Translate this page into:
Provisional fixation of unstable femoral neck basicervical fractures: A web-based survey and biomechanical assessment using a sliding hip screw construct
*Corresponding author: Mohammad M. Alzahrani, Department of Orthopedics, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia. mmalzahrani@iau.edu.sa
-
Received: ,
Accepted: ,
How to cite this article: Alzahrani MM, Culliton KN, Wilkin GP, Papp SR, Liew AS. Provisional fixation of unstable femoral neck basicervical fractures: A web-based survey and biomechanical assessment using a sliding hip screw construct. J Musculoskelet Surg Res 2022;6:70-6.
Abstract
Objectives:
Many hip fractures are considered rotationally unstable, especially during lag screw insertion. To counteract this instability, multiple provisional fixation constructs have been used to maintain the fracture reduction. This study aimed to compare the methods of provisional fixation biomechanically in ba sicervical femoral neck fractures.
Methods:
A web-based survey was sent by e-mail to members of three orthopedic assocations with questions concerning used techniques for provisional fixation of unstable basicervical femoral neck fractures and these results were used to guide our biomechanical assessment. Twenty, fourth-generation composite proximal femurs were osteotomized in the basicervical region to simulate a basicervical fracture. These fractures were anatomically reduced and one of the four provisional fixation constructs was applied. A sliding hip screw was then inserted with a torque limiter to the appropriate depth. The amount of fracture displacement during screw insertion was collected and analyzed.
Results:
Of the 142 respondents, 79.6% apply some form of provisional fixation. Derotational screw was the most commonly used provisional fixation (43.4%), followed by one superior Kirschner wire (K-wire) (39.8%). Biomechanically, the single derotation screw construct showed significantly less displacement (0.92 mm) than the one superior K-wire construct (3.09 mm). No other significant differences in fracture displacement were found between the groups.
Conclusion:
This study highlights that the majority of surgeons apply a form of provisional fixation during the surgical management of unstable basicervical femoral neck fractures. We have shown biomechanically that the single derotation screw had superior rotational stability when compared to the one superior K-wire.
Keywords
Basicervical
Femoral neck
Fixation
Fractures
Provisional
Survey
INTRODUCTION
The number of hip fracture cases, including femoral neck fractures, is expected to increase significantly by mid-century, and it is estimated that the global incidence will reach more than 2 million in 2050.[1] Managing these fractures safely and cost-effectively will be of uttermost importance. Many surgeons have considered basicervical femoral neck fractures to be a difficult subtype to treat due to the inherent rotational instability of the fracture.[2,3]
While an adequate reduction can be commonly achieved, displacement of the fracture typically occurs during insertion of the fixation device, commonly a sliding hip screw (SHS) or cephalomedullary nail (CMN).
Multiple provisional fixation techniques have been described to counteract this instability, including a superior derotational screw, one or two superior Kirschner wires (K-wires), and different types of clamps and bone hooks.[4,5] Typically, the surgeon applies one or a number of these methods depending on personal preference or training received without any concrete evidence to support the choice of method. The addition of a superior derotational screw to the SHS in the unstable femoral neck and hip fractures has been shown to offer superior rotational stability,[3,6] but unfortunately, there is a lack of studies exploring other provisional fixation methods. In addition, the majority of biomechanical studies have assessed the stability of the fracture after the final fixation construct is applied. However, fracture displacement can commonly occur intraoperatively during insertion of the lag screw for an SHS or CMN.
Therefore, we designed our study in two parts. The first part was a web-based survey of practicing orthopedic surgeons to explore commonly used methods of provisional fixation in unstable basicervical femoral neck fractures. The survey results were then used to guide our biomechanical testing, which assessed the rotational stability of four of the most commonly applied provisional fixation methods in a basicervical femoral neck fracture synthetic bone model. We hypothesized that the derotational screw and the transcervical-transacetabular (TC-TA) K-wire constructs would provide superior rotational stability compared to one or two superior K-wires.
MATERIALS AND METHODS
Web-based survey
A web-based anonymous survey was sent, through e-mail, to all surgeon members of the Canadian Orthopaedic Association (COA), Orthopaedic Trauma Association (OTA), and Saudi Orthopedic Association (SOA) between January 2019 and October 2019. Reminders were sent on a monthly or bimonthly basis and the survey was closed in November 2019, at which time, the data were collected and evaluated.
