Translate this page into:
Internal fixation of scapular body fractures: Short-term results of a prospective study
2 Department of Orthopedic Surgery, Nasser Institute for Research and Treatment, Cairo, Egypt
Corresponding Author:
Ahmed Afifi
Department of Orthopedic Surgery, Faculty of Medicine, Cairo University, Cairo
Egypt
ahmedafifi@kasralainy.edu.eg
| How to cite this article: Afifi A, Khaled I. Internal fixation of scapular body fractures: Short-term results of a prospective study. J Musculoskelet Surg Res 2020;4:194-198 |
Abstract
Objectives: Most scapular body fractures can be treated conservatively with good-healing capacity. Indications of surgical treatment of these fractures are often debatable. The purpose of this study was to evaluate the short-term results of open reduction and internal fixation of displaced scapular body fractures. Methods: This prospective case series was conducted between 2016 and 2019. It included 10 male patients with displaced scapular body fractures treated with open reduction and internal fixation using Judet approach. Their mean age was 35.9 years (range, 18–60). The mean follow-up period was 16 months (range, 12–18). Patients were assessed radiologically for union and functionally using the Disabilities of the Arm, Shoulder, and Hand (DASH) score. Results: Union was achieved in all patients at a mean of 11.3 weeks (range, 8–14). The mean DASH score in the 12th month after the surgery was 30.8 (range, 26.7–36.7). Conclusions: Internal fixation of scapular body fractures gives good functional outcomes with a low complication rate.
Introduction
Scapular body fractures constitute 50% of all scapular fractures.[1] These fractures are uncommon as the scapula is surrounded by good musculature conferring protection making fractures less likely.[2]
Scapular body fractures are mostly due to high energy trauma. They are usually associated with chest, cervical spine, head injuries, or other fractures, with a mortality rate reaching up to 10%–15%. These fractures may be missed during the initial examination while resuscitating the associated life-threatening severe injuries.[2],[3]
Most scapular body fractures can be managed conservatively with good healing due to rich blood supply from the surrounding muscles.[4],[5] However, shoulder function may be reduced after conservative treatment of markedly displaced fractures with chronic pain in 12% of patients and radiographic scapular deformity in 25% of patients.[6],[7],[8],[9],[10],[11],[12]
The indications of operative management are often debatable.[2] However, with improved surgical techniques and availability of better implants, there was more interest and enthusiasm toward the internal fixation of markedly displaced scapular fractures.[13]
Prospective studies regarding the internal fixation of scapular body fractures are deficient in the literature. Many studies are retrospective and/or discussing all scapular fractures, not specifically body fractures. Our purpose was to assess the short-term outcome of internal fixation of displaced scapular body fractures regarding union and shoulder function.
Patients and Methods
This prospective study was conducted between January 2016 and June 2019 after the approval of our ethical committee. Ten males with scapular body fractures were included, with a mean age of 35.9 years (range, 18–60). The dominant side was affected in 40% of cases. We included patients with markedly displaced extra-articular scapular body fractures according to the following criteria: (1) Glenopolar angle (GPA) ≤22° and/or (2) more than 20 mm lateral displacement of the distal scapular body fragment compared to the proximal fragment on a three-dimensional computed tomography (3D-CT) scan, and/or (3) angulation more than 45° between the proximal and distal main fragments of the scapular body (measured in 3D-CT simulating scapular Y view) and/or (4) translation with no apposition of the proximal and distal main body fragments (measured in 3D-CT simulating scapular Y view). Patients with an associated head injury, other fractures in the same limb, and/or any previous shoulder pathology were excluded.
Seven fractures were class 14B1 (scapular body fracture that exits the body at 2 points or less), and three fractures were class 14B2 (scapular body fracture that exits the body at 3 points or more) according to the revised Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association classification system.[14] Regarding the mode of trauma, six fractures were due to motor car accidents (60%), three fractures were due to motorbike accidents (30%), and one fracture was due to a fall of a heavy object over the shoulder (10%). Surgery was performed after a mean of 2.3 days following trauma (range, 2–3). All patients had preoperative anteroposterior and scapular lateral (Y) radiographs and a CT scan with 3-D reconstructions (3D-CT scan). All measurements were made on 3D-CT images.
