Translate this page into:
Nonunion of lateral humeral condyle fracture with progressive cubitus valgus in children: How to address the challenge?
2 Department of Orthopedics, King Fahad General Hospital, Almadinah Almunawwarah, Saudi Arabia
3 College of Medicine, King Saud University, Riyadh, Saudi Arabia
4 Department of Orthopedics, Pediatric Orthopedic Surgery Division, King Faisal Specialist Hospital & Research Centre, Riyadh, Saudi Arabia
Corresponding Author:
Nezar B Hamdi
Department of Orthopedics, Pediatric Orthopedic Surgery Division, King Faisal Specialist Hospital & Research Centre, Riyadh
Saudi Arabia
Nhamdi@kfshrc.edu.sa
| How to cite this article: Alshammari AN, Alrehaili HH, Aldayel AK, Hamdi NB. Nonunion of lateral humeral condyle fracture with progressive cubitus valgus in children: How to address the challenge?. J Musculoskelet Surg Res 2019;3:311-314 |
Dear Sir,
Nonunion, and subsequently, cubitus valgus deformity are some of the unacceptable complications if the lateral humeral condyle (LHC) fracture has not been timely and appropriately treated.[1] Nonetheless, the optimal management of the nonunion LHC fracture when presenting late with valgus deformity, the timing of surgery, which internal fixation method to use, and which osteotomy technique to use remains a topic of considerable controversy.
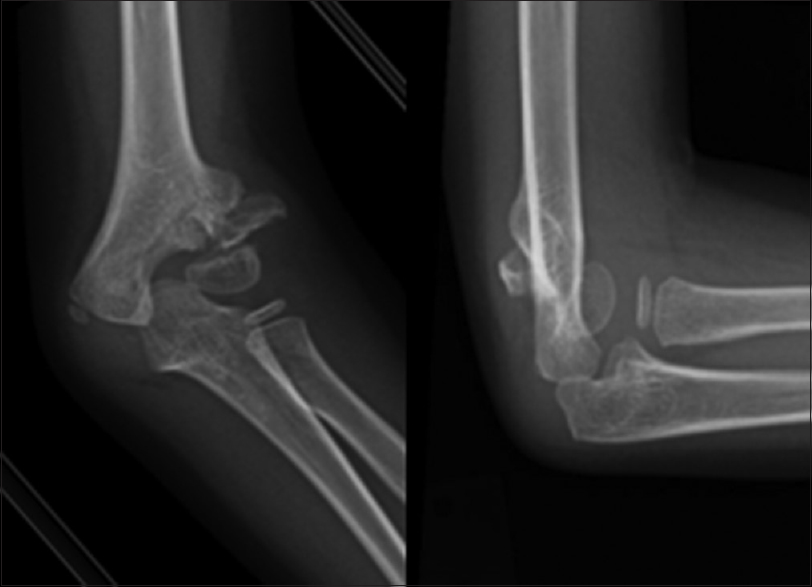
A 4-year-old girl was referred to our clinic for a left elbow valgus deformity. She injured her left elbow 11 months earlier, and it was treated by cast immobilization at a local hospital at that time. The initial diagnosis and the details of the treatment were unknown. Her parents noticed a gross progressive valgus deformity of the left elbow. The patient did not have any pain or neurological complaints. On examination, the patient had left elbow gross cubitus valgus deformity. She had no restriction of elbow motion; the elbow was not painful, and there were no signs of ulnar neuropathy. However, plain radiographs and three-dimensional reconstruction computed tomography (CT) showed a nonunion of fracture of LHC with proximal migration of the lateral condyle. The carrying angle was 34° of valgus on the affected side as compared to 16° on the normal side [Figure - 1], [Figure - 2], [Figure - 3].