The web-based survey consisted of questions concerning the type and length of the surgeon’s practice, in addition to questions related to the management of unstable basicervical hip fractures (type of preferred fixation construct, a preferred technique of provisional fixation if any, and order of fixation) [Supplemental - Figure 1]. The survey was initially piloted on 10 volunteers to assess the time required to complete the survey and the clarity of the questions before sending it to the member surgeons. In addition, data were collected and descriptive statistics were analyzed. For data analysis, the Chi-square test was performed to compare the variables and P < 0.05 was considered statistically significant.

- Osteotomized femoral neck in the basicervical region.
Biomechanical study
Rotational stability was assessed using twenty, fourth-generation composite left proximal femurs (model number: SKU-3403, SawBones®) which were vertically osteotomized in the basicervical region (at an angle of 70°) to simulate an unstable basicervical femoral neck fracture [Figure 1]. All fractures were osteotomized and fixed using a mold to standardize fracture location and SHS placement. These fractures were anatomically reduced and held within a prefabricated mold to maintain the reduction and fracture compression. One of the four provisional fixation constructs was applied; Group 1: Single 7.3 mm derotation screw, Group 2: Two superior 2.0 mm K-wires, Group 3: One superior 2.0 mm K-wire, and Group 4: A TC-TA 2.0 mm K-wire transfixing into pelvic SawBone model potted in a stationary position [Figure 2]. An SHS guidewire was then inserted centrally in the femoral head and reamed and tapped to a tip apex distance of <20 mm. The SHS was then inserted with a torque limiter to the appropriate depth to maintain a uniform torque force during insertion for all specimens. All trials were performed by a single, fellowship-trained orthopedic trauma surgeon (MMZ). Rotational stability was assessed using an open-source software package developed by Jackson et al. to perform multi-camera 3D data acquisition using consumer-grade cameras (GoPro Hero 5, Medium FOV, 48 fps, 2.7 k).[7] This method was chosen over conventional systems such as Northern Digital Inc. This method was chosen over conventional optical tracking systems such as Polaris (Northern Digital Inc.) because it does not require heavy physical markers which were found to affect rotational stability during pilot testing. Using this technique, markers could be painted on the surface of the femur and tracked during SHS insertion.

- (a) One 2.0 mm K-wire and transcervical-transacetabular K-wire constructs. (b) Two superior 2.0 mm K-wire construct. (c) Single derotation screw construct.
Total rotation was determined by the final maximal angular rotation about the neck axis during insertion. For the femurs used, the total rotation was converted to a displacement based on the diameter of the basicervical region to approximate the total displacement seen at the fracture site. A sample size analysis determined that to achieve a power of 0.80 to detect a 1.9 mm difference in rotational stability, four samples were required per group. For data analysis, the one-way analysis of variance was performed to compare the variables, and P < 0.05 was considered statistically significant.
RESULTS
Web-based survey
One hundred and forty-two surgeons completed the survey. The mean years in the practice of respondents were 13.3 years. More than half of the surgeons (52.8%) described their practice as academic, while 38% had a community practice and 9.2% were in private practice. A trauma fellowship was completed by 58.5% of the respondents.
When asked about the type of fixation construct preferred for unstable basicervical femoral neck fractures, 50% preferred an SHS, 43.7% preferred a CMN, and 6.3% preferred other constructs (including cannulated screws, blade plate, and arthroplasty) [Figure 3]. A form of provisional fixation was applied to counteract the unstable pattern of these fractures by 79.6% of the responding surgeons. Interestingly, 35.5% of surgeons using a CMN do not routinely use any form of provisional fixation versus only 7% of surgeons applying an SHS construct (P < 0.001). Derotational screw (43.4%) and one superior K-wire (39.8%) were the most commonly used forms of provisional fixation [Figure 4]. More surgeons (47.8%) preferred to apply the provisional fixation before the final construct guidewire, while 41.6% preferred to start with the final construct guidewire before applying the provisional fixation and 9.7% had no specific preference [Figure 5].