Operative technique
Surgery was performed under general anesthesia in the lateral decubitus position. Judet approach was used in all cases.[15]
The skin incision was made following the posterolateral lip of acromion extending along the spine of the scapula, then turning inferiorly along the medial border of the scapula [Figure - 1]. Superficial dissection was performed, and then the deltoid muscle was detached sharply from the spine of the scapula. Lateral traction of the detached deltoid was enhanced through a stay-suture in the most medial part of the muscle [Figure - 2]. Then, the internervous plane between infraspinatus (suprascapular nerve) and teres minor (axillary nerve) was developed. The infraspinatus muscle was entirely elevated from medial to lateral to expose the infraspinous fossa up to the glenoid neck [Figure - 3]. The fracture was exposed, and the hematoma was cleared off bone fragments. Fracture reduction began with the lateral border of the scapula. A careful reduction was made, and fixation was performed using locked 3.5 mm titanium reconstruction plates. The plates were contoured before their application to match the scapula's curvature after being reduced [Figure - 4]. Screws were carefully inserted to avoid pleural or pulmonary injury. Infraspinatus and deltoid muscles were reattached after fixation, and the wound was closed in layers over a drain.
 |
| Figure 1: Skin incision |
 |
| Figure 2: Stay-suture in the detached deltoid muscle |
 |
| Figure 3: Muscle elevation from the scapula to allow fracture exposure |
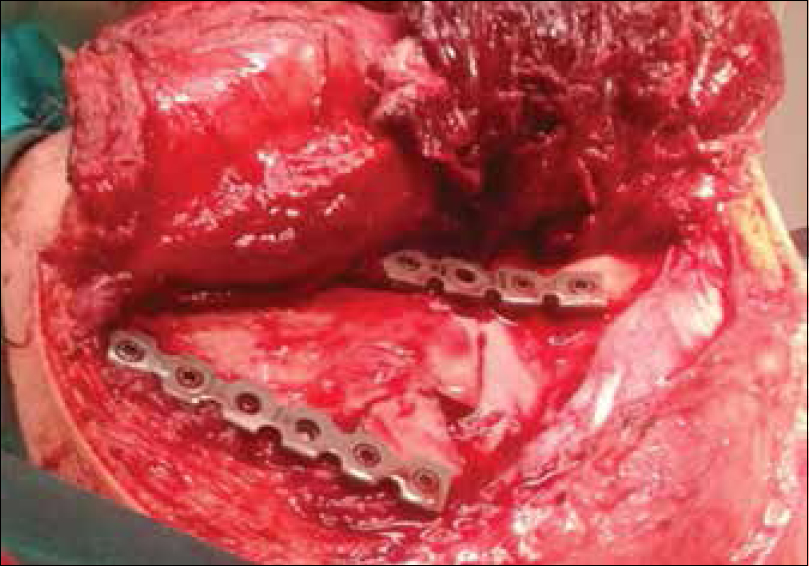 |
| Figure 4: Fixation was done using contoured 3.5 mm reconstruction plates |
The shoulder was immobilized in a sling for 3 weeks after the surgery with no restriction of hand, wrist, or elbow motion. Passive shoulder motion was allowed 2 weeks after the surgery and continued till 6 weeks. Then, active shoulder motion and muscle-strengthening exercises were started. Patients were clinically, radiologically, and functionally followed-up using the Disabilities of the Arm, Shoulder, and Hand (DASH) score (the Arabic version).[16]
Results
A total of 16 patients with scapular body fractures were assessed for eligibility; 4 patients did not meet the inclusion criteria, and 2 patients refused to participate in the study. Only 10 male patients met the inclusion criteria and were enrolled after their acceptance. The mean preoperative measurements are listed in [Table - 1]. No patient was lost at the final follow-up period. The mean follow-up period was 16 months (range, 12–18). The mean operative time was 2.25 h (range, 2–3). The mean intra-operative blood loss was 239.5 cc (range, 200–400). Two reconstruction plates were used in all patients (one at the lateral scapular border, which is the key structure for fracture reduction and fixation, and the other plate at the medial border). In 3 patients, the medial plate was contoured and placed along the medial border and the inferior surface of the scapula's spine. Union was defined as bony consolidation of the fracture lines in follow-up CT scans. All patients achieved union at a mean of 11.3 weeks (range, 8–14). Patients returned to their activities at a mean of 4.6 months (range, 3–6). The mean DASH score in the 12th month after the surgery was 30.8 (range, 26.7–36.7). All patients had an intact postoperative neurovascular state. One patient developed superficial wound infection 1 week after surgery, and immediate debridement was done together with antibiotic therapy for 2 weeks, and the infection resolved. Eight patients regained full shoulder range of motion, whereas 2 patients had mild limitation of shoulder external rotation (−10°, −15°). Hardware removal was not needed in any patient. No other complications were encountered [Table - 2]. [Figure - 5] shows a case example of a scapular body fracture.