 |
| Figure 1: Preoperative cubitus valgus deformity of the left elbow |
 |
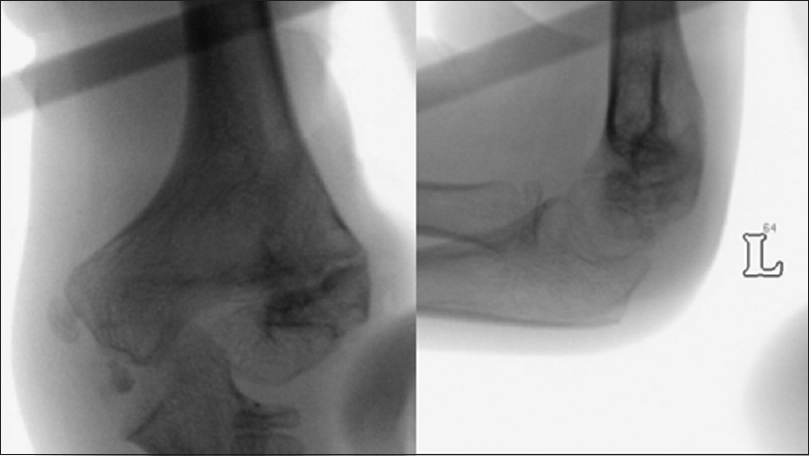
| Figure 2: Radiograph of the left elbow in anteroposterior and lateral views demonstrated nonunion of lateral humeral condyle with proximal migration of the lateral condyle and the carrying angle was 34° of valgus |
 |
| Figure 3: Preoperative three-dimensional reconstruction computed tomography |
In view of the progression and degree of deformity, the surgeon was prompted to perform a prophylactic ulnar nerve transposition and medial closing-wedge osteotomy.
The surgery was performed under general anesthesia with upper arm tourniquet. Dual incisions were used with Kaplan's approach laterally, and a standard medial approach to the elbow.[2] A medial incision parallel to the intermuscular septum was developed, and anterior subcutaneous transposition of the ulnar nerve secured with an adipose flap was performed as a prophylactic procedure to prevent a possibility of any neural symptoms. The lateral condyle was exposed through the lateral incision. After identifying the nonunion site, the fibrous tissue between the fracture fragments was removed. Freshening of the opposing bony fragments was performed carefully to achieve healthy bleeding surfaces. The fracture was reduced under the control of an image intensifier, with the help of a bone clamp and one partially threaded cancellous screw, which was inserted perpendicular to the fracture line. A mineralized collagen bone graft was injected directly at the nonunion site. Then, starting with the distal osteotomy, which was done parallel the articular surface at the upper margin of the olecranon fossa.
The proximal osteotomy was performed at about 15° angle from the distal osteotomy, keeping the lateral cortex intact. The medial-based wedge bone was removed from the lateral approach. With the elbow extended, while maintaining the periosteal hinge, the wedge was closed by fracturing the lateral cortex. Two crossed Kirschner wires (K-wires) were inserted into the lateral column. One more K-wire was inserted from the medial condyle to the lateral cortex of the proximal fragment for more stability. Intraoperatively, elbow range of motion was full in both flexion and extension arcs and in pronation and supination. The valgus correction was checked before applying an above elbow slab [Figure - 4].
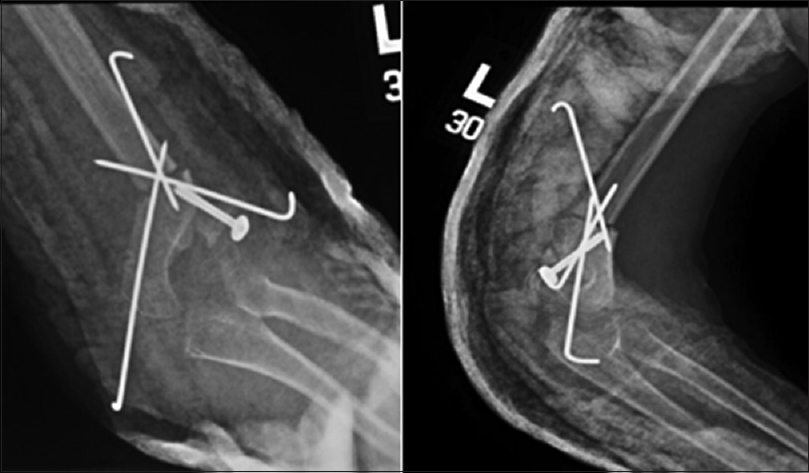 |
| Figure 4: Immediate postoperative radiographs of the left elbow (anteroposterior and lateral views) |
Postoperatively, the patient's elbow was immobilized for 6 weeks, and K-wires were removed at 6 weeks. The child regained almost full flexion-extension range of motion, which was 0–140° within 3 months [Figure - 5]. At 18 months postsurgery, the patient was free of symptoms and had a full elbow range of motion. The carrying angle was 10°. Radiographs and CT revealed a good bone union with no signs of osteonecrosis or heterotopic ossification [Figure - 6].