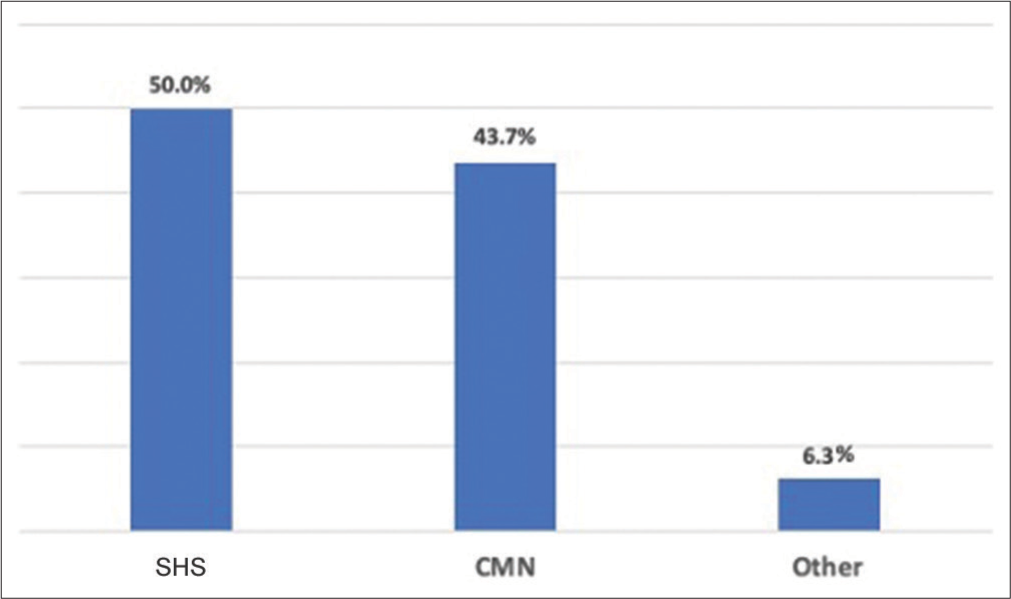
- Respondents type of preferred fixation for unstable basicervical femoral neck fractures.

- Respondents preferred method of provisional fixation for unstable basicervical femoral neck fractures.
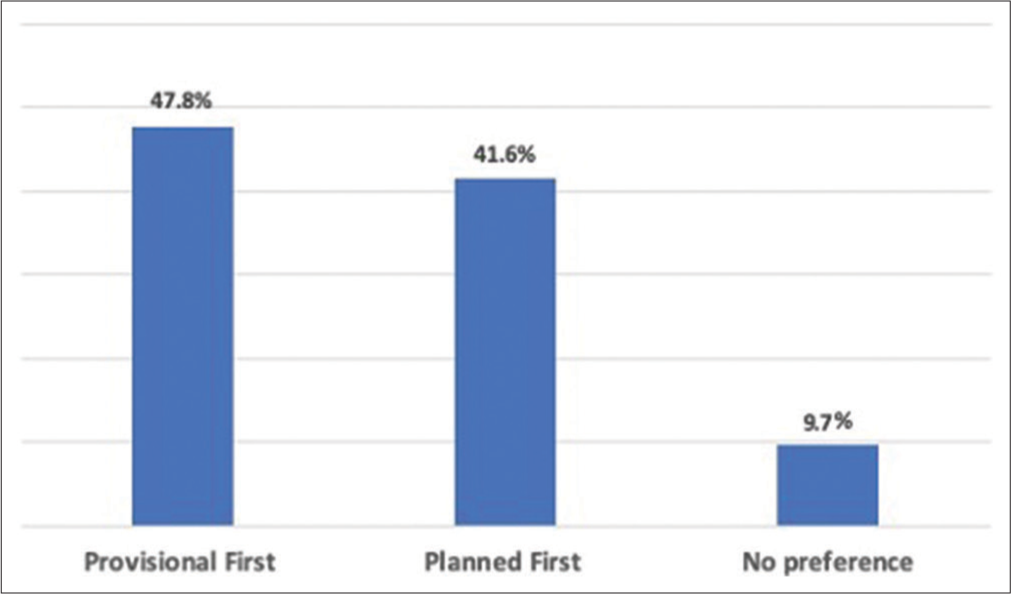
- Respondents preferred order of fixation for unstable basicervical femoral neck fractures.
The number of years in practice, type of practice, and completion of an orthopedic trauma fellowship were not significantly associated with the preferred fixation construct. On the other hand, we observed that surgeons in academic practice were more likely to apply a form of provisional fixation compared to other practices (P < 0.05).
