Translate this page into:
Radial and ulnar nerve palsies in closed humerus fracture: A case report and literature review
*Corresponding author: Ibrahim S. Alshaygy, MD. MHSc., Department of Orthopedic Surgery, King Khalid University Hospital, Riyadh, Saudi Arabia. ialshaygy@ksu.edu.sa
-
Received: ,
Accepted: ,
How to cite this article: Alshaygy I, Altwaijri N, Alageel M, Alharbi S, Alabdali A, Alsuwaine B. Radial and ulnar nerve palsies in closed humerus fracture: A case report and literature review. J Musculoskelet Surg Res 2023;7:298-301.
Abstract
Fractures of the humeral shaft are commonly associated with radial nerve injury because of the anatomical course of the nerve. An ulnar nerve injury is rarely associated with such fractures. We present a case of a humeral shaft fracture with combined radial and ulnar nerve injuries in a female adult patient. The patient subsequently underwent radial and ulnar nerve exploration with internal fixation of the left humerus. According to our literature review, no similar cases were previously reported.
Keywords
Fracture
Humerus
Radial Nerve
Trauma
Ulnar nerve
INTRODUCTION
Humerus shaft fractures account for 1–5% of fractures.[1] These injuries occur most commonly due to traumatic events, such as falls or motor vehicle accidents.[2] The most injured peripheral nerve is the radial nerve in long bone fractures.[3] Given the radial nerve’s location near the humerus’ periosteum and its length within the arm, radial nerve injury is frequently associated with midshaft humeral fractures.[4]
Radial nerve injury occurs in around 18% of closed distal or midshaft humerus fractures. In open fractures, the laceration incidence of the radial nerve is 60%, whereas in closed fractures, the injury is more likely to be incomplete neuropraxia.[5]
Injuries to the ulnar nerve are divided into low or high, with high injuries happening close or proximal to the flexor carpi ulnaris motor branch.[6] Most patients with ulnar nerve injury lose finger adduction and abduction and develop intrinsic muscle dysfunction, counting claw hand deformity, and reduced pinch and grip strength.[7]
This report presents a rare and unusual case of a combined radial and ulnar nerve injury in a closed humeral shaft fracture. To the best of our knowledge, no patient presenting with the same injury has been described in the literature. We believe reporting this case can add to the literature, aid in managing similar cases, and stress the importance of complete clinical examination even after discovering one injury to avoid missing another concurrent injury.
CASE REPORT
A 32-year-old female, medically and surgically free, was brought by ambulance to the emergency department after a hit-and-run road traffic accident where she was thrown approximately 4 m. On her arrival, primary and secondary surveys were carried out by the trauma surgery team. She started developing a seizure and was intubated. Chest and pelvis radiographs showed no significant findings, but the left humerus radiographic examination showed a distal shaft fracture [Figure 1]. Proper physical examination, including peripheral neurological examination, could not be properly carried out at the time due to the patient’s condition.

- Radiograph after the trauma event. Showing a mid shaft humerus fracture.
The patient was found to have ecchymosis and swelling over the posterolateral aspect of the left arm with obvious deformity. Her distal pulses were palpable. Realignment and splinting were done. The left arm radiograph was repeated [Figure 2a and b], and distal pulses were palpable. The patient then underwent a trauma computed tomography scan, which revealed an anterior forehead subgaleal hematoma, a linear nondisplaced fracture of the left transverse process of T1, bilateral dependent atelectasis, L2 right transverse process undisplaced fracture, L5 left transverse process undisplaced fracture, and contusions around the left kidney. After that, admission under the care of the surgical intensive care unit for monitoring was done. Five days later, the patient was extubated and off sedation, and her neurological status was then examined. She was found to have a loss of thumb and wrist extension with complete wrist drop, indicating a radial nerve injury, and loss of finger adduction, indicating an ulnar nerve injury.
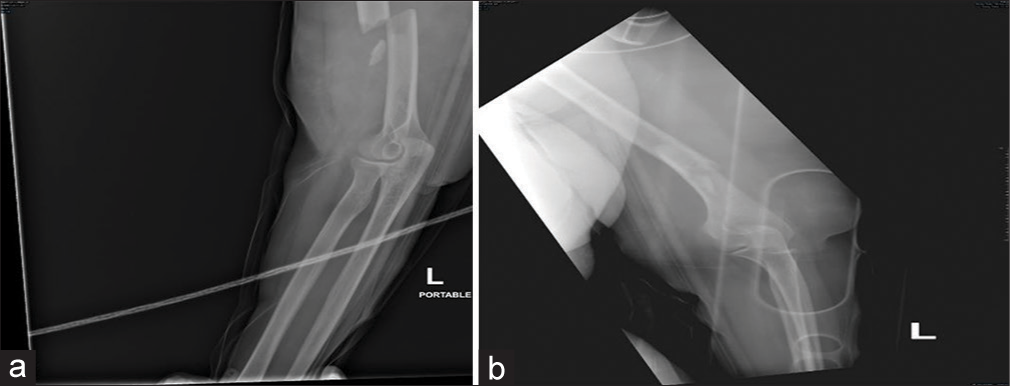
- (a and b) radiograph after realignment and applying the U-shape back slab.