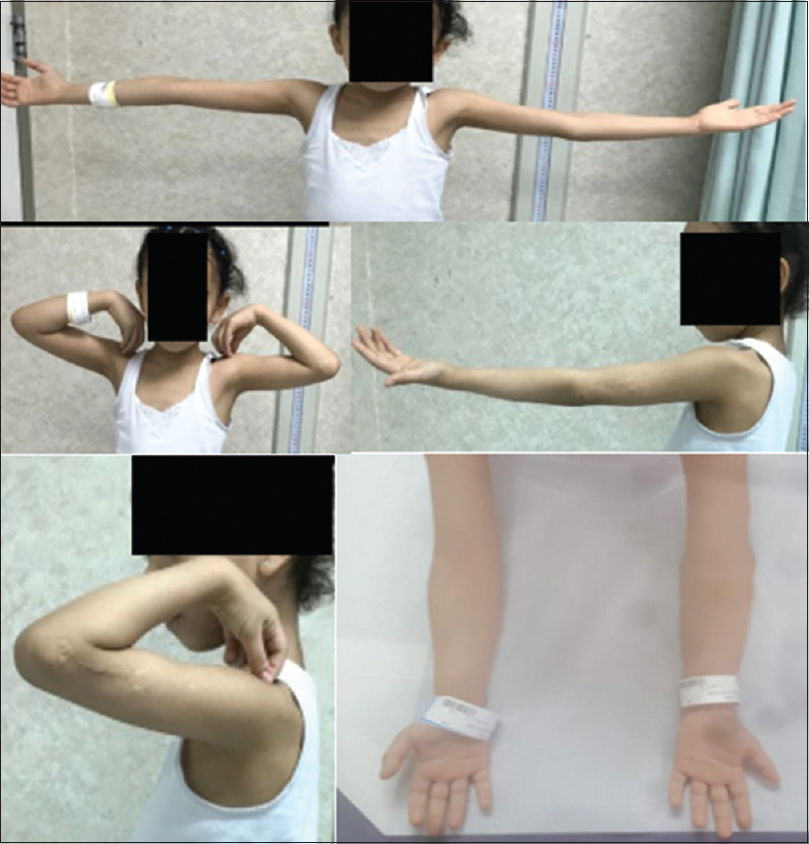 |
| Figure 5: Clinical photos at 18 months after surgery. The child had a full range of motion with good alignment |
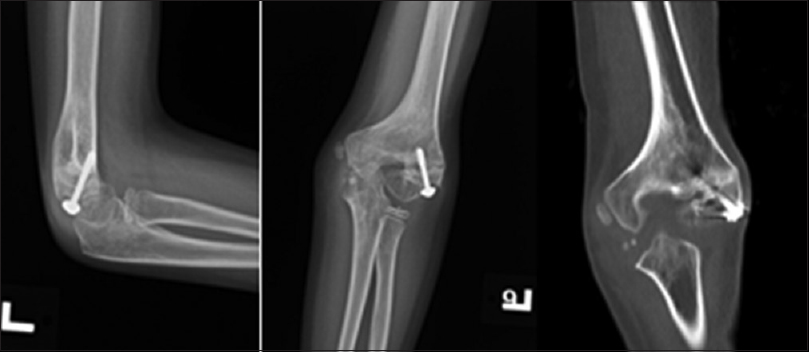 |
| Figure 6: Radiographs and computed tomography at 18 months after surgery showed a united lateral humeral condyle with carrying angle of 10° without evidence of avascular necrosis |
Consequently, 2 weeks after his last visit, the screw was removed, and complete fracture healing was recognized intraoperatively at the time of the screw removal [Figure - 7]. At the 2-year follow-up, the patient was asymptomatic and maintaining the carrying angle in 10° valgus. The elbow flexion-extension arc was 0–140°. The Mayo Elbow Performance Score was 90 (excellent).[3]
 |
| Figure 7: Intraoperative radiographs from image intensifier; screw was removed |
Despite surgical treatment of nonunion LHC fracture being a controversial issue due to possible complications such as elbow stiffness, avascular necrosis, and persistent nonunion,[4],[5],[6] this seems not to be the situation in the case described in this letter. However, Kim et al. mentioned that surgical treatment is recommended for a child with an open epiphyseal plate, which can be mediated by internal fixation and bone grafting with limited exposure of the distal part of the humerus. By doing so, it will prevent further deterioration of the cubitus valgus deformity.[7],[8]
Shimada et al. recommended surgical treatment in patients with considerable deformity, progressive angulation, and/or ulnar nerve problems.[9] Abed et al. reported approximately 10 weeks as the average time to union of LHC fracture nonunion after screw fixation with adequate compression, and this being the rationale behind the use of compression screws for fixation rather than K-wires.[10] Pin-tract infection is a common complication of delayed removal of K-wires, and if the pin-tract infection was severe enough, it might result in a loss of reduction and fixation.[10],[11] In addition, the screws provide better purchase, compression, and stability of the union site than K-wires, thus prompting healing and allowing early mobilization of the elbow.[10],[12],[13]
Tien et al. routinely exposed, released, and transposed the ulnar nerve subcutaneously anteriorly in all cases regardless of whether they have ulnar nerve symptoms or not.[14] In our case, we performed anterior transposition of the ulnar nerve, to protect the nerve during the surgery and to avoid the development of any neurological symptoms secondary to postoperative adhesions in the nerve bed.[10],[14]
Surgical osteotomy is done for valgus deformities of the elbow; many of these surgeries are done for cosmetic reasons rather than functional limitations.[8] Similarly, our case showed no signs of restriction of movement; however, she had nonunion with an increasing carrying angle.