Biomechanical study
Rotational stability was highest for the derotational screw group, followed by the two superior K-wires groups, then the TC-TA K-wire group, while the one superior K-wire group had the least stability [Table 1]. The derotational screw group showed significantly superior rotational stability when compared to the one superior K-wire (P < 0.05). Both the two superior K-wires and the TC-TA K-wire groups were more rotationally stable than the one superior K-wire group, but this did not reach statistical significance.
| Group construct | Rotational displacement (Mean±SD) (mm) |
|---|---|
| Derotational screw | 0.92±0.72 |
| Two superior K-wires | 1.57±1.06 |
| Transcervical-transacetabular K-wire | 1.86±1.19 |
| One superior K-wire | 3.09±1.37 |
In addition, the derotational screw group showed less rotational displacement compared to the two superior K-wires and TC-TA groups, but this also was not statistically significant. There was no significant difference in rotational displacement between the two superior K-wires and the TCTA groups.
DISCUSSION
More orthopedic surgeons in our survey preferred an SHS (50%) construct for the management of unstable basicervical femoral neck fractures, while a large number preferred a CMN (43.7%) construct for these fractures. In addition, a significantly larger number of participant surgeons that applied a CMN construct did not apply any form of provisional fixation compared to surgeons using an SHS construct. This can be attributed to the difficulty of applying a form of provisional fixation with a CMN (especially a derotational screw) unless a “Miss a nail” technique is applied. When a form of provisional fixation was applied, a derotational screw or a single superior K-wire was the most commonly used method.
Slobogean et al. showed in a survey of orthopedic surgeons, which included members of the OTA and COA, that for displaced young femoral neck fractures, a similar number of respondents preferred an SHS construct (49%) or a multiple screws construct (46%).[8] They also found that of the surgeons that preferred an SHS, 46.1% preferred to supplement it with a derotational screw. A similar study by Sciacca et al. explored the preferred fixation method of displaced femoral neck fractures in the young and old age groups by 52 surgeons at an international AO course.[9] They found that the majority of surgeons preferred screw fixation for the young patients and a form of arthroplasty for the older age groups. Luttrell et al. surveyed active OTA members regarding preferred constructs for vertically oriented femoral neck fractures.[10] Of the 272 respondents, 47% preferred an SHS with or without a derotational screw. We are not aware of any study that explored different types of preferred provisional fixation methods for unstable basicervical femoral neck fractures.
Biomechanically, we have shown that the derotational screw group offered significantly superior rotational stability at the time of SHS insertion compared to the single superior K-wire group. In addition, although the two superior K-wires and TC-TA K-wire groups had less rotational displacement compared to the single superior K-wire group, this did not reach statistical significance.
Multiple studies in the literature biomechanically compared different types of constructs used for the management of unstable basicervical femoral neck fractures. However, we are not aware of any study that explored the amount of displacement seen with different types of provisional fixations at the time of SHS insertion.[11-14]
Blair et al. biomechanically compared three fixation techniques (three parallel cannulated cancellous screws, SHS, and SHS with a derotational screw) in an osteoporotic cadaveric basicervical hip fracture model.[3] They found that the SHS construct outperformed the three cannulated screws construct in axial load, while there was no significant difference between the tested constructs in torsional and lateral bend testing. These results were reproduced in a biomechanical cadaveric study by Deneka et al., where SHS with a derotational screw demonstrated a higher average peak force and load to failure when compared to three cancellous screws when axial and torsional forces were applied.[15]
In a biomechanical synthetic femora model of Pauwels type III femoral neck fractures by Johnson et al., the SHS with a derotational screw was superior to both an inverted triangle and modified crossed cannulated screw construct when axially loaded.[16] In addition, Bonnaire et al. highlighted the significance of a derotational screw for the management of femoral neck fractures.[6] Their biomechanical cadaveric study showed less fracture gap formation when a derotational screw was added to the SHS construct compared to an SHS alone.
While we found that the derotational screw constructs supplied improved rotational stability during the SHS insertion, Blair et al. highlighted in their study that it does not provide any increased fixation after SHS insertion.[3] We tested the constructs using synthetic SawBone models, which eliminate the soft-tissue constrain, which may have a role in fracture stabilization. Unfortunately, we found no studies in the literature that compared K-wire provisional fixation to derotational screw fixation in a cadaveric model. This would be an excellent aspect to explore in future research directives.
