to (SS = IPI-[IPT–0.6]).
| Inter-rater reliability (consistency) (n=140, raters=3) | ||||||
|---|---|---|---|---|---|---|
| Cronbach’s Alpha (α) | LL | SS | CPI | CPT | IPI | IPT |
| 0.955 | 0.925 | 0.781 | 0.894 | 0.691 | 0.755 | |
| Rater (a) readings | 49±14 | 40±9 | 51±12 | 13±8 | 68±10 | 29±11 |
| Rater (b) readings | 45±13 | 40±10 | 54±11 | 14±8 | 65±9 | 26±10 |
| Rater (c) readings | 49±14 | 42±10 | 55±13 | 14±9 | 58±9* | 17±10 |
LL: Lumbar lordosis, SS: Sacral slope, CPI: Conventional pelvic incidence, CPT: Conventional pelvic tilt, IPI: Iliopectneal incidence, IPT: Iliopectneal tilt
Conventional measurements (CPT and PI)
The average CPI was 53° ± 10°, with an interclass agreement of 0.8. The CPI was equal to (CPI = SS + [CPT + 1.2]). The CPI was negatively correlated with IPI -0.2, P = 0.006 [Figure 3]
The average CPT was 14° ± 8°, with an interclass agreement of 0.9. The CPT was negatively correlated with IPT-0.3, P < 0.001.
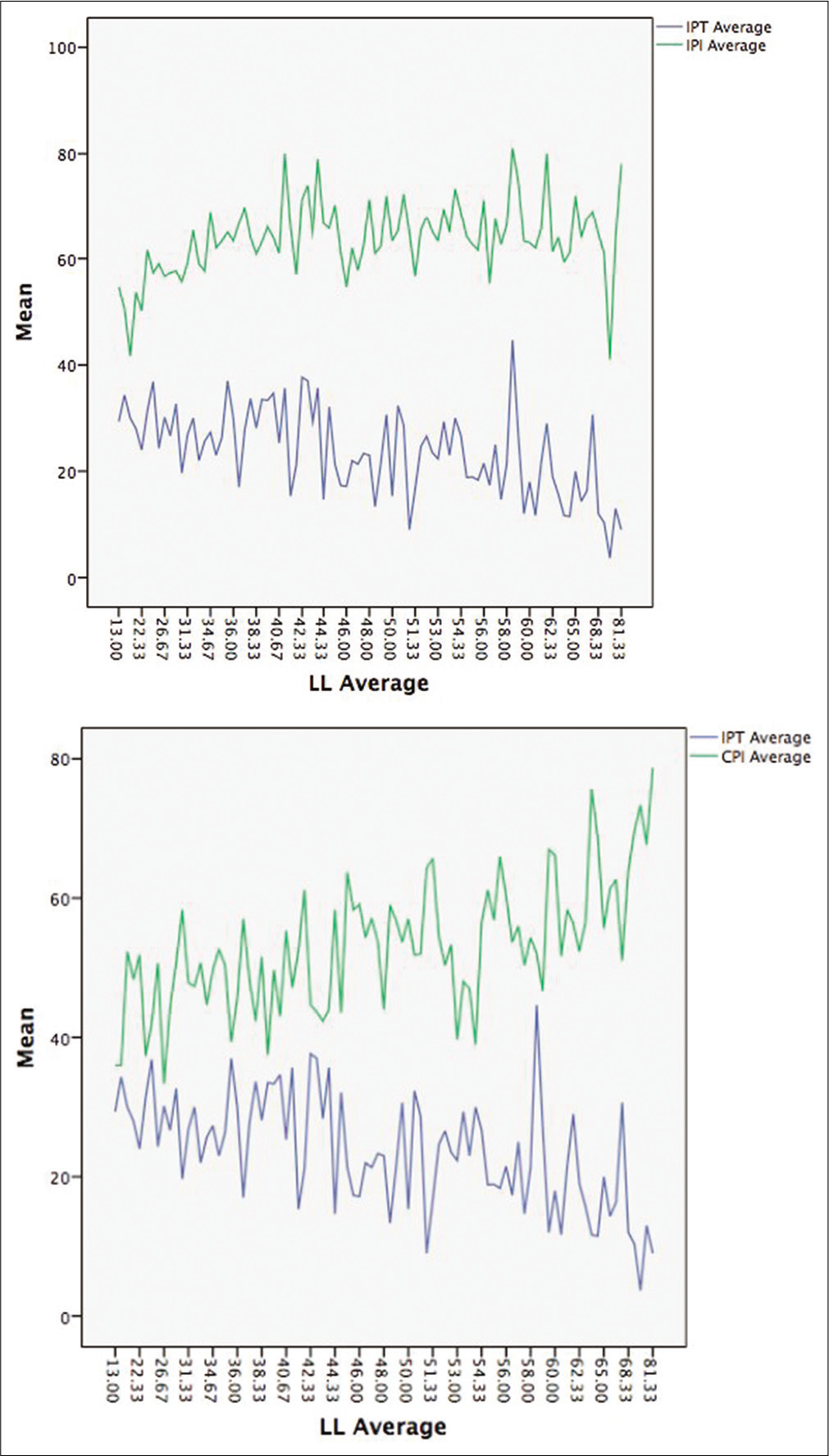
- Correlation lumbar lordosis, iliopectineal tilt and incidence.