Some authors reported treatment of late nonunion with cubitus valgus deformity by staged in situ fixation of the nonunion with or without ulnar nerve transposition followed by the second-stage corrective varus osteotomy of the distal humerus. The interval usually being 6 months between the two stages.[15] On the other hand, others described a single-stage operation, including fixation of the nonunion site and corrective varus osteotomy with or without anterior ulnar nerve transposition. This combined technique can successfully achieve different aspects of the problem simultaneously; by fixation of the LHC nonunion and restoring limb alignment.[10],[14],[16]
We believe that the single-stage operation provides redistribution of the forces across the elbow joint and anatomical limb alignment. It also provides the elbow with the right environment for nonunion healing and regaining movement.
There are various types of osteotomies. In our reported case, we used a medial closing-wedge osteotomy. This technique is easy to perform, safe, and was used to restore the carrying angle by utilizing the long axis of the humerus and the epicondyle with an imaginary line connecting the two epicondyles.[4],[17] Some authors reported distorted elbow appearance in some cases after simple closing wedge osteotomy of the medial column, and they recommended a combined wedge and transposition osteotomy for functional and esthetic correction.[4],[15] However, in our case, a simple medial closing wedge osteotomy provided satisfactory correction and good cosmetic appearance.
Supracondylar dome osteotomy is another type of osteotomy; in this technique, the center of rotation of the distal humeral fragment remains at the midline of the humerus.[14] To correct the deformity, a small arc of rotation is required, which results in less valgus movement; unlike closing wedge osteotomy, which requires a more significant valgus movement. This weak valgus moment in supracondylar dome osteotomy, in turn, increases the mechanical stability and enhances the union at the osteotomy site.[10],[14] The main drawback of dome osteotomy is that it is technically more complicated than the simple closing wedge osteotomy.[18] Therefore, we think that using an anterior transposition of the ulnar nerve, open reduction, internal fixation of the nonunion site with bone grafting, and medial closing wedge osteotomy of the humerus as a single-stage procedure are a viable solution and effective method for this uncommon and challenging problem. It has shown positive results by decreasing the carrying angle with the good bone union and functional outcome. A longer follow-up and more cases are necessary to confirm these findings.