This study has limitations, as is with any biomechanical study. The use of synthetic bone in our biomechanical testing may be considered a weakness, but we believe that cadaveric bone may introduce interspecimen variability, which is reduced with synthetic bone. In addition, the web-based survey was based on a questionnaire whose validity and reliability have not been established.
One strength of the study is that the biomechanical test methods were designed from the survey results and feedback. An additional strength of the study is that the amount of displacement was measured during the SHS insertion, which simulates the rotational force applied intraoperatively in these cases. Furthermore, the amount of torque applied to the specimens was kept from exceeding a maximum torque by applying a torque limiter to the SHS.
CONCLUSION
Our present study highlights that multiple provisional fixation methods are currently used to counteract the rotational instability of unstable basicervical femoral neck fractures. Biomechanically, we have shown that a single 7.3 mm derotational screw construct outperforms the single superior K-wire in rotational stability at the time of SHS screw insertions, which were the most commonly used methods by surgeons participating in our survey. However, more studies are required to assess these findings in different bone models and the amount of clinically relevant rotational displacement in these unstable fracture patterns.
ACKNOWLEDGMENT
We would like to thank the COA, OTA, and Saudi Orthopedic Association for their help with distributing the web-based survey to their surgeon members.
AUTHORS’ CONTRIBUTIONS
MMA: Concept, design, study execution, manuscript writing, and review. KC: Design, study execution, manuscript writing, and review. GPW, SRP, and ASL: Concept, design, manuscript writing, and review. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
ETHICAL APPROVAL
The authors confirm that this study had been prepared following COPE roles and regulations. Given the nature of the study and the fact that it did not include any patient-related data, the IRB review was not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate responders consent forms. In the form, the responders have given their consent for the images and other clinical information to be reported in the journal. The responders understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This survey did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
SUPPLEMENTAL FIGURE

- Web-based survey outline.
References
- World-wide projections for hip fracture. Osteoporos Int. 1997;7:407-13.
- [CrossRef] [PubMed] [Google Scholar]
- Basicervical versus intertrochanteric fractures: An analysis of radiographic and functional outcomes. Orthopedics. 2006;29:919-25.
- [CrossRef] [PubMed] [Google Scholar]
- Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop Relat Res. 1994;306:256-63.
- [Google Scholar]
- Internal fixation of femoral neck fractures. J Am Acad Orthop Surg. 2006;14:565-71.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction techniques for young femoral neck fractures. J Orthop Trauma. 2019;33(Suppl 1):S12-9.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of fracture gap changes, dynamic and static stability of different osteosynthetic procedures in the femoral neck. Injury. 2002;33(Suppl 3):C24-32.
- [CrossRef] [Google Scholar]
- 3D for the people: Multi-camera motion capture in the field with consumer-grade cameras and open-source software. Biol Open. 2016;5:1334-42.
- [CrossRef] [PubMed] [Google Scholar]
- Management of young femoral neck fractures: Is there a consensus? Injury. 2015;46:435-40.
- [CrossRef] [PubMed] [Google Scholar]
- Variations of treatment in selected proximal femur fractures among surgeons with a different surgical experience-a survey at an international AO course. Injury. 2015;46(Suppl 6):S57-60.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative decision making in the treatment of high-angle “vertical” femoral neck fractures in young adult patients, An expert opinion survey of the orthopedic trauma association's (OTA) membership. J Orthop Trauma. 2014;28:e221-5.
- [CrossRef] [PubMed] [Google Scholar]
- Vertically oriented femoral neck fractures: Mechanical analysis of four fixation techniques. J Orthop Trauma. 2007;21:544-8.
- [CrossRef] [PubMed] [Google Scholar]
- A biomechanical comparison of two triple-screw methods for femoral neck fracture fixation in a synthetic bone model. J Trauma. 2010;69:1537-44.
- [CrossRef] [PubMed] [Google Scholar]
- Results of cephallomedullary nail fixation for displaced intracapsular femoral neck fractures. J Orthop Trauma. 2011;25:714-20.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanical comparison of a dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir Orthop Traumatol Cech. 2015;82:140-4.
- [Google Scholar]
- Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures. J Orthop Trauma. 1997;11:337-43.
- [CrossRef] [PubMed] [Google Scholar]
- Vertically oriented femoral neck fractures: A biomechanical comparison of 3 fixation constructs. J Orthop Trauma. 2017;31:363-8.
- [CrossRef] [PubMed] [Google Scholar]






