Translate this page into:
Patients' satisfaction and outcomes of minimally invasive sacroiliac joint fusion at a tertiary care center
2 Department of Orthopedics, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia
Corresponding Author:
Omar A Al-Mohrej
Department of Orthopaedics, King Faisal Specialist Hospital and Research Centre, Riyadh
Saudi Arabia
mohrejo@kfshrc.edu.sa
| How to cite this article: Al-Mohrej OA, Khan NU, Rehman SU, Al-Rabiah AM. Patients' satisfaction and outcomes of minimally invasive sacroiliac joint fusion at a tertiary care center. J Musculoskelet Surg Res 2020;4:205-209 |
Abstract
Objectives: Sacroiliac (SI) joint dysfunction usually relates to SI joint pain that results from unusual patterns of motion within the joint, whether excessive or insufficient. SI joint pain is a frequent reason for axial back pain, which is suffered by around 30% of the population. This retrospective study intends to examine the safety and efficiency of minimally invasive (MI) SI joint fusion that employs triangular implants for individuals where conservative management has not succeeded. Methods: An observational study with eight patients on whom one surgeon performed ten consecutive SI joint fusion operations; all patients have completed their 12-month review. The study has examined medical records for demographic details, perioperative data, pain scores, satisfaction levels, safety procedures, complications, and fusion rates 1 year after the operation. Results: At the time of surgery, the patients had a mean age of 37.87 years (ranging from 17 to 58). All but one patient were female. Between 2016 and 2019, 10 SI joints in these eight patients underwent fusion. Four patients had left side fusion, two had right side fusion, and two had bilateral SI joint fusion. Pain scores were reduced considerably, with a mean drop of 6. On the 12-month follow-up, with only one joint had not undergone satisfactory fusion. Conclusions: This study demonstrated that MISI joint fusion employing triangular implants is both safe and effective for treating this particular cohort of patients.
Introduction
Lower back pain (LBP) is experienced by approximately 90% of adults during their lifetime. It is one of the most frequently cited reasons for visiting a physician in the USA.[1],[2] LBP has a huge effect on the economy, caused losses in 2005 approximated at $85 billion.[3]
LBP can be caused by facet arthritis, muscle strains/injuries, disc herniation, sacroiliac (SI) dysfunction, and scoliosis; in addition, hip conditions can often present with LBP.[4] Thus, treating LBP successfully requires the identification of the source of the pain, which can be highly challenging because the condition has numerous inputs.
Recent research has reported that between 15% and 30% of patients suffering from LBP exhibited SI joint difficulties.[4] In addition, around 75% of patients who had undergone lumbar fusion went on to experience a high level of degeneration in SI joints on examination 5 years postoperatively.[5],[6],[7] Diagnostic accuracy can be achieved by taking a detailed history, full physical examination, radiology, and diagnostic injections.[8]
Nerve root ablation has been used to treat SI joint pain without surgery and returned promising results, although these have generally been temporary.[9] Radiofrequency ablation is the only treatment for which any good evidence is present supporting the treatment of SI joint pain with nonsurgical techniques.[10]
Many approaches have been described for SI joint fusion.[11] The most commonly used approaches are open using the Smith-Petersen approach,[12] with plate and screws, and minimally invasive (MI) approaches under fluoroscopy guidance. There are, however, many drawbacks to open SI joint fusion, including long recovery time/hospital stays, high levels of nonunion, disappointing long-term outcomes, intraoperative blood losses, and poor patient satisfaction ratings.[13] Furthermore, open surgery demands a substantial incision, autograft bone harvest, and patients cannot bear weight on the joint for a considerable time after surgery.[14]
In recent times, MISI joint fusion has become popular, and the results are highly promising.[15],[16],[17],[18] Nevertheless, MISI joint fusion does carry the risks of complications and adverse outcomes.