Moreover, the patient suffered a complete loss of sensation over radial and ulnar nerve distribution. After counseling, the patient opted for surgical management. The patient was then taken to the operating room; while under general anesthesia, the patient was put in a lateral position with arm support and complete padding of dependent areas. A direct posterior universal incision with a triceps-sparing approach was chosen. A subcutaneous degloving injury measuring around 10 cm was found during the surgical approach. On exploration, the ulnar and radial nerves were found to be contused but in continuity. Both nerves were protected with vessel loops [Figure 3], and fracture fixation was performed using a 4.5-mm narrow dynamic compression plate [Figure 4a and b]. The patient was placed in a cock-up splint for 6 weeks and was sent for physical therapy.
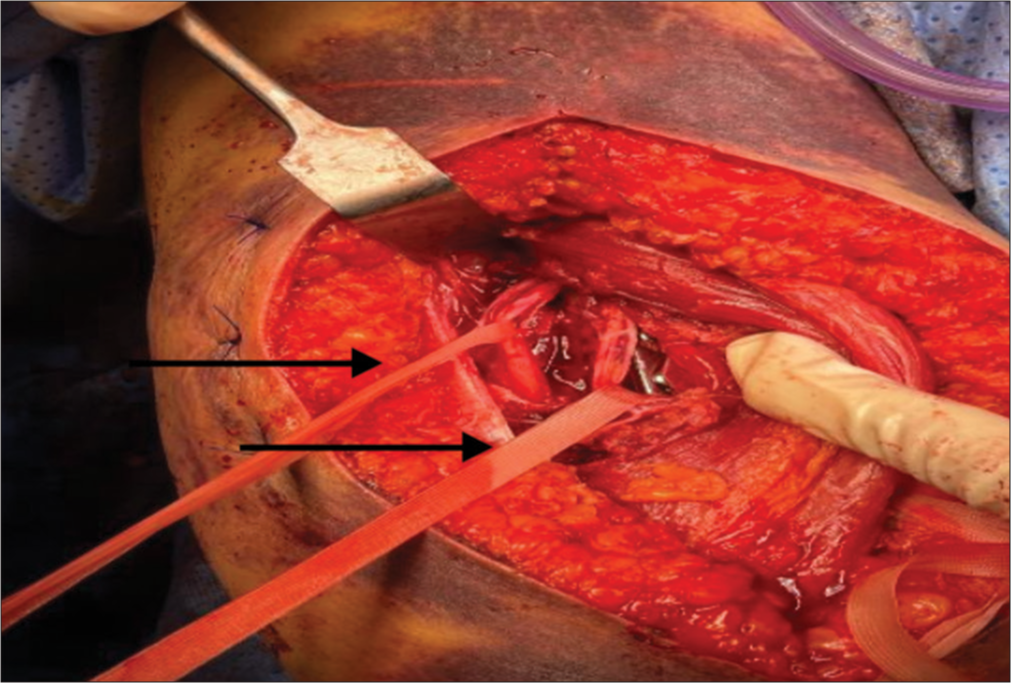
- Vessel loops around the radial nerve branches after fixation of the fracture. Vessel loops are pointed at by the arrows.
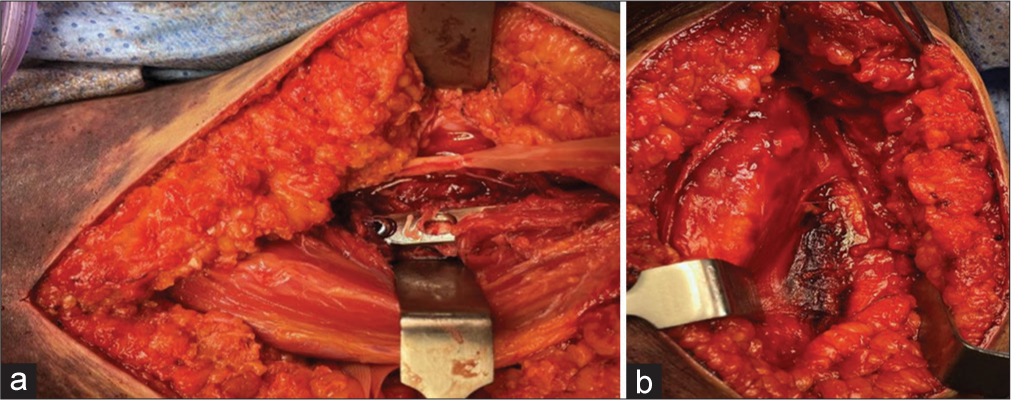
- (a) Intraoperative picture showing plate insertion, (b) Intraoperative picture showing the fracture of the humerus.