The clinical message from this letter is to remind the readers about different treatment options in treating a valgus deformity in a LHC nonunion and to take the necessary precautions in avoiding the unfavorable complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient's guardians have given their consent for the patient's images and other clinical information to be reported in the journal. The patient's guardians understand that the name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Skak SV, Olsen SD, Smaabrekke A. Deformity after fracture of the lateral humeral condyle in children. J Pediatr Orthop B 2001;10:142-52. [Google Scholar] |
| 2. | Kaplan EB. Surgical approaches to the proximal end of the radius and its use in fractures of the head and neck of the radius. J Bone Joint Surg 1941;23:86. [Google Scholar] |
| 3. | Morrey BF, An KN, Chao EY. Functional evaluation of the elbow. In: Morrey BF, editor. The Elbow and Its Disorders. 2nd ed. Philadelphia: W. B. Saunders; 1993. p. 86-9. [Google Scholar] |
| 4. | Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma 1964;4:592-607. [Google Scholar] |
| 5. | Toh S, Tsubo K, Nishikawa S, Inoue S, Nakamura R, Narita S. Osteosynthesis for nonunion of the lateral humeral condyle. Clin Orthop Relat Res 2002;405:230-41. [Google Scholar] |
| 6. | Jakob R, Fowles JV, Rang M, Kassab MT. Observations concerning fractures of the lateral humeral condyle in children. J Bone Joint Surg Br 1975;57:430-6. [Google Scholar] |
| 7. | Flynn JC. Nonunion of slightly displaced fractures of the lateral humeral condyle in children: An update. J Pediatr Orthop 1989;9:691-6. [Google Scholar] |
| 8. | Kim HT, Lee JS, Yoo CI. Management of cubitus varus and valgus. J Bone Joint Surg Am 2005;87:771-80. [Google Scholar] |
| 9. | Shimada K, Masada K, Tada K, Yamamoto T. Osteosynthesis for the treatment of non-union of the lateral humeral condyle in children. J Bone Joint Surg Am 1997;79:234-40. [Google Scholar] |
| 10. | Abed Y, Nour K, Kandil YR, El-Negery A. Triple management of cubitus valgus deformity complicating neglected nonunion of fractures of lateral humeral condyle in children: A case series. Int Orthop 2018;42:375-84. [Google Scholar] |
| 11. | Bogdan A, Quintin J, Schuind F. Treatment of displaced supracondylar humeral fractures in children by humero-ulnar external fixation. Int Orthop 2016;40:2409-15. [Google Scholar] |
| 12. | Von Laer L. Screw fixation of lateral condyle fractures of the humerus in children. Orthop Traumatol 1993;2:29-35. [Google Scholar] |
| 13. | Li WC, Xu RJ. Comparison of Kirschner wires and AO cannulated screw internal fixation for displaced lateral humeral condyle fracture in children. Int Orthop 2012;36:1261-6. [Google Scholar] |
| 14. | Tien YC, Chen JC, Fu YC, Chih TT, Hunag PJ, Wang GJ, et al. Supracondylar dome osteotomy for cubitus valgus deformity associated with a lateral condylar nonunion in children. J Bone Joint Surg Am 2005;87:1456-63. [Google Scholar] |
| 15. | Waters P, Bae D. Pediatric Hand and Upper Limb Surgery: A Practical Guide. 1st ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2012. p. 326-30. [Google Scholar] |
| 16. | Abzug JM, Herman MJ, Kozin S. Spring. Pediatric Elbow Fractures: A Clinical Guide to Management. Cham: Springer International Publishing; 2018. [Google Scholar] |
| 17. | Abdelmotaal HM, Abutalib RA, Khoshhal KI. The closed wedge counter shift osteotomy for the correction of post-traumatic cubitus varus. J Pediatr Orthop B 2013;22:376-82. [Google Scholar] |
| 18. | Kumar K, Sharma VK, Sharma R, Maffulli N. Correction of cubitus varus by French or dome osteotomy: A comparative study. J Trauma 2000;49:717-21. [Google Scholar] |
Fulltext Views
3,983
PDF downloads
549