Based on a multicenter, prospective randomized controlled trial, MISI fusion provided improvements in pain, disability, and quality of life compared to nonsurgical management.[17] As well, MISI joint fusion had more favorable clinical outcomes compared to conventional open surgical SI joint arthrodesis.[12]
However, up to our knowledge, studies reporting the complications are scarce. Hence, this study intends to explore patients' satisfaction, surgical outcomes, and complications of MISI joint fusion for degenerative sacroiliitis using triangular, porous titanium plasma spray-coated implants.
Subjects and Methods
Study subject and data used
This observational study reports the results of 10 consecutive joint fusion operations for patients operated on by a single surgeon (AMR). Medical records underwent review to look at demographic data, perioperative data, pain scores, safety procedures, complications, level of fusion, and patient satisfaction levels, both 1 year and 5 years after the surgery. While the level of pain was assessed using a 0–10 Visual Analog Scale (VAS), satisfaction was evaluated using a binary manner by questioning the patients if they would have the same surgery again for the same result.[19]
Three physicians (OAM, NUK, and SUR) undertook a review of medical records for every patient attending the spinal clinic at the King Faisal Specialist Hospital and Research Center (KFSH and RC) between January 1, 2010 and December 2015. All patients for whom there was a follow-up of at least 5 years were added to the review. No loss in follow-up was encountered.
Diagnostic test and inclusion criteria
Patients attended the clinic suffering SI joint pain alongside the complaints of LBP spreading into the back of their thighs. Pain in the buttocks and groin were also mentioned. Patient history, clinical examination, and diagnostic injections were used to diagnose the patients with either SI joint disruption or degenerative sacroiliitis. Every patient underwent a full clinical and physical examination to find the primary cause of pain in the most accurate possible manner, given the complexity of their pain issues. Diagnoses were guided by the findings of positive results with three or more maneuvers during provocative physical examination such as distraction, thigh thrust, compression, flexion-abduction-external rotation test, and Gaenslen tests. For the assessment of pathology of the lumbar pelvic hip complex, physicians employed diagnostic imaging techniques (computed tomography [CT] scan). Magnetic resonance imaging, however, was used in cases with the symptoms of degenerative disc diseases.
Patients underwent image-guided diagnostic injection of the SI joints under local anesthetic to confirm the diagnosis when there was an agreement between the outcomes of clinical investigation, physical examination, and imaging. If pain reduced by 50% straight off the local anesthetic administration, this indicated that the SI joint was the source of pain. The patient is eligible then to undergo MISI joint fusion. Three triangular titanium implants, coated with porous plasma, are placed across SI joint for the stabilization and fusion of the joint with no requirement for a supporting bone graft.
Operative technique
MISI joint fusion takes place using general endotracheal anesthesia, the patient is placed prone on a Jackson table. Fluoroscopy is used to obtain inlet, outlets, and lateral sacral views visualizing S1 foramen, anterior/posterior sacral lines, and sacral ala line and incision of between 3 cm and 5 cm is performed above the lateral buttock. Blunt dissection of the gluteal fascia takes place, with the gluteus maximus being split down to the ilium's outer table in line with its direction. Under the control of fluoroscopy, a guidewire is run through the ilium above the SI joint into the superior, lateral, or inferior sacrum to the S1 foramen according to how many implants are to be inserted and the surgeon's choice [Figure - 1]. Implant length is determined, employing a depth gauge. The guidewire is used to pass through a soft-tissue protector, and the bone is decorticated, employing a broach or hand drill. The implant is placed in the target location of arthrodesis, employing a pin-guide system. The majority of patients are given two or three implants for the stabilization of the SI joint, followed by closure of the tissue layers. The surgery and follow-up were undertaken by one surgeon (AMR).