The new measurements (IPT and PI)
The average IPI was 64° ± 8°, with an interclass agreement of 0.6. The IPI was equal to (IPI = SS + [IPT + 0.6]). The IPI was negatively correlated with CPI-0.2 P = 0.006
The average IPT was 24° ± 8°, with an interclass agreement of 0.8. The IPT was negatively correlating with CPT-0.3, P < 0.001.
DISCUSSION
By utilizing the iliopectineal line; a two-dimensional (line) mechanical conceptualization, with the advantage of direct estimation of the -horizontal- sagittal balance displacement relative to the femoral heads, while, for being within the pelvis, it allows accurate measurements for the orientation of the pelvis as one unit. Thus serving as the 3-dimensional pelvic vertebra proposed by Dubousset.[17] This may provide more input than the conventionally used one-dimensional (points) in the femoral head center, especially for assessment of the spine deformity in cases where hip pathology or lower limbs factors may contribute to the sagittal balance,[10] and a practical application for intra-operative fluoroscopy with short films.
Our new measurements seem to provide comparatively valid measurements for the estimated LL, independent of the lower limbs’ compensation for the posture, as evident by the degree of correlation between the conventional and proposed angels. The lesser values of interclass agreement arose due to lack of familiarity with the new method, in addition to the lack of agreement on “which line” or “portion of the line” is to be used; as the sample included cases with severe deformity; two iliopectineal lines appeared on some radiographs. Eventually, we agreed to recommend the lower line in such cases, as it can be traced from the anterior surface of S1.
Despite the diversity of our sample in terms of age and spine pathology status, the radiological parameters seem to provide sound estimates, given the fairly normal distribution and the small standard error of the mean.
We advocate that the iliopectineal line, being easily identified as a two-dimensional anatomical landmark and practically used as a radiological reference in daily practice, can provide comparably valid and reliable readings to the point-based conventional PI and tilt, and does not necessitate repeating exposure for long films views. Theoretically, the IPI can be treated as an additional Kyphotic curve, in comparison to, and almost equal in magnitude (curvature) to the LL in “normal” upright posture. Moreover, considering the triangle formed by the sagittal vertical axis (SVA), the horizontal distance of the SVA from the femoral heads, and the iliopectineal line; we find that “the cosine of IPI” represents the relationship of the horizontal distance of the SVA from the femoral head to the “length” of iliopectineal line; [Supplements: Figure 4] with the latter almost vary to a negligible degree while maintaining the sagittal balance. This implies that IPI angle changes in dynamic flexion/extension views will be proportional to the horizontal SVA displacement; and hence can be used indirectly to estimate the overall posture.