 |
| Figure 5: (a and b) Preoperative radiograph and three-dimensional computed tomography scan of a case of a scapular body fracture, (c) postoperative radiograph showing internal fixation with 2 reconstruction plates, (d) clinical photo showing full shoulder abduction |
Discussion
In this prospective study, the results are encouraging. Union was achieved in all patients at a mean of 11.3 weeks, and full shoulder range of motion was regained in 80% of patients. Only two patients had a mild limitation of shoulder external rotation. The mean DASH score after 1 year was 30.8. Only one patient had a wound infection, which resolved after debridement and antibiotic therapy. No other complications were encountered. Judet approach, despite being an extensive approach, was used in this study as it gives excellent exposure to the scapular body, allowing better fracture visualization, reduction, and fixation. Modified and minimally invasive approaches require advanced surgeon's experience in internal fixation of scapular fractures. These approaches are less extensive than the classic Judet approach, and comparative studies may be needed to compare the effect of the approach on the functional outcomes.
The aim of fixation of scapular body fractures is to regain the anatomical relationship between the scapular body and the glenoid, and congruency between the scapular body and chest wall, allowing comfortable scapulothoracic motion.[11]
Although most scapular body fractures used to be treated nonoperatively, there has been a recent trend toward surgical management of displaced fractures with debatable indications.[11],[17],[18],[19],[20]
Studies that discuss the decision-making and management of scapular fractures are largely retrospective.[11],[12],[19],[20] There is a lack of prospective studies comparing the outcome of conservative and operative treatment of scapular fractures with little data about the specific characteristics of scapular fracture that necessitates operative treatment.[17] Nordqvist and Petersson had a study on 22 patients with scapular body fractures and concluded that conservative management of these fractures does not always lead to satisfactory functional outcomes.[7] Zlowodzki et al. reported in their systematic review of 520 scapular fractures in 22 retrospective case series that 135 out of 137 isolated scapula body fractures (99%) were managed conservatively with good or excellent results in 86% of cases. However, a proper comparison between surgical and conservative management could not be established in their review.[4] Schofer et al. reported the outcome of conservative treatment of scapular fractures in 50 patients and concluded that there was a significant difference in the constant score and shoulder range of motion when compared to the uninjured shoulder.[21]
Jones and Sietsema retrospectively reviewed 31 operatively treated patients with scapular fractures in comparison to 31 patients treated conservatively. Although the two groups were heterogeneous regarding the fracture characteristics, the outcome was good and comparable in both groups.[22] Dimitroulias et al. prospectively studied the results of nonsurgical management in 32 out of 49 patients with displaced scapular body fractures and obtained satisfactory outcomes.[23]
Kannan etal. reported in their systematic review the results of management of 97 scapular body fractures in 3 studies; 75 patients were managed conservatively, and 22 patients were managed with internal fixation. They concluded that there was no significant difference between surgical and conservative management (P = 0.28). However, they stated that fractures with 100% translation at the lateral scapular border and/or medialization of the glenohumeral joint >15 mm, are indicated for surgery.[24]
Based on the previously mentioned data, the authors hypothesized that restoration of the anatomical relationship between the scapular body and the glenoid would help regain the preinjury shoulder and scapulothoracic function. The key step was re-alignment and rigid fixation of the lateral scapular border.
An important weak point of this study is the absence of a control group. Thus, we could not provide strong evidence that surgical intervention leads to a better outcome. Other drawbacks are the limited number of patients and the lack of radiographic correlation with functional scores. Furthermore, the DASH score is not the best score for the evaluation of shoulder, and scapulothoracic function, and more specific scores should be used.
Conclusions
Internal fixation of scapular body fractures gives good outcomes regarding union and shoulder function with a low complication rate.
Recommendations
We recommend increasing the sample size together with a longer follow-up period. A control group is needed to compare the outcome of internal fixation to that of conservative treatment. Furthermore, the decision of surgical management of these fractures should not be taken easily and should be conferred only to markedly displaced fractures based on the GPA measurement, the degree of lateral displacement, angulation and/or translation.