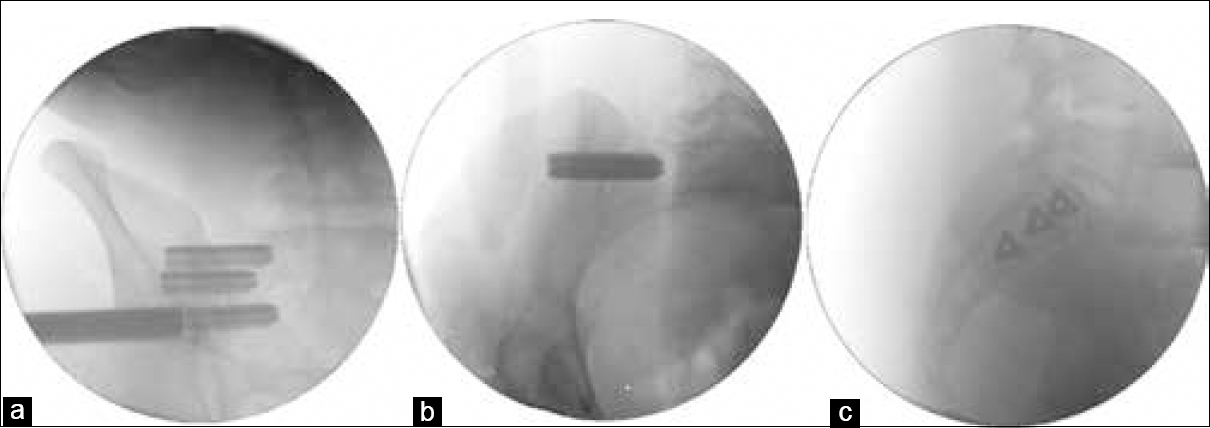 |
| Figure 1: (a) The implant is placed in the target location of arthrodesis, employing a pin-guide system. (b) Final anteroposterior and (c) lateral views of the implants in the desired location. All are fluoroscopic images |
Postoperative instructions
Patients are given instructions not to weight-bear using a walker initially for 3 weeks, followed by 4 weeks employing toe touch ambulation. Weight-bearing exercises are increased in line with patient tolerance until full weight-bearing walking occurs.
Statistical analysis
Statistical analysis was conducted using the Statistical Package for the Social Sciences software (IBM Corp. Released 2013. IBM SPSS Statistics for Mac, Version 22.0. Armonk, IBM Corp, NY). The quantitative data were described employing the descriptive measures, for example, standard deviation and arithmetic mean. With the categorical variables, descriptive statistics underwent summary as percentages and frequencies.
Results
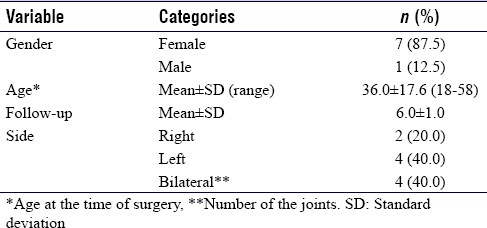
At the time of surgery, the mean patient age was 36.0 ± 17.6 years (ranging from 18 to 58). One patient was male, with seven females [Table - 1]. In total, eight patients had 10 SI joints fused between 2010 and 2015: Four underwent left side fusion, two underwent right side fusion, and two underwent bilateral SI joint fusion.
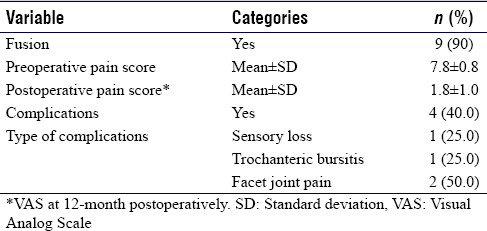
Numerical Rating Scale was employed to find a mean preoperative pain score, which was 7.8 ± 0.8. Pain improvement was found on the 6–8-week follow-up consultation, with symptoms continuing to be relieved on both 3- and 6-month follow-ups. The improvement continued at the 1-year follow-up, with the mean pain score dropping by − 6.0–1.8 ± 1.0.
For all patients except one, clinically significant improvements took place (defined as a rise above the baseline of 2+ points).[20] On a 5-year follow-up, 90% of the patients were satisfied and would be happy to undergo similar surgery for the same outcome. Patient follow-up was conducted with radiographs at 3 and 6 months; the level of fusion was examined using CT scanning at 12 months. Only one patient had not experienced acceptable solid fusion in the SI joint.