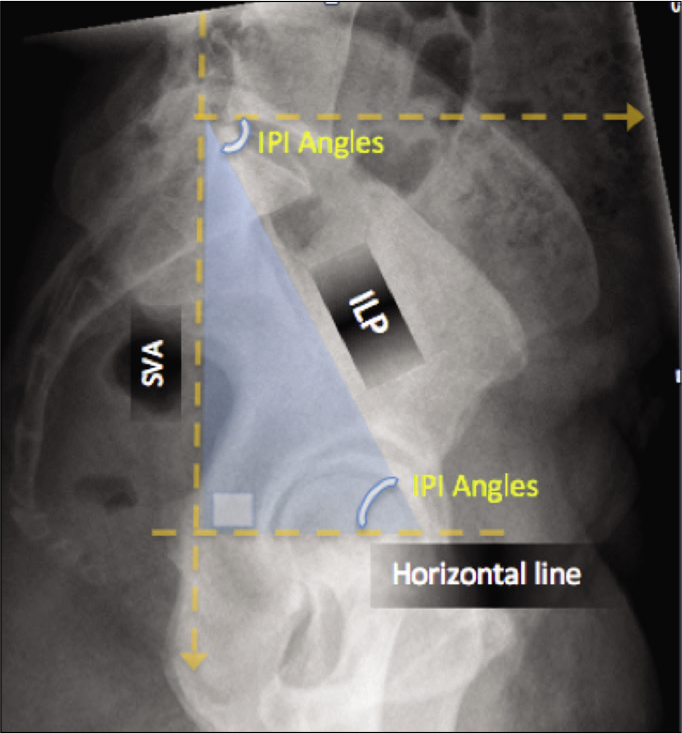
- Represent the triangle formed by the sagittal vertical axis (SVA), the horizontal distance of the SVA from the femoral heads, and the iliopectineal line; we find that “the cosine of Iliopectineal inclination angle” represents the relationship of the horizontal distance of the SVA from the femoral head to the “length” of iliopectineal line. Thus, the larger the angle, the less (shorter) horizontal displacement.
LIMITATIONS
The limitations of this study are the retrospective nature, it is only a radiological evaluation, it has a small sample size, and there was no matched age group.
CONCLUSION
Iliopectineal line, being an anatomical sacro-acetabulum distance and more related to the center of the gravity vector, provides a practical and reproducible radiological reference point (line) for the spinopelvic parameters. In addition, its relationship to the horizontal line and upper endplate of the first sacral vertebra provide comparative readings to the PI and tilt, respectively, without the need for the center of the femoral head. Our study found an excellent inter-reliability results and further studies are needed for accurate clinical implications.
AUTHORS’ CONTRIBUTIONS
ABB, conceived the idea, IM, NM, MA, MAA, KM, AA collected and organized the data, AA, KM, and IM wrote the manuscript, and AB revised and provided critical input. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
ETHICAL APPROVAL
This study was approved by the Medical Research Center at Hamad medical corporation, Doha, Qatar. IRB protocol approval number is: 15136/15, granted on June 8th, 2015.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
There is no conflict of interest.
References
- Primate Functional Morphology and Evolution. 1975. De Gruyter Mouton. Available from: https://www.degruyter.com/view/title/5056 [Last accessed on 2021 Feb 22]
- [CrossRef] [Google Scholar]
- The position of the human pelvis in the vertebrate series. Arch Frauenk Konstitutionsforsch. 1929;15:215-61.
- [Google Scholar]
- Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: A literature review. Int Orthop. 2015;39:87-95.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic incidence-lumbar lordosis mismatch results in increased segmental joint loads in the unfused and fused lumbar spine. Eur Spine J. 2014;23:1384-93.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103.
- [CrossRef] [PubMed] [Google Scholar]
- Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop. 1987;11:261-9.
- [CrossRef] [PubMed] [Google Scholar]
- Equilibre sagittal du rachis. Relations entre bassin et courbures rachidiennes sagittales en position debout. Rachis. 1993;5:215-26.
- [Google Scholar]
- Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976). 2011;36:E1648-54.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal alignment of spine and pelvis regulated by pelvic incidence: Standard values and prediction of lordosis. Eur Spine J. 2006;15:415-22.
- [CrossRef] [PubMed] [Google Scholar]
- Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34:1828-33.
- [CrossRef] [PubMed] [Google Scholar]
- Global analysis of sagittal spinal alignment in major deformities: Correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J. 2011;20(Suppl 5):681-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pelvic parameters: Origin and significance. Eur Spine J. 2011;20(Suppl 5):564-71.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of pelvic rotation on pelvic incidence, pelvic tilt, and sacral slope. Spine (Phila Pa 1976). 2014;39:E1276-83.
- [CrossRef] [PubMed] [Google Scholar]
- Gravitational forces and sagittal shape of the spine. Clinical estimation of their relations. Int Orthop. 2008;32:809-16.
- [CrossRef] [PubMed] [Google Scholar]
- Increased pelvic incidence may lead to arthritis and sagittal orientation of the facet joints at the lower lumbar spine. BMC Med Imaging. 2013;13:34.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30:346-53.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional analysis of the scoliotic deformity In: Weinstein SL, ed. The Pediatric Spine: Principles and Practice. New York: Raven Press Ltd.; 1994. p. :479-96.
- [Google Scholar]