Ethical consideration
This study was approved by the ethical committee of our institution on November 15th, 2015 with the serial number 385. The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or notforprofit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
AA conceived and designed the study, conducted research, provided and organized data. IK collected, analyzed, and interpreted data. IK provided research material and logistic support. AA reviewed the literature and wrote the initial and final drafts of the article. All authors contributed to clinical studies, data acquisition, data analysis, statistical analysis, manuscript preparation, and manuscript editing. All authors have critically revised and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Tuček M, Chochola A, Klika D, Bartoníček J. Epidemiology of scapular fractures. Acta Orthop Belg 2017;83:8-15. [Google Scholar] |
| 2. | Noguchi T, Mautner JF, Duncan SF. Dorsal plate fixation of scapular fracture. J Hand Surg Am 2017;42:843.e1-843.e5. [Google Scholar] |
| 3. | Lapner PC, Uhthoff HK, Papp S. Scapula fractures. Orthop Clin North Am 2008;39:459-74. [Google Scholar] |
| 4. | Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: Systematic review of 520 fractures in 22 case series. J Orthop Trauma 2006;20:230-3. [Google Scholar] |
| 5. | Gosens T, Speigner B, Minekus J. Fracture of the scapular body: Functional outcome after conservative treatment. J Shoulder Elbow Surg 2009;18:443-8. [Google Scholar] |
| 6. | Ada JR, Miller ME. Scapular fractures. Analysis of 113 cases. Clin Orthop Relat Res 1991;269:174-80. [Google Scholar] |
| 7. | Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res 1992;283:139-44. [Google Scholar] |
| 8. | Romero J, Schai P, Imhoff AB. Scapular neck fracture-the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg 2001;121:313-6. [Google Scholar] |
| 9. | Haraguchi N, Toga H, Sekiguchi Y, Kato F. Corrective osteotomy for malunited fracture of the glenoid cavity: A case report. Clin Orthop Relat Res 2002;404:269-74. [Google Scholar] |
| 10. | Bozkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Başbozkurt M. Conservative treatment of scapular neck fracture: The effect of stability and glenopolar angle on clinical outcome. Injury 2005;36:1176-81. [Google Scholar] |
| 11. | Bartoníček J, Frič V. Scapular body fractures: Results of operative treatment. Int Orthop 2011;35:747-53. [Google Scholar] |
| 12. | Cole PA, Talbot M, Schroder LK, Anavian J. Extra-articular malunions of the scapula: A comparison of functional outcome before and after reconstruction. J Orthop Trauma 2011;25:649-56. [Google Scholar] |
| 13. | Cole PA, Freeman G, Dubin JR. Scapula fractures. Curr Rev Musculoskelet Med 2013;6:79-87. [Google Scholar] |
| 14. | Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018 J Orthop Trauma 2018;32 Suppl 1:S1-170. [Google Scholar] |
| 15. | Cole PA, Dubin JR, Freeman G. Operative techniques in the management of scapular fractures. Orthop Clin North Am 2013;44:331-43, viii. [Google Scholar] |
| 16. | Alotaibi NM, Aljadi SH, Alrowayeh HN. Reliability, validity and responsiveness of the Arabic version of the Disability of Arm, Shoulder and Hand (DASH-Arabic). Disabil Rehabil 2016;38:2469-78. [Google Scholar] |
| 17. | Schroder LK, Gauger EM, Gilbertson JA, Cole PA. Functional outcomes after operative management of extra-articular glenoid neck and scapular body fractures. J Bone Joint Surg Am 2016;98:1623-30. [Google Scholar] |
| 18. | Herrera DA, Anavian J, Tarkin IS, Armitage BA, Schroder LK, Cole PA. Delayed operative management of fractures of the scapula. J Bone Joint Surg Br 2009;91:619-26. [Google Scholar] |
| 19. | Jones CB, Cornelius JP, Sietsema DL, Ringler JR, Endres TJ. Modified Judet approach and minifragment fixation of scapular body and glenoid neck fractures. J Orthop Trauma 2009;23:558-64. [Google Scholar] |
| 20. | Cole PA, Gauger EM, Herrera DA, Anavian J, Tarkin IS. Radiographic follow-up of 84 operatively treated scapula neck and body fractures. Injury 2012;43:327-33. [Google Scholar] |
| 21. | Schofer MD, Sehrt AC, Timmesfeld N, Störmer S, Kortmann HR. Fractures of the scapula: Long-term results after conservative treatment. Arch Orthop Trauma Surg 2009;129:1511-9. [Google Scholar] |
| 22. | Jones CB, Sietsema DL. Analysis of operative versus nonoperative treatment of displaced scapular fractures. Clin Orthop Relat Res 2011;469:3379-89. [Google Scholar] |
| 23. | Dimitroulias A, Molinero KG, Krenk DE, Muffly MT, Altman DT, Altman GT. Outcomes of nonoperatively treated displaced scapular body fractures. Clin Orthop Relat Res 2011;469:1459-65. [Google Scholar] |
| 24. | Kannan S, Singh HP, Pandey R. A systematic review of management of scapular fractures. Acta Orthop Belg 2018;84:497-508. [Google Scholar] |
Fulltext Views
3,022
PDF downloads
871