No intraoperative complications occurred, and every patient experienced satisfactory wound healing without complication. A single patient experienced trochanteric bursitis, which underwent successful treatment with medication and physical therapy, with another developing sensory loss in the sole of his foot on the side of the operation. On postoperative follow-up, two patients suffering from LBP caused by degenerative disc disease were still experiencing this pain, but there were significant improvements in the SI joint pain [Table - 2].
Discussion
For the relief of SI joint pain, SI joint fusion is most frequently addressed at present by using MISI joint fusion surgery. MISI joint fusion has the advantage of only requiring a minimal incision, having a short surgery time, low levels of blood loss, and shorter immobilization period. While at present, MISI joint fusion is the most preferred procedure for SI joint fusion, it is not uncommon for perioperative and postoperative complications to arise. There is little research available regarding patient satisfaction levels/postoperative complications following this type of the surgery.
The procedural complication rate of 11.11% was found by Shamrock et al.; the most frequent problems were hematomas, trochanteric bursitis, and wound infection; 3% of patients experienced device-related difficulties, the most frequent being impingement on the nerve root.[21] Wound infection was reported by Heiney et al. as the most frequent problem followed by nerve root impingement.[20] In the current study, there were no complications with wounds. However, two patients experienced pain in the facet joint, this occurred with the study of Sachs and Capobianco who found 20% of patients experienced this type of pain, which may be explainable by the presence of degenerative spinal disc disease and the fact that patients undergoing surgery tend to be in a higher age bracket.[15]
In terms of the safety of percutaneous MISI joint fusion, efficient intraoperative imaging is essential in preventing complications arising from the procedure, such as poor positioning of implants or irritation of the nerve root.[21] It is crucial to place the implants probably that preoperative CT scans and intra-operative fluoroscopic views (inlet, outlet, lateral, and oblique) are carefully evaluated. Implants have to pass over the SI joint without breaching the SI osseous envelope to avoid iatrogenic nerve injury.[21]
The literature reports high levels of patient satisfaction postoperatively. Rudolf et al. observed in a study over 5 years the outcomes from this type of surgery, both clinically and radiographically, illustrating that VAS pain scores fell from 83 to 24 after this type of surgery.[22] In addition, they found that 80% of patients experienced significant clinical benefits after 1 year, which was still the case after 5 years.[19] Sachs and Capobianco found similar results, with a study of 40 patients demonstrating that pain scores improved on average by 78 points after 1 year.[15] Rudolf examined 50 patient histories, reporting that pain/functional scores improved significantly no matter what the patient's lumbar spinal fusion history was.[23] The findings of the current study consensus with those of the studies mentioned above, with VAS scores improving by six points. All patients involved, expressed satisfaction with the results of surgery, with 90% stating that they would be happy to undergo the same operation if they experienced the same problem. However, the majority of patients in the study cohort are younger than those in other studies, and the better quality of bone in these patients might have contributed to the excellent outcomes from surgery and better pain control.
A limitation of this study is that the sample cohort is relatively small; nevertheless, the findings showed great promise. While every patient who experienced SI fusion was included, retrospective studies are open to selection bias that could affect the results. Although we selected a sample cohort with extensive follow-up data, the study was conducted in just one center, which affects results' generalizability. Furthermore, one of the main limitations is not using a validated method to measure the satisfaction. This could affect the findings significantly. Hence, our recommendations should be taken into consideration with the aforementioned limitations and take into account similar studies in the literature. Despite these limitations, our study could be interpreted as an eye-opener on SI joint fusion using MI techniques in Saudi Arabia. Further studies taking into consideration these limitations and involving control groups would be of great value.
Conclusions
If conservative measures are not successful, then SI fusion using MI techniques is a relatively safe and highly efficient alternative treatment for properly chosen patients. More high-quality research covering a longer time period and with larger sample size is recommended.
Ethical considerations
This study obtained ethical approval from KFSH&RC Research advisory council.