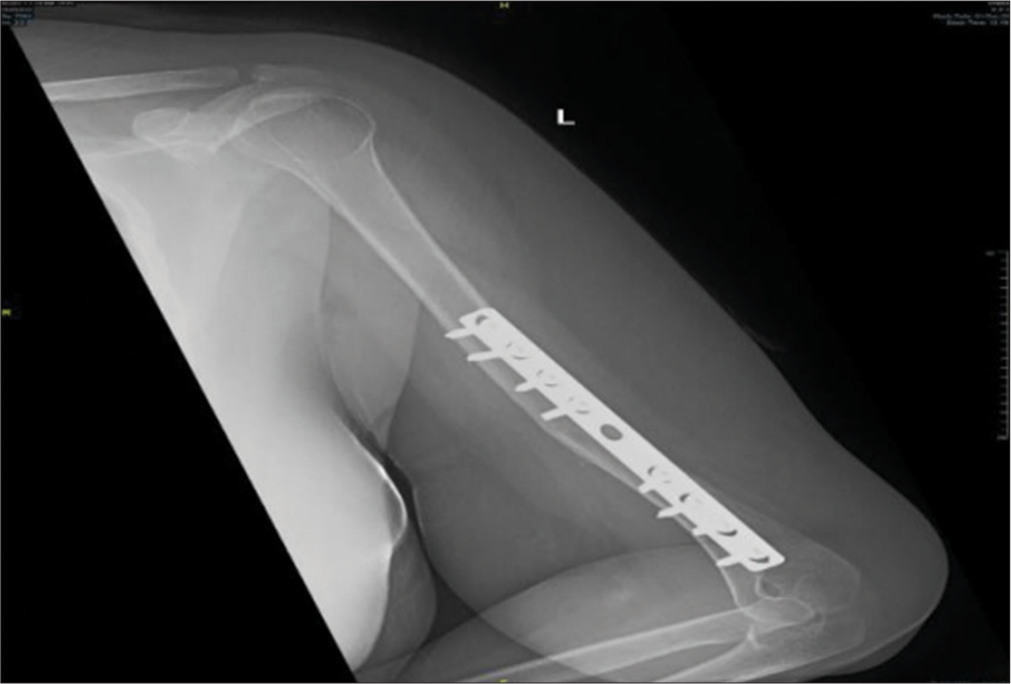
At the 4-month follow-up, gradual recovery occurred in the ulnar nerve, showing improved sensation and finger adduction, but radial nerve function did not improve. At this point, electromyography was arranged for the patient. The results indicated electrophysiological evidence of nonlocalizable, chronic, mild left radial neuropathy (mild neuropraxia/axonotmesis) with no evidence of active/ongoing denervation. At the 6-month follow-up, she was noted to have complete recovery of radial and ulnar nerve function. She was then discharged from the clinic, given her fracture union and return of baseline function [Figure 5a and b].
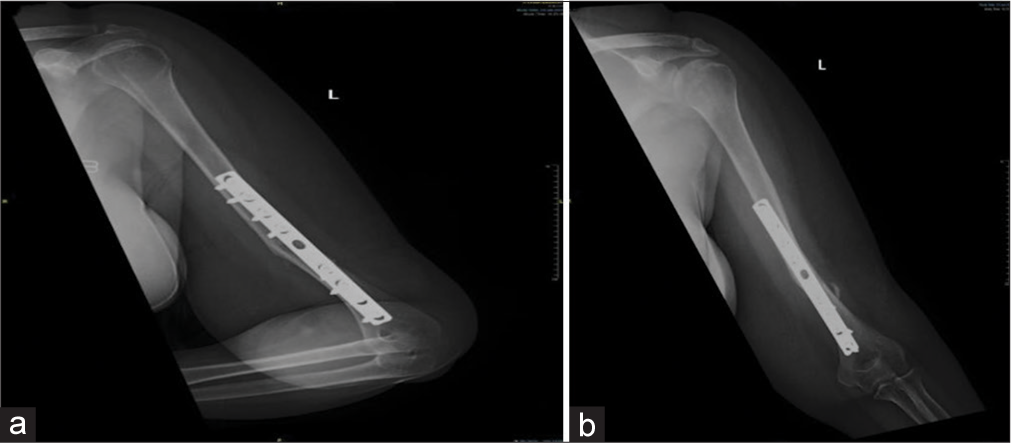
- (a and b) Post-operative radiograph.
DISCUSSION
Fractures of the humerus shaft fractures usually occur during high-velocity trauma, with the radial nerve being the most likely peripheral nerve to be injured.[8] The standard of care for humeral shaft fractures is non-surgical treatment.[9] Radial nerve palsy is not an absolute indication for surgical management given that radial nerve injuries in the setting of fractures of the humeral shaft are expected to recover spontaneously in more than 70% of cases; complete recovery is expected in around 90% of cases, including those that undergo procedural intervention.[10] Stahl et al [11] described the first case of palsy of the ulnar nerve after a humeral shaft spiral fracture. In our case, the injury of the ulnar nerve was due to contusion from blunt trauma, in contrast to other studies where Stahl et al found the ulnar nerve transected and repaired intraoperatively[11] and Pathak et al found a piece of bone abutting the ulnar nerve and penetrating the bone.[12] In our patient, radial and ulnar nerve palsies manifested as complete wrist drop, loss of finger adduction, and sensory disturbance along the distribution of both nerves. During the post-operative course and clinic follow-up, both nerves recovered gradually. An electromyogram study at 4 months showed evidence of non-localizable chronic mild left radial neuropathy (mild neuropraxia/axonotmesis) with no evidence of active or ongoing denervation. No electrophysiological evidence of ulnar neuropathy was found. At the patient’s 6-month follow-up, there was complete recovery of the radial and ulnar nerves with fracture union [Figure 6]. The radial nerve injury is commonly linked with a closed, simple humerus shaft fracture, especially when the injury is to the distal shaft. Ulnar nerve injury is found almost exclusively with severely comminuted or open humerus shaft fractures due to a penetrating/laceration injury. In our case, the fracture pattern was less likely to be concomitant with ulnar nerve palsy. Therefore, the presence of ulnar nerve palsy was an exceptional finding and necessitated a thorough examination of all peripheral nerves to avoid missing any injuries to the nerves.
- Radiograph at 6 months after surgery.
CONCLUSION
This case accentuates the importance of vigilant neurological examination of all peripheral nerves in the upper limbs in patients with a humerus fracture, regardless of the severity, and pattern of the fracture. Any nerve injury can substantially impact a patient’s quality of life, necessitating a thorough evaluation of every patient presenting with an injury to their extremities. Thus, physicians must orient themselves to all possible anatomical variants of the nerves. To deliver high-quality care, physicians must approach, impact injuries caused by high-velocity traffic accidents with great care and knowledge of possible nerve injuries.
AUTHORS’ CONTRIBUTIONS
NA has written the first and final drafts. IS reviewed the manuscript and prepared the case. AA reviewed the final draft of the manuscript. SA has reviewed the manuscript and oversaw the writing process. BA reviewed the final draft of the manuscript. MA wrote the first draft and helped review the manuscript’s final draft. All authors have critically reviewed and approved the final draft and are responsible for the manuscript’s content and similarity index.
USE OF ARTIFICIAL INTELLIGENCE (AI)-ASSISTED TECHNOLOGY FOR MANUSCRIPT PREPARATION
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
DECLARATION OF PATIENT CONSENT
The authors certify that they have obtained all appropriate patients consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
CONFLICTS OF INTEREST
There are no conflicting relationships or activities.
FINANCIAL SUPPORT AND SPONSORSHIP
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Incidence and characteristics of humeral shaft fractures after subpectoral biceps tenodesis. Orthop J Sports Med. 2019;7:2325967119833420.
- [CrossRef] [PubMed] [Google Scholar]
- Approach to radial nerve palsy caused by humerus shaft fracture: Is primary exploration necessary? Injury. 2013;44:323-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of humeral shaft fractures related to associated injuries. A retrospective study of 237 patients. Acta Orthop Scand. 1991;62:148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Tendon transfers for radial, median, and ulnar nerve injuries: Current surgical techniques. Clin Plast Surg. 2011;38:621-42.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis of traumatic ulnar nerve injuries: A systematic review. Ann Plast Surg. 2019;82(Suppl 1):S45-52.
- [CrossRef] [PubMed] [Google Scholar]
- Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. J Bone Joint Surg Br. 2005;87:1647-52.
- [CrossRef] [PubMed] [Google Scholar]
- Humeral shaft fractures In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- Epidemiology of humerus fractures in the United States: Nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 2012;64:407-14.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar nerve palsy following fracture of the shaft of the humerus. J Orthop Trauma. 1998;12:363-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar nerve injury after a comminuted fracture of the humeral shaft from a high-velocity accident: A case report. J Med Case Rep. 2012;6:192.
- [CrossRef] [PubMed] [Google Scholar]