Acknowledgment
The authors would like to thank Ms. Shuruq A. Al-Sakran, research coordinator, for her support in this research project.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
OAM conceived and designed the study, OAM and NUK conducted research, NUK and SUR provided research materials and collected and organized data. OAM analyzed and interpreted data. OAM, NUK, and AMR wrote the initial and final draft of the article and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
| 1. | Weksler N, Velan GJ, Semionov M, Gurevitch B, Klein M, Rozentsveig V, et al. The role of sacroiliac joint dysfunction in the genesis of low back pain: The obvious is not always right. Arch Orthop Trauma Surg 2007;127:885-8. [Google Scholar] |
| 2. | Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA, American Society of Interventional Pain Physicians. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician 2009;12:E35-70. [Google Scholar] |
| 3. | Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Google Scholar] |
| 4. | Sembrano JN, Polly DW. How often is low back pain not coming from the back? Spine (Phila Pa 1976) 2009;34:E27-32. [Google Scholar] |
| 5. | Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: A prospective cohort study over five-year follow-up. Spine (Phila Pa 1976) 2008;33:1192-8. [Google Scholar] |
| 6. | DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med 2011;12:732-9. [Google Scholar] |
| 7. | Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976) 1996;21:1889-92. [Google Scholar] |
| 8. | Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac joint pain and its treatment. Clin Spine Surg 2016;29:42-8. [Google Scholar] |
| 9. | Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: Outcomes of a new technique. J Spinal Disord Tech 2008;21:579-84. [Google Scholar] |
| 10. | Polly DW, Cher DJ, Wine KD, Whang PG, Frank CJ, Harvey CF, et al. Randomized controlled trial of minimally invasive sacroiliac joint fusion using triangular titanium implants vs. nonsurgical management for sacroiliac joint dysfunction: 12-month outcomes. Neurosurgery 2015;77:674-90. [Google Scholar] |
| 11. | Yson SC, Sembrano JN, Polly DW Jr., Sacroiliac joint fusion: Approaches and recent outcomes. PM R 2019;11 Suppl 1:S114-S117. [Google Scholar] |
| 12. | Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, et al. Open versus minimally invasive sacroiliac joint fusion: A multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013;7:14. [Google Scholar] |
| 13. | Ashman B, Norvell DC, Hermsmeyer JT. Chronic sacroiliac joint pain: Fusion versus denervation as treatment options. Evid Based Spine Care J 2010;1:35-44. [Google Scholar] |
| 14. | Lorio MP, Polly DW Jr., Ninkovic I, Ledonio CG, Hallas K, Andersson G. Utilization of minimally invasive surgical approach for sacroiliac joint fusion in surgeon population of ISASS and SMISS Membership. Open Orthop J 2014;8:1-6. [Google Scholar] |
| 15. | Sachs D, Capobianco R. Minimally invasive sacroiliac joint fusion: One-year outcomes in 40 patients. Adv Orthop 2013;2013:536128. [Google Scholar] |
| 16. | Ledonio CG, Polly DW, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion: Are they similarly safe and effective? Clin Orthop Relat Res 2014;472:1831-8. [Google Scholar] |
| 17. | Polly DW, Swofford J, Whang PG, Frank CJ, Glaser JA, Limoni RP, et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg 2016;10:28. [Google Scholar] |
| 18. | Cher DJ, Frasco MA, Arnold RJ, Polly DW. Cost-effectiveness of minimally invasive sacroiliac joint fusion. Clin Outcomes Res 2015;8:1-14. [Google Scholar] |
| 19. | Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J 2014;8:375-83. [Google Scholar] |
| 20. | Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg 2015;9:40. [Google Scholar] |
| 21. | Shamrock AG, Patel A, Alam M, Shamrock KH, Al Maaieh M. The safety profile of percutaneous minimally invasive sacroiliac joint fusion. Global Spine J 2019;9:874-80. [Google Scholar] |
| 22. | Rudolf L. MIS fusion of the SI joint: Does prior lumbar spinal fusion affect patient outcomes? Open Orthop J 2013;7:163-8. [Google Scholar] |
| 23. | Rudolf L. Sacroiliac joint arthrodesis-MIS technique with titanium implants: Report of the first 50 patients and outcomes. Open Orthop J 2012;6:495-502. [Google Scholar] |
Fulltext Views
1,773
PDF downloads
393





